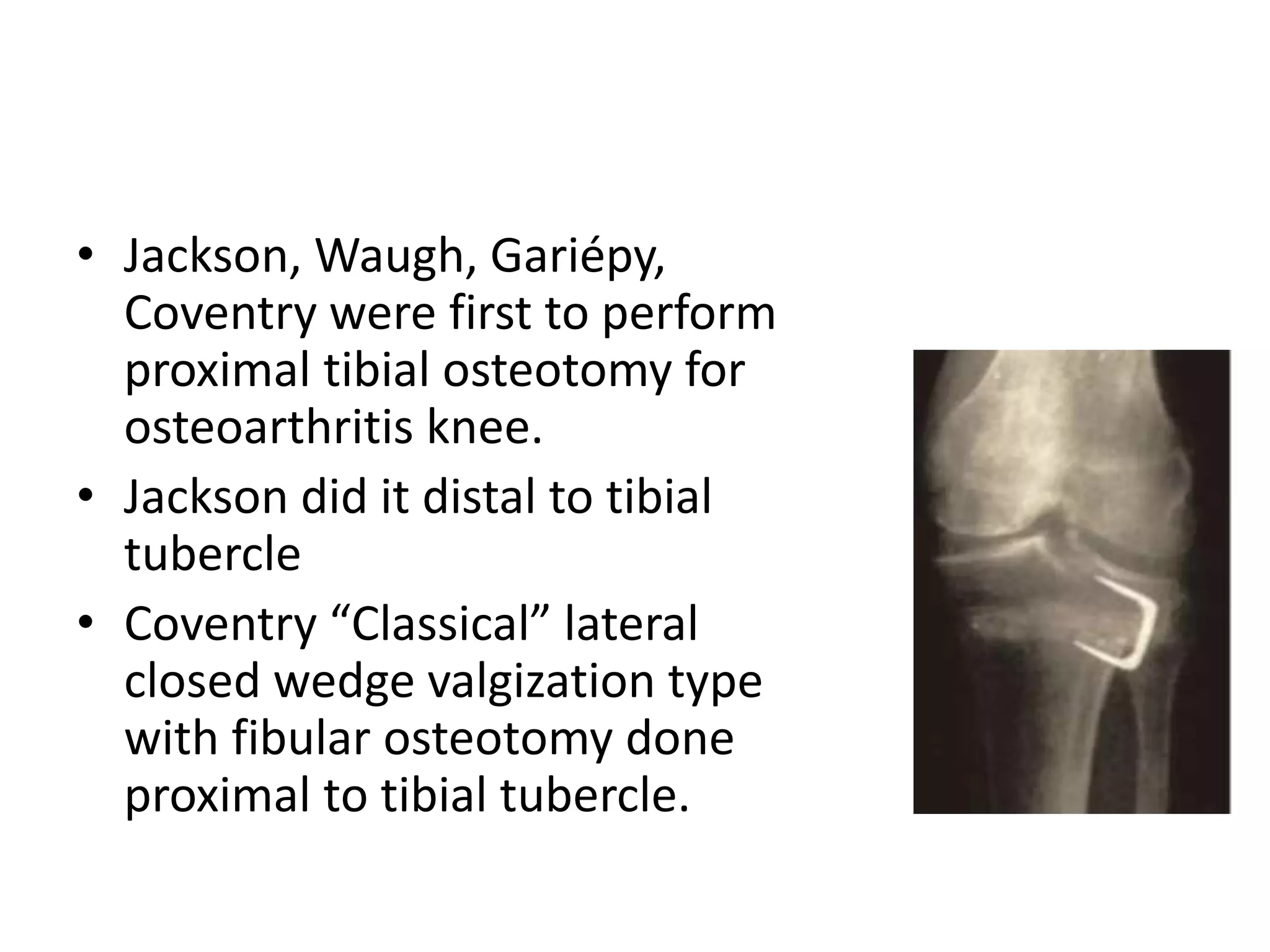
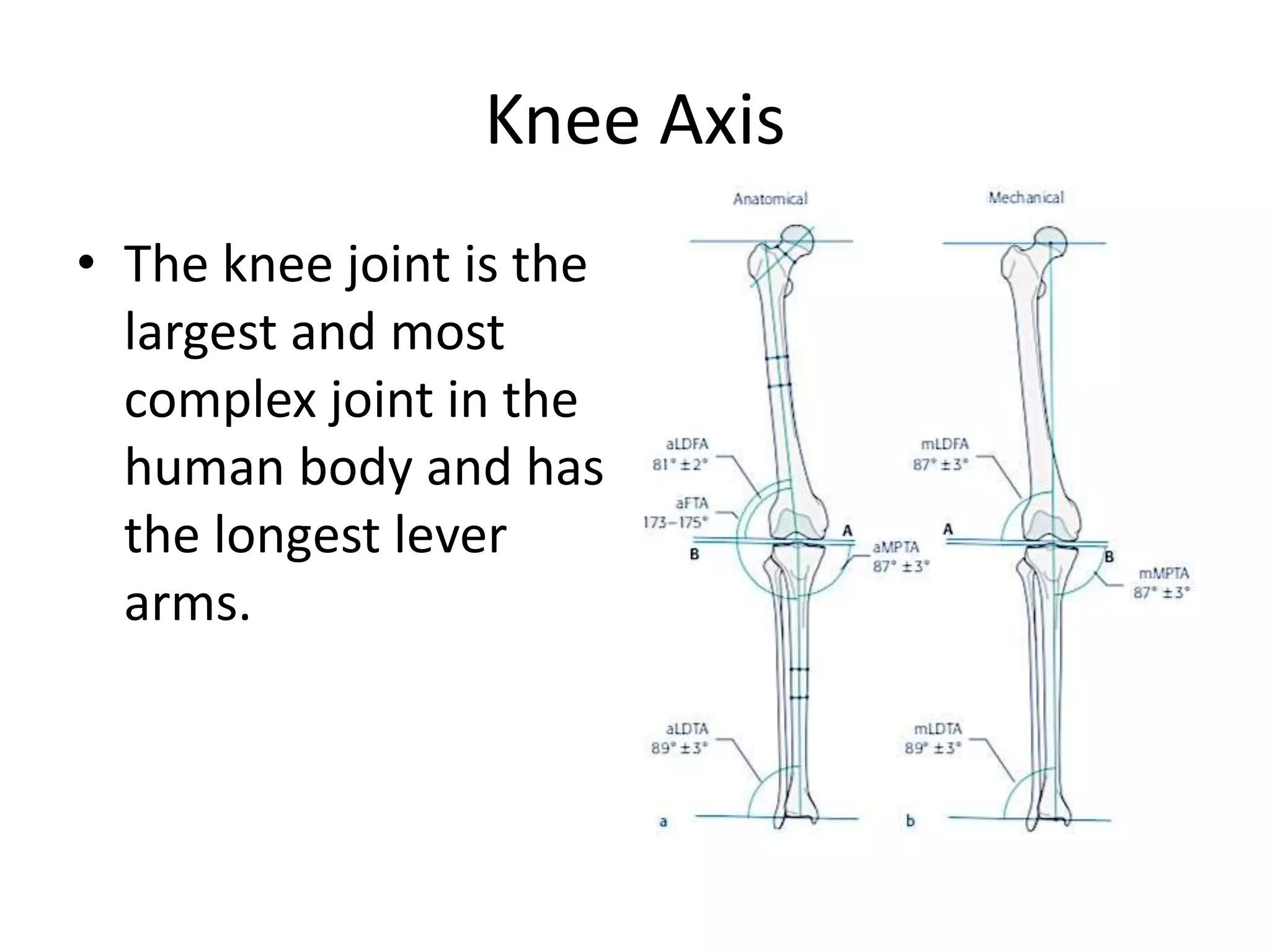
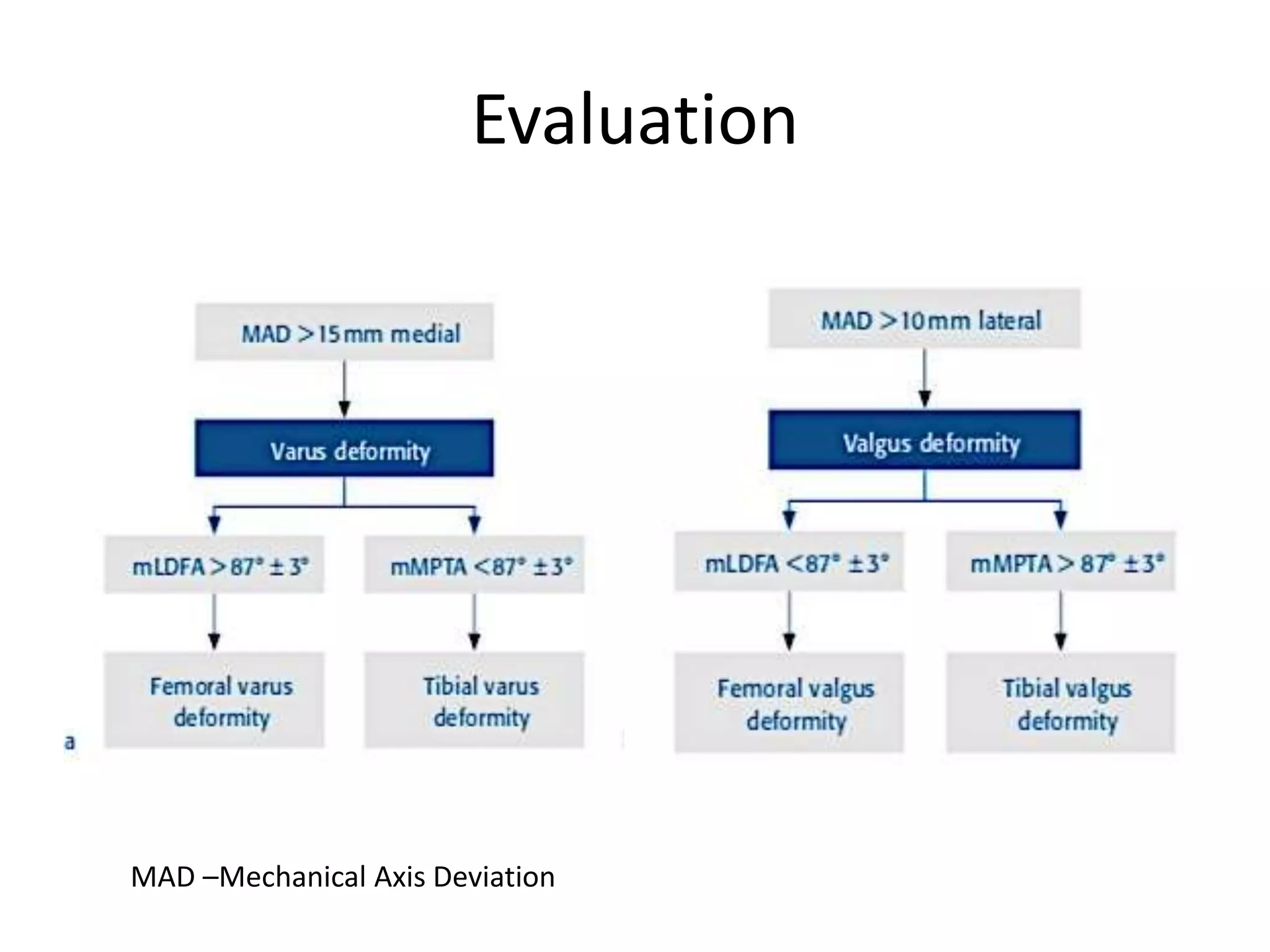
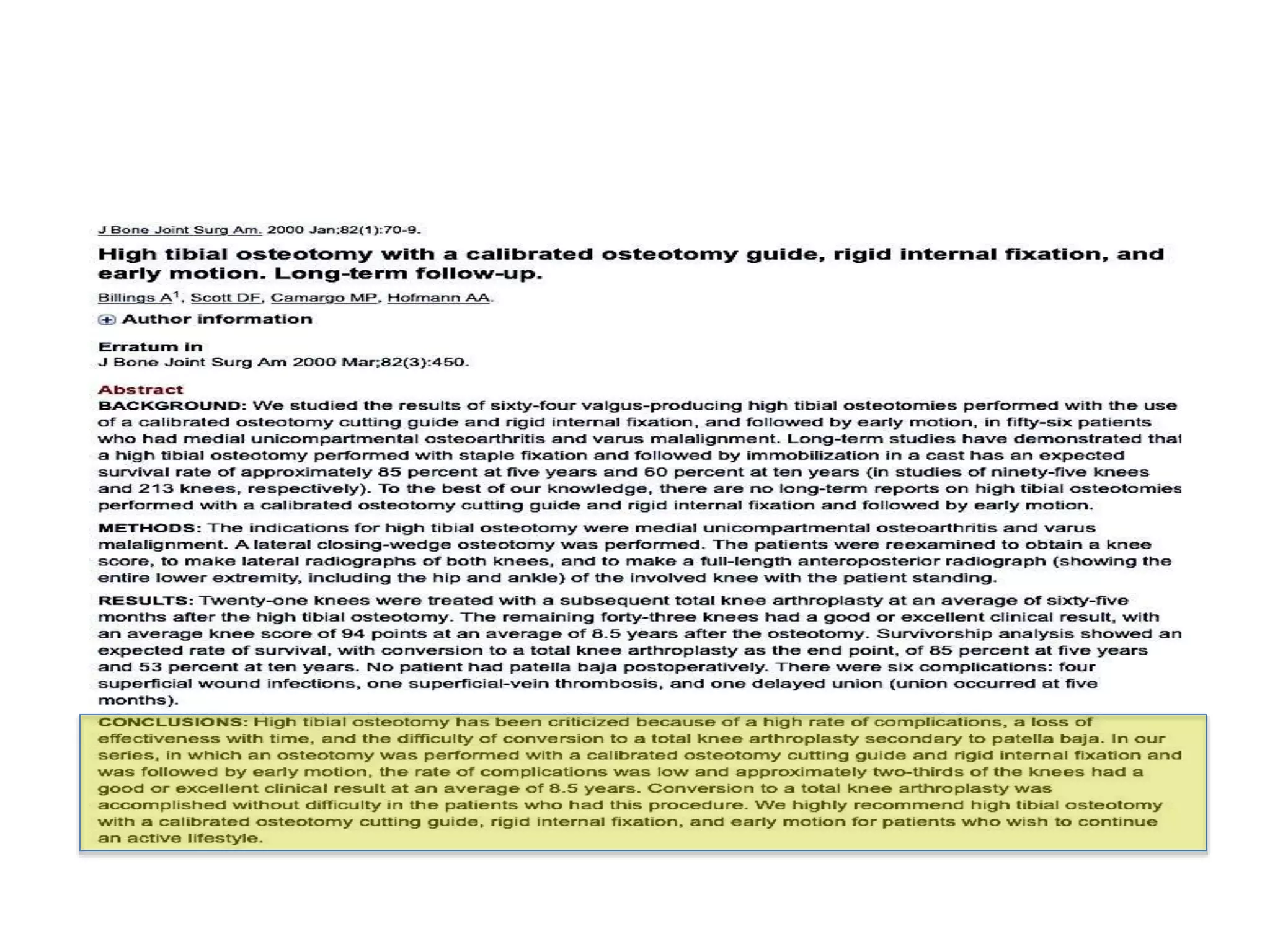
1) The document discusses the planning of a high tibial osteotomy (HTO) procedure, including a brief history of osteotomies, knee axis anatomy, indications for HTO, preoperative planning considerations, and techniques for planning correction angles and wedge sizes.
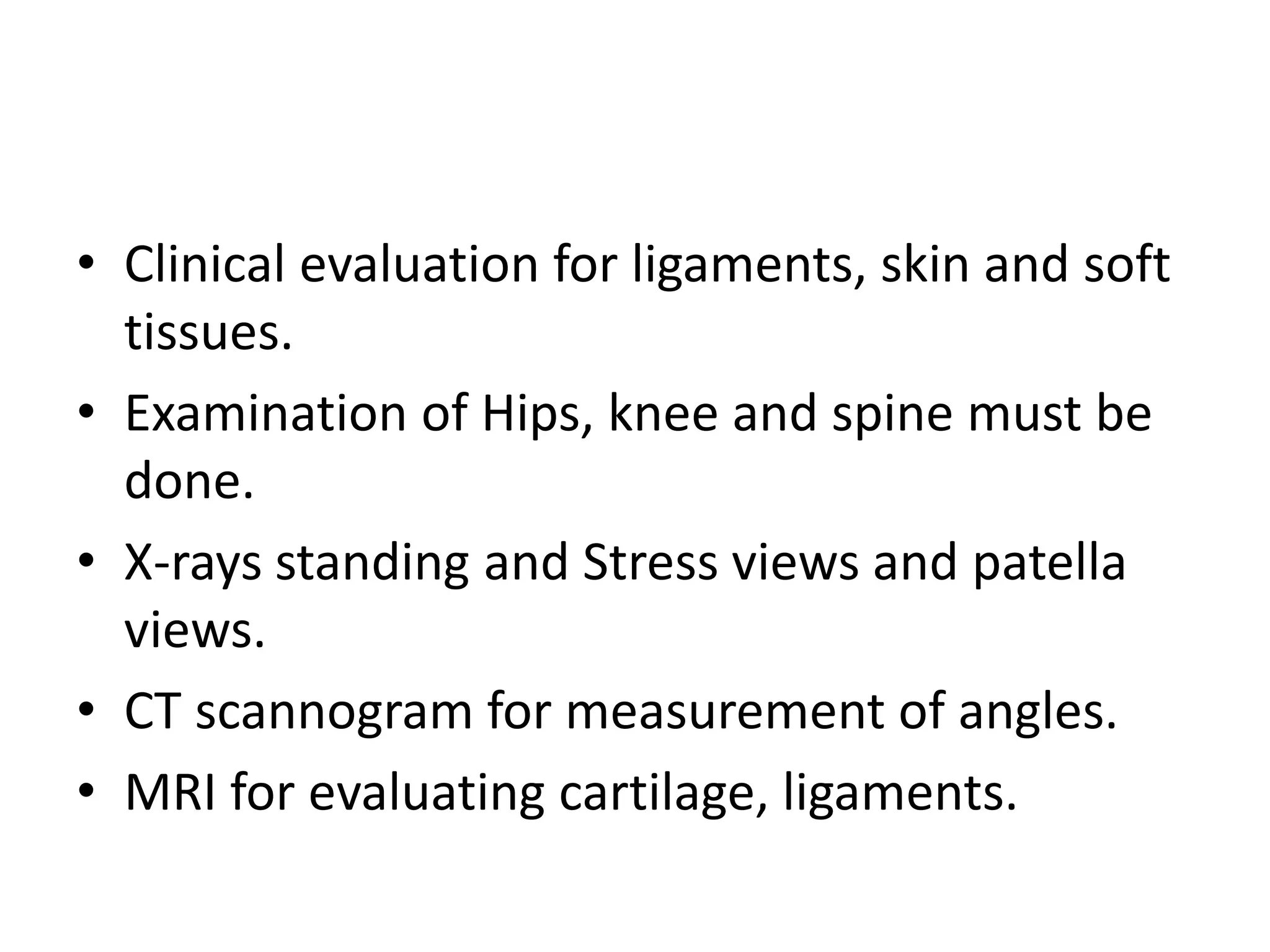
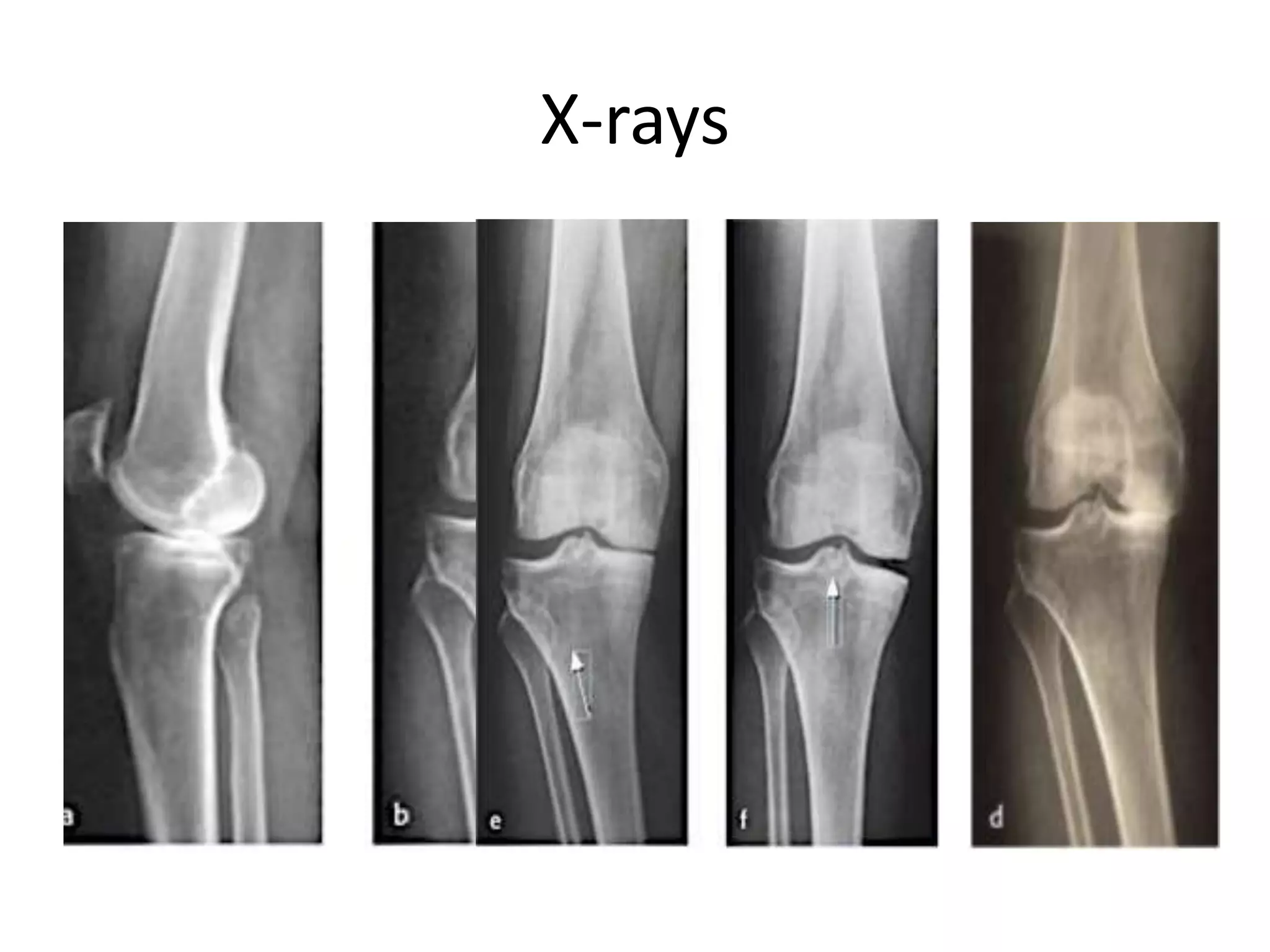
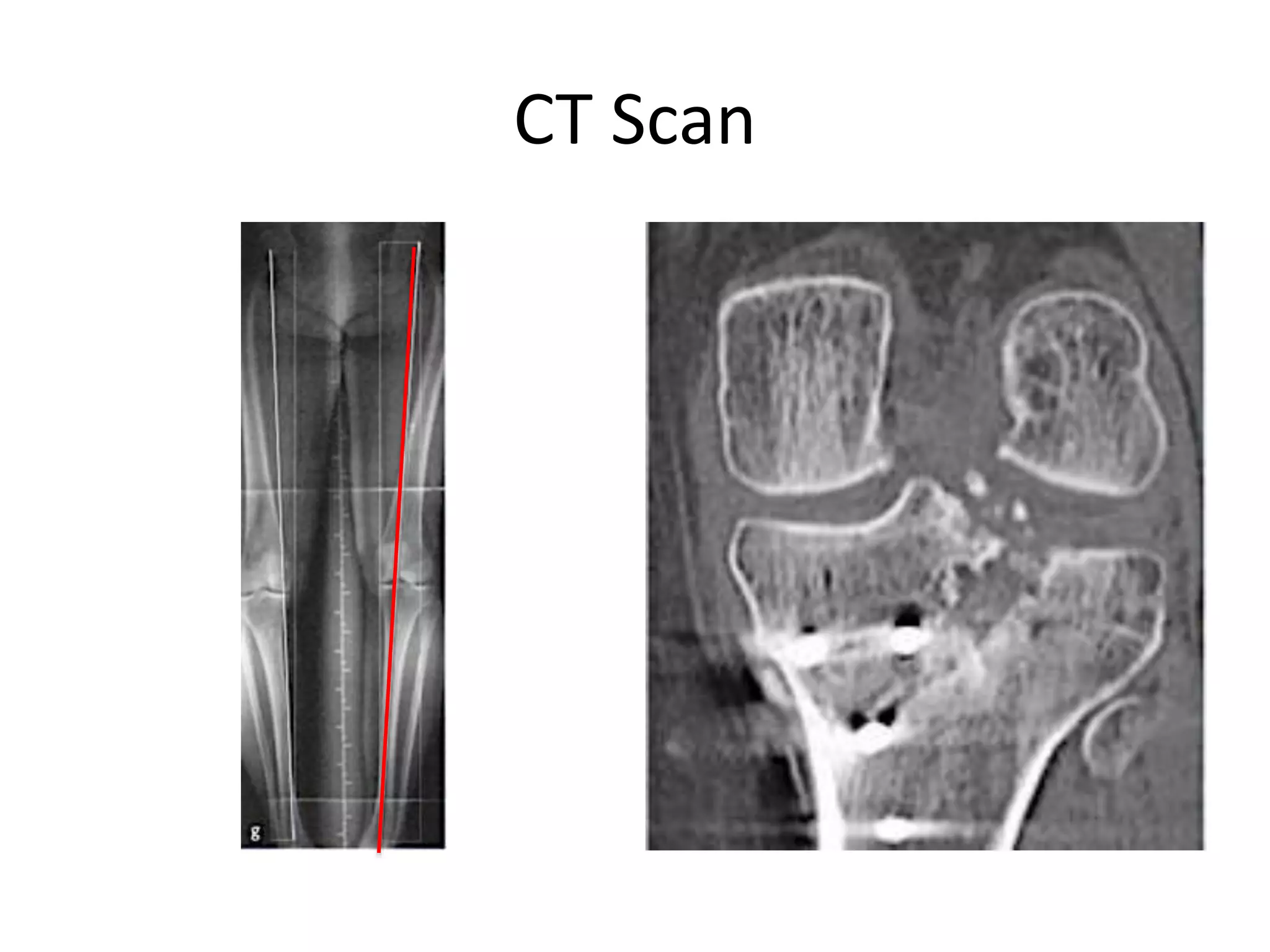
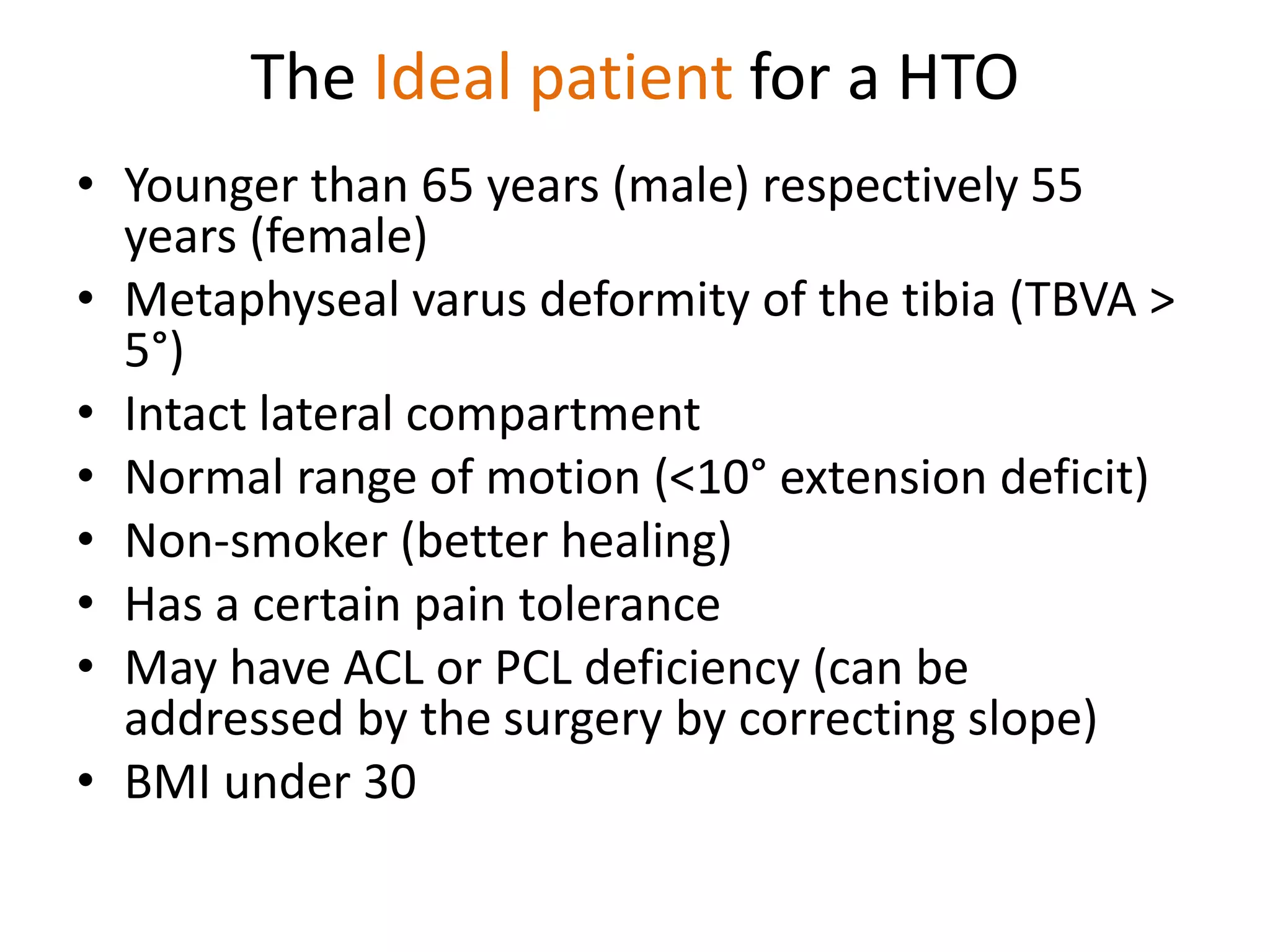
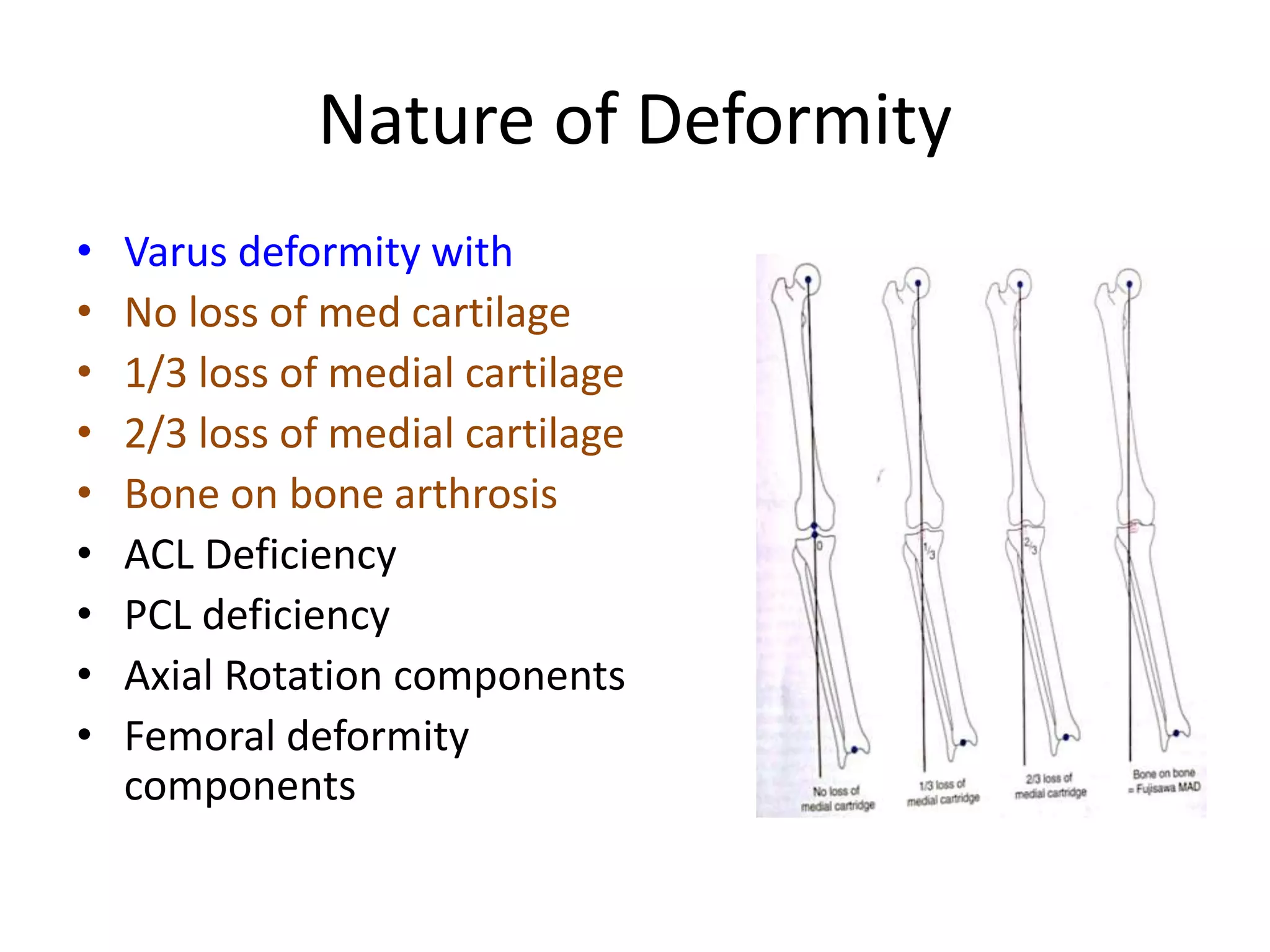
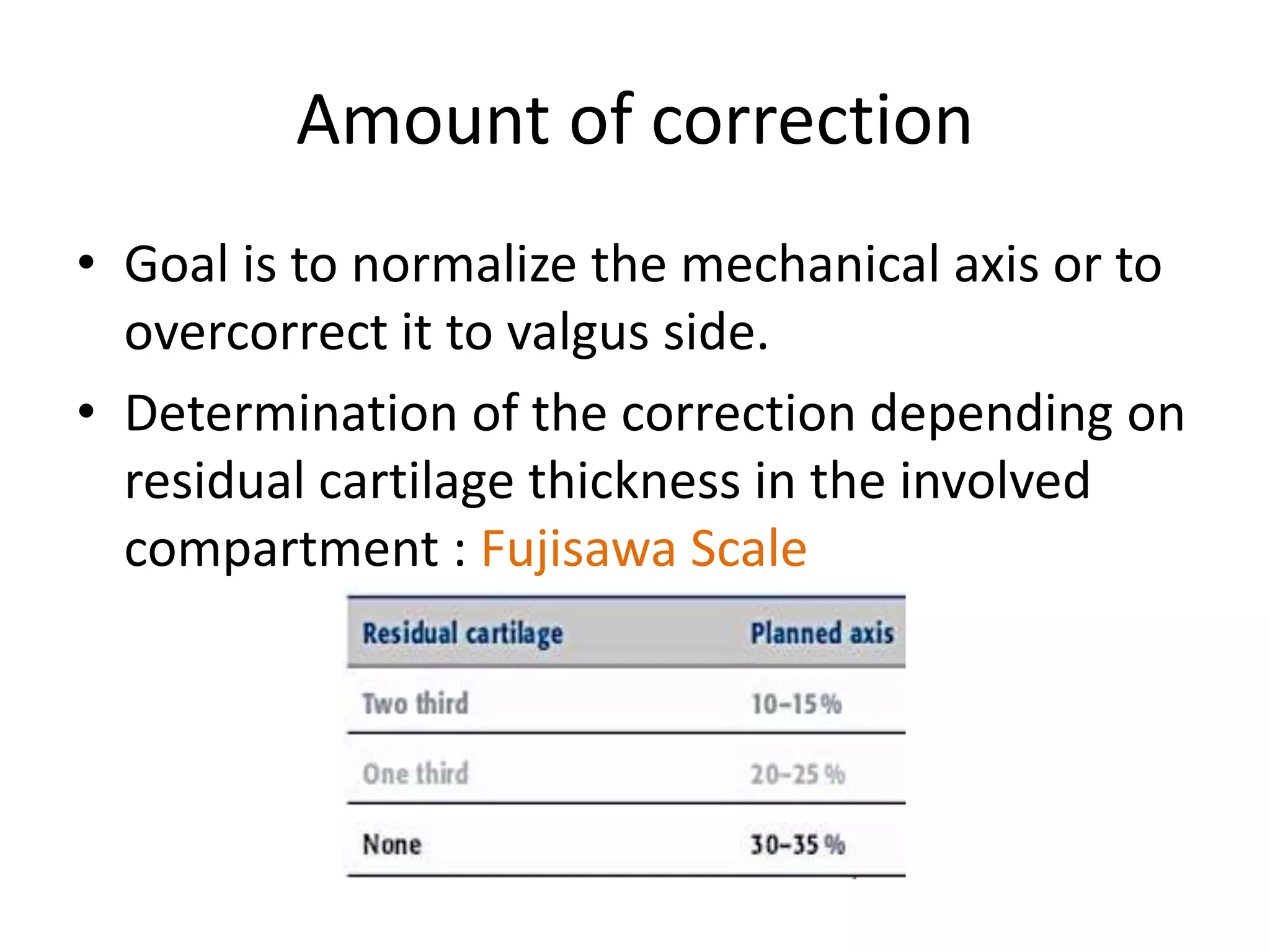
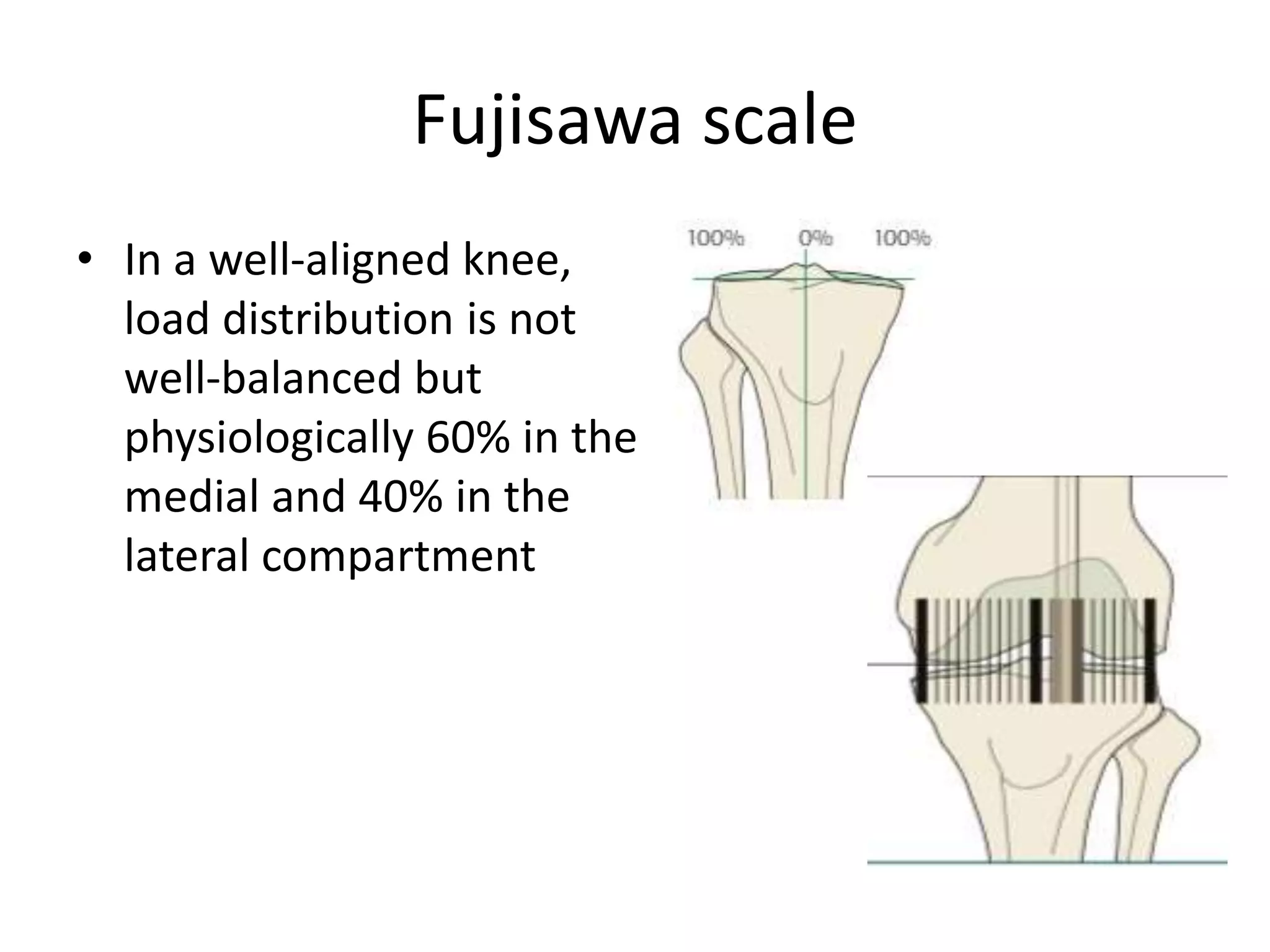
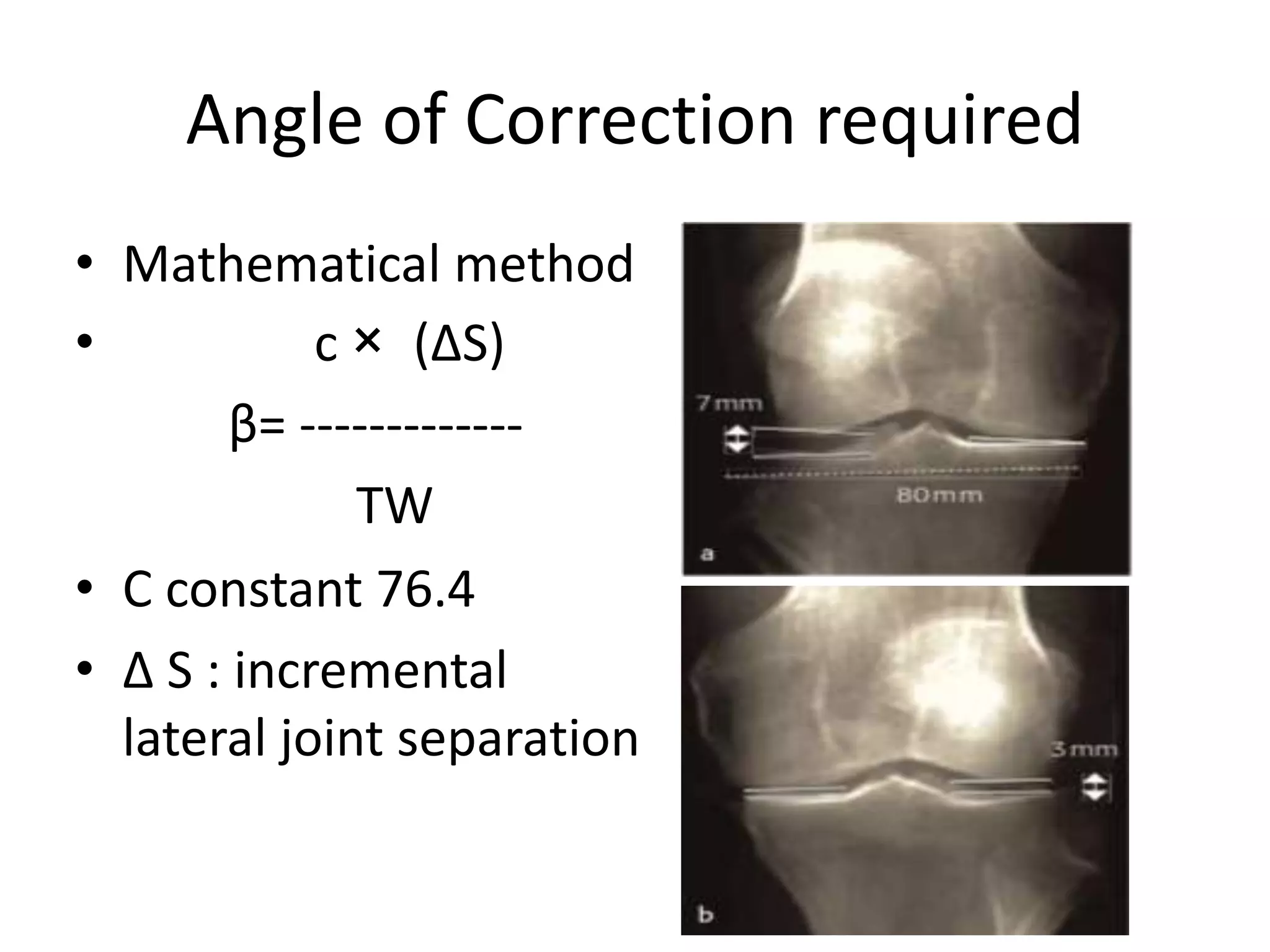
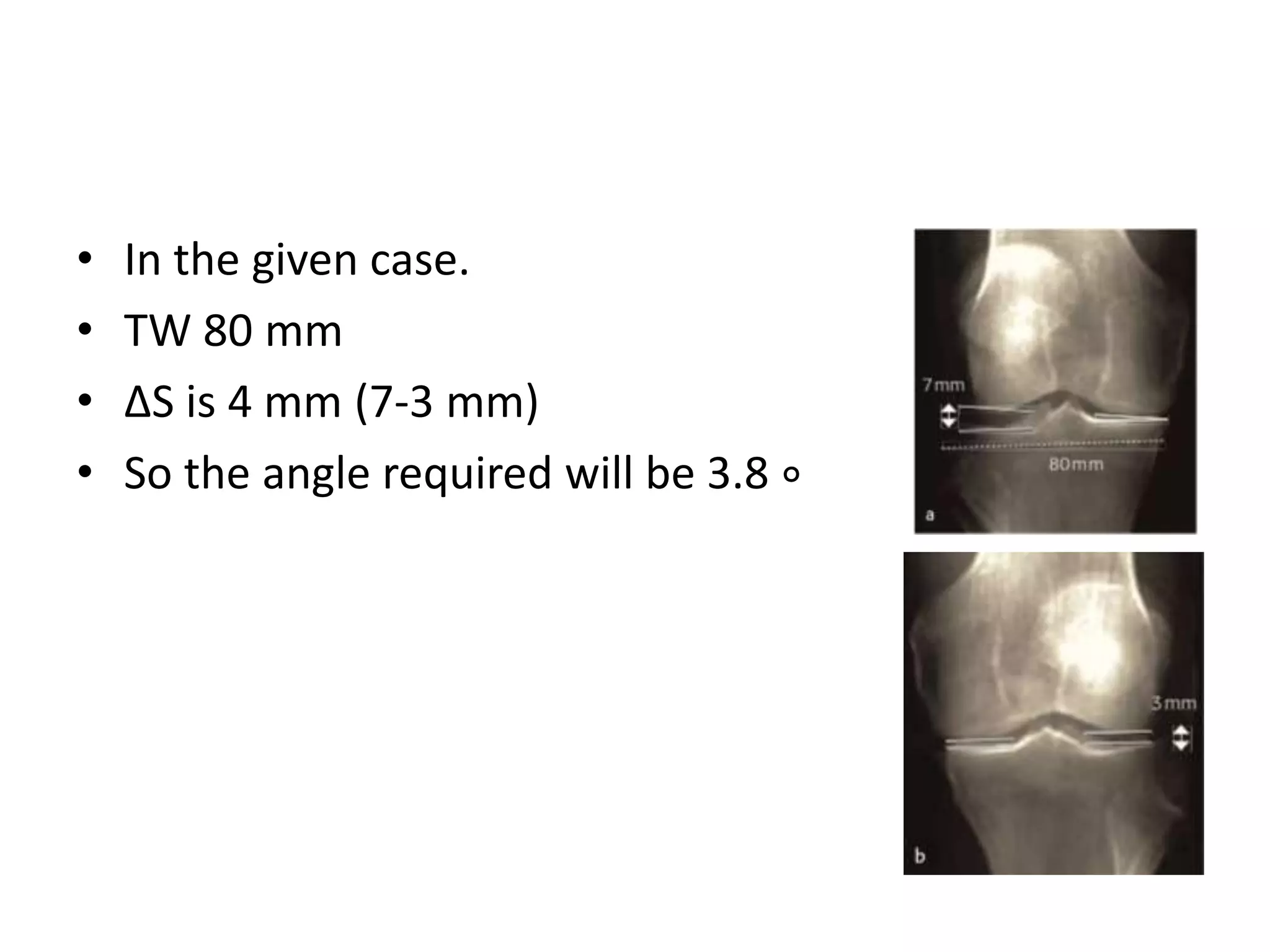
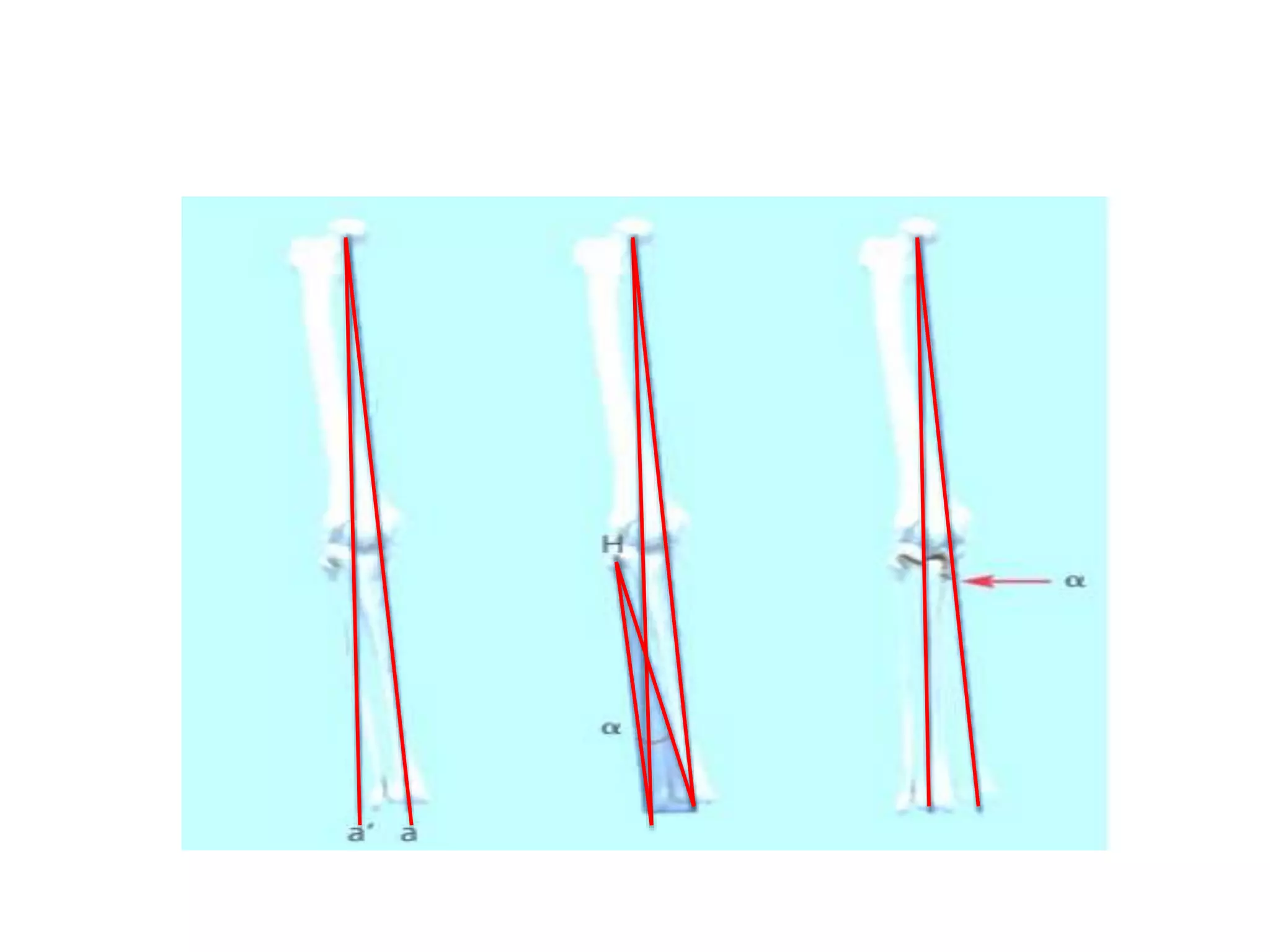
2) Key factors in planning include determining the nature and location of deformity, ideal candidates for HTO vs other procedures, and calculating the needed correction angle based on methods like the Fujisawa scale.
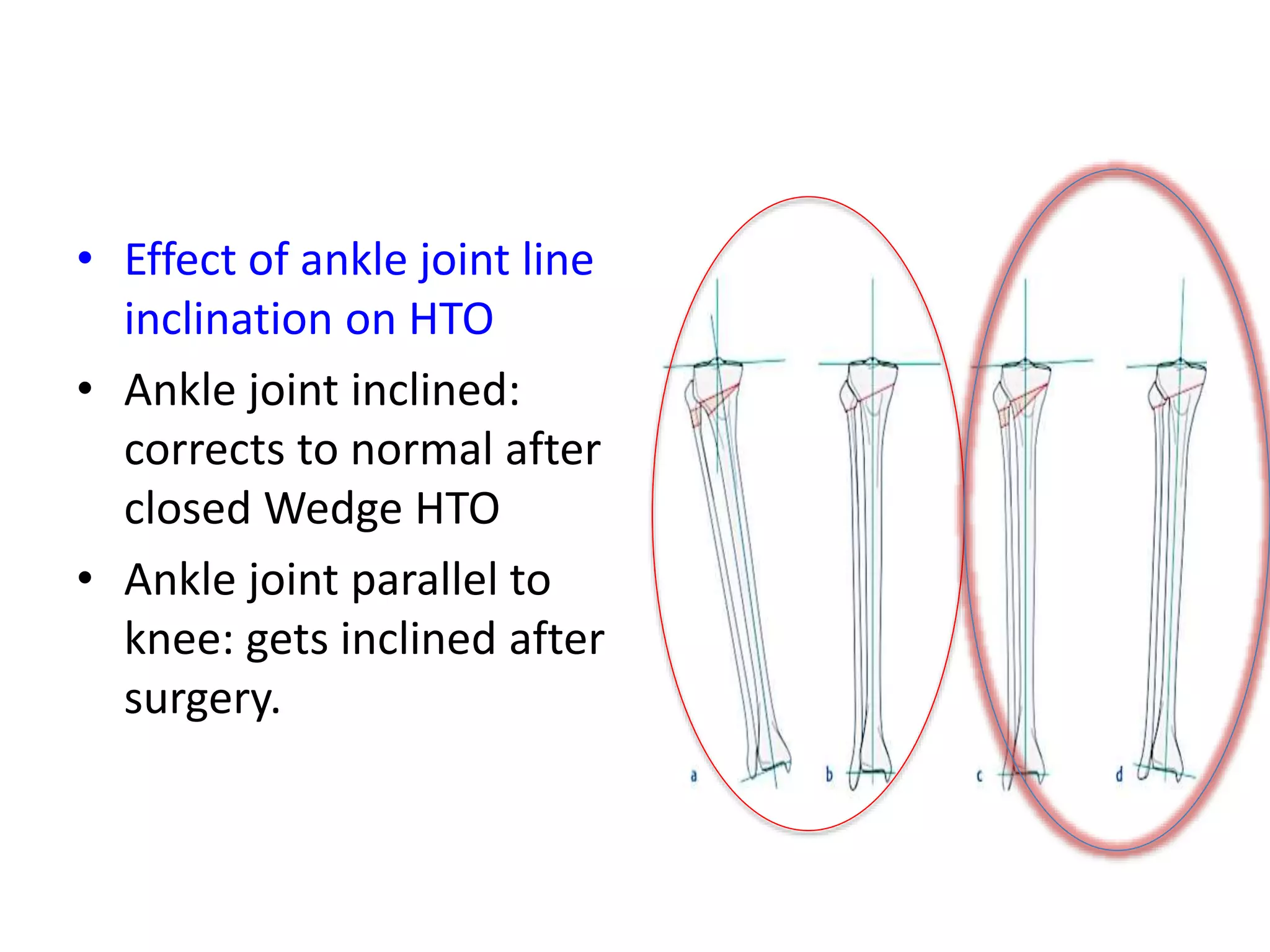
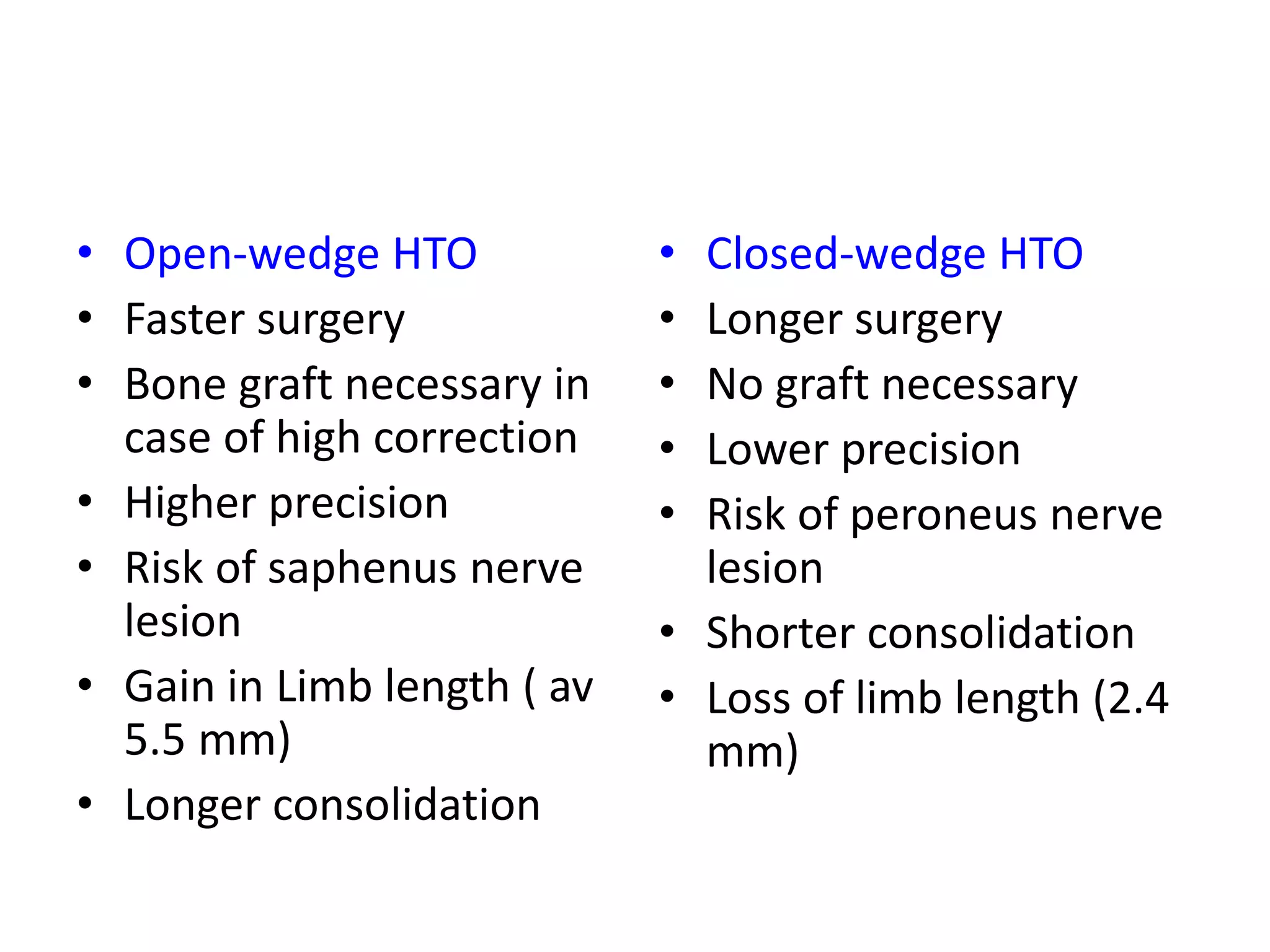
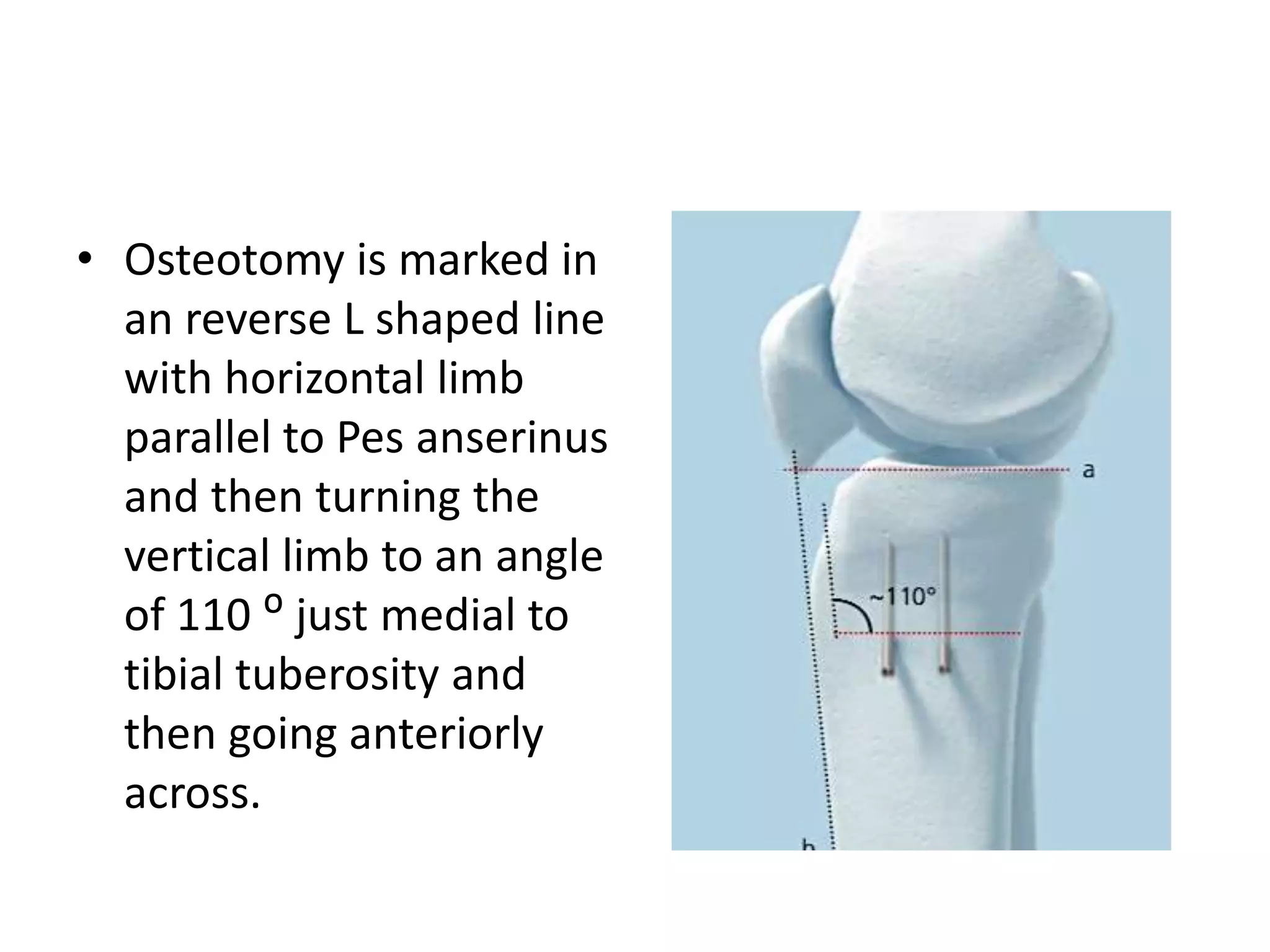
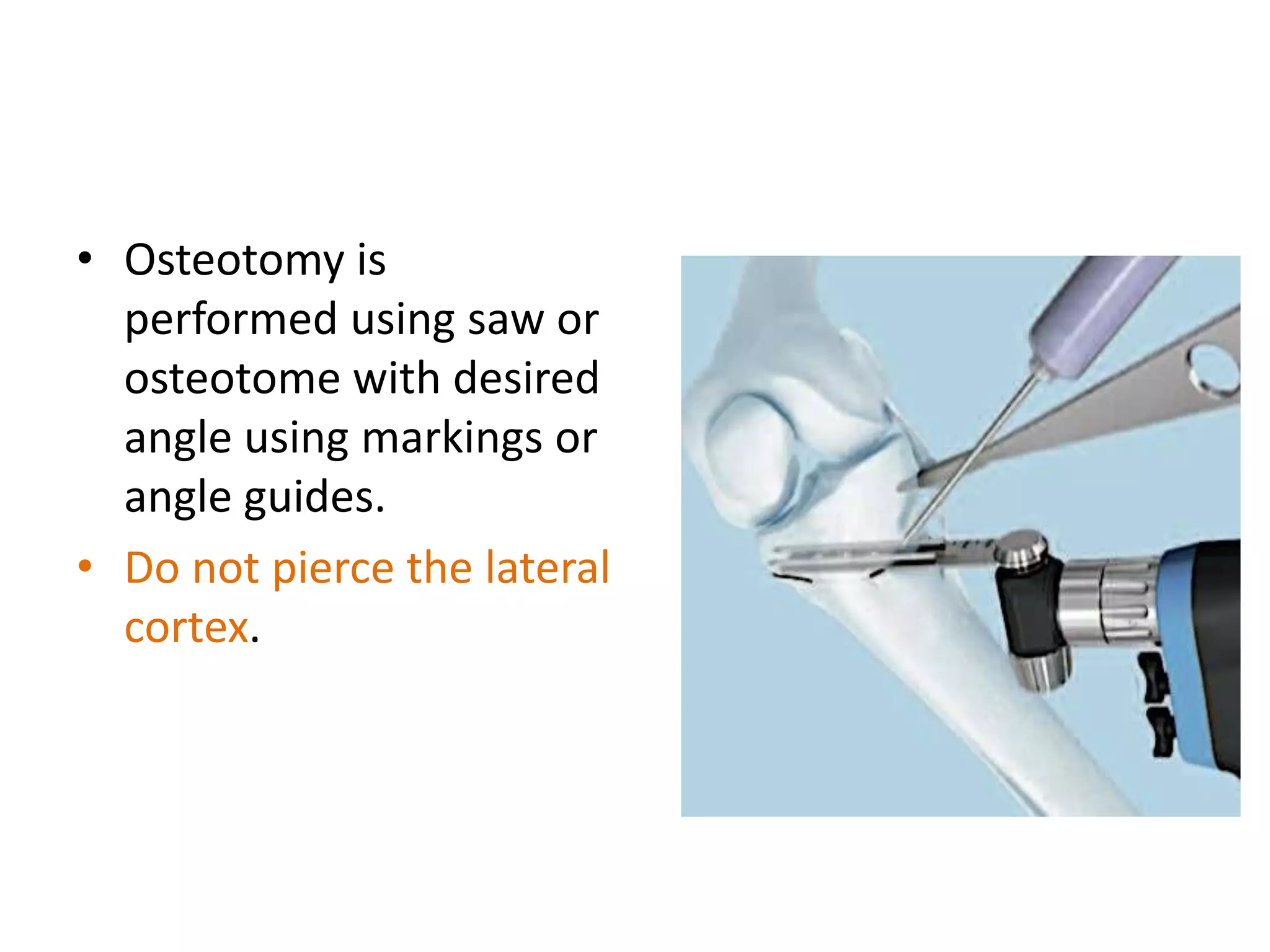
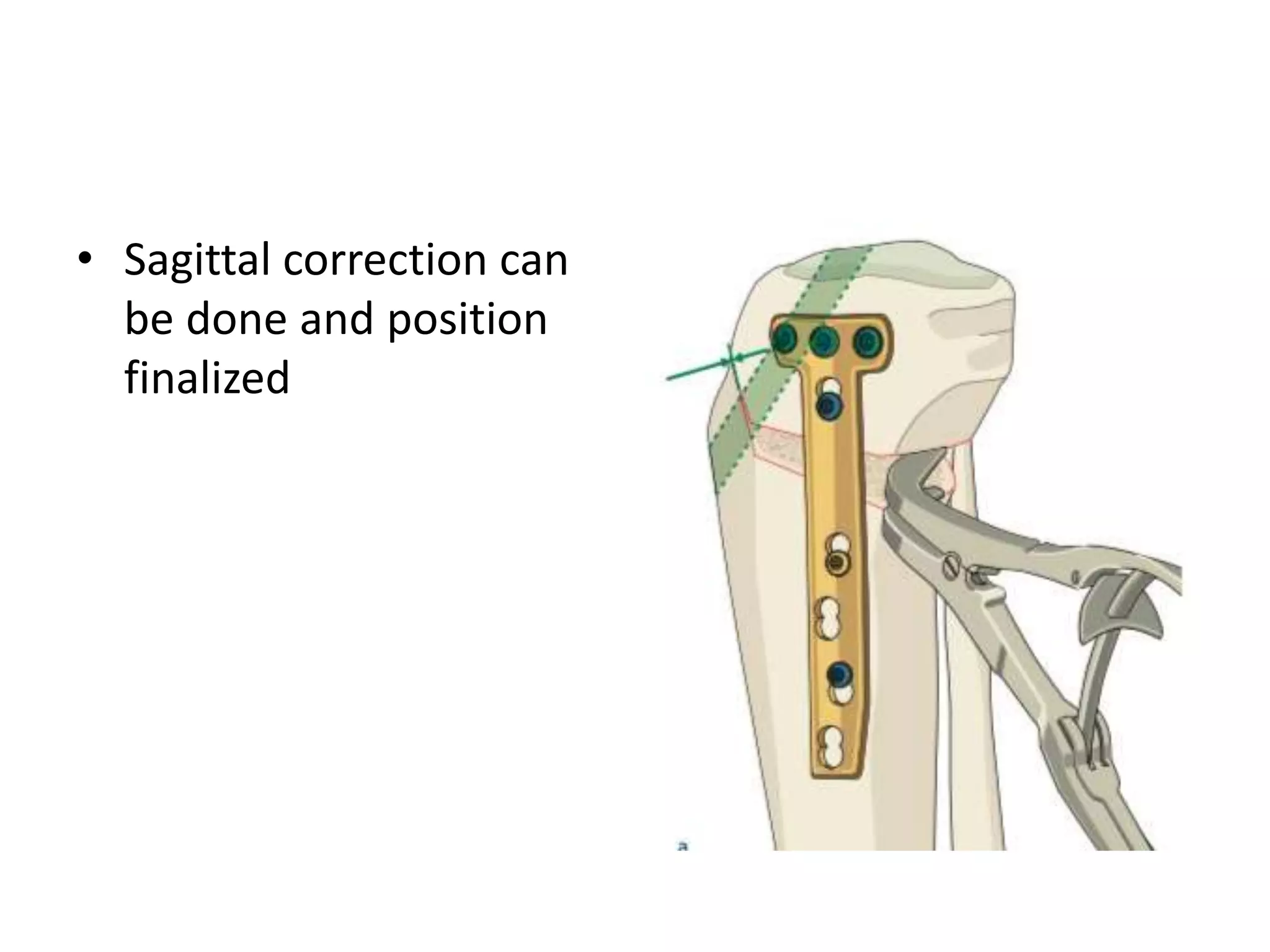
3) Precise planning is important for procedures like open vs closed wedge osteotomy and correcting any concomitant deformities in the sagittal or transverse planes.