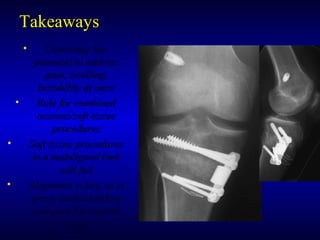
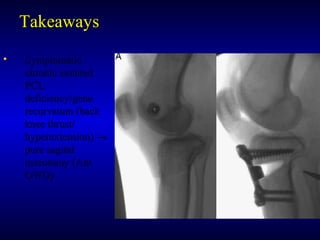
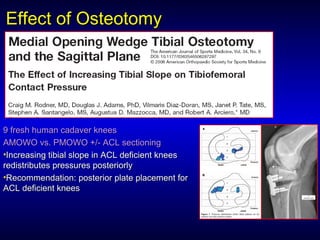
This document summarizes a presentation on medial opening wedge high tibial osteotomy. Key points include:
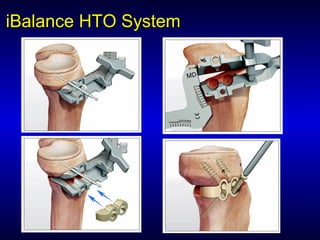
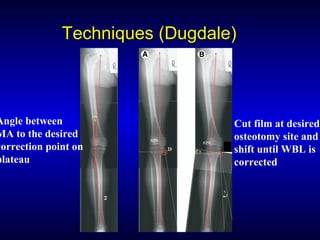
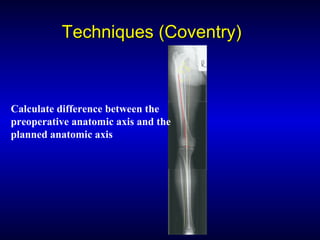
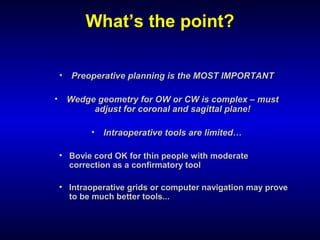
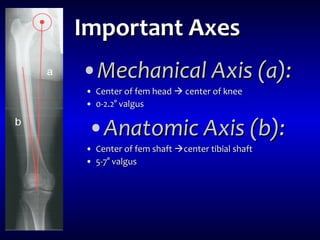
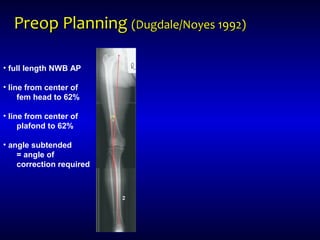
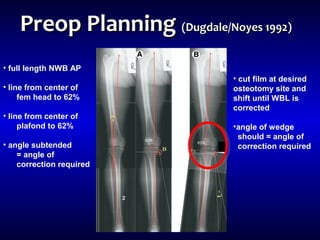
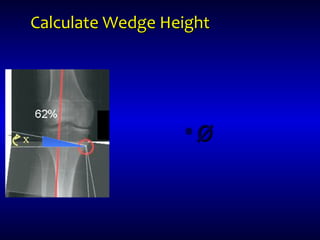
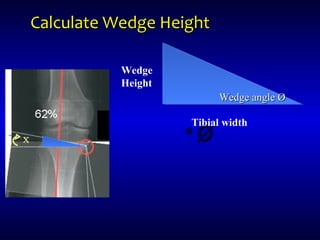
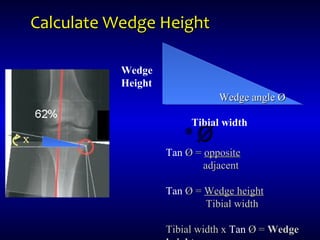
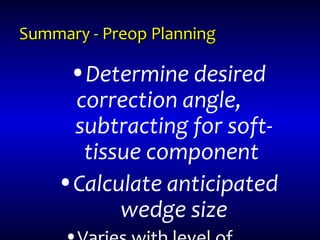
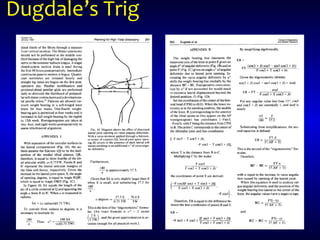
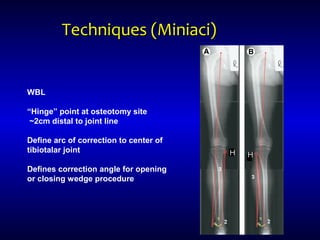
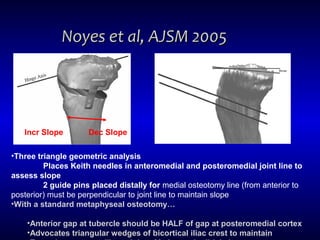
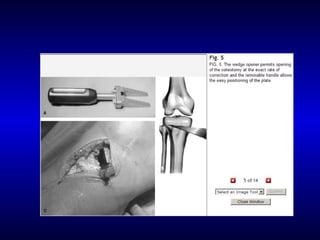
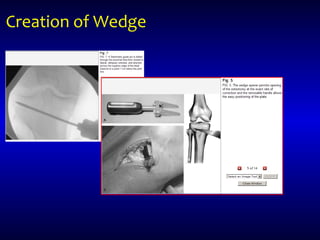
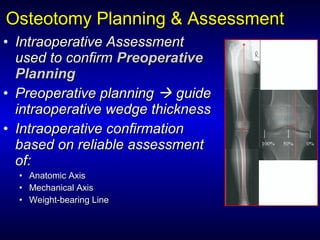
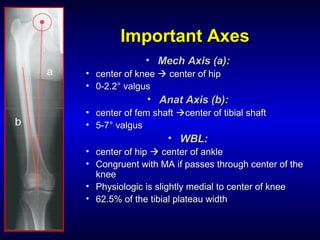
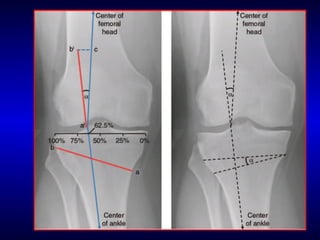
1) Preoperative planning is critical to determine the appropriate correction and wedge size.
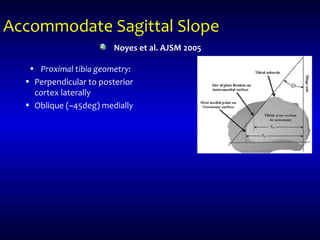
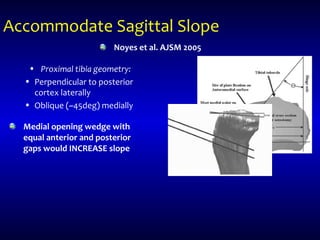
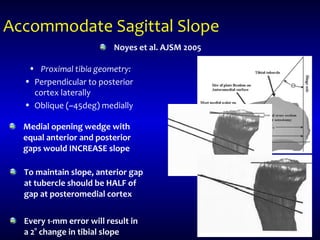
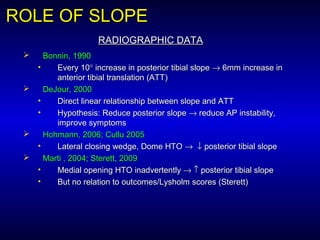
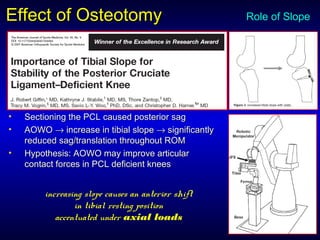
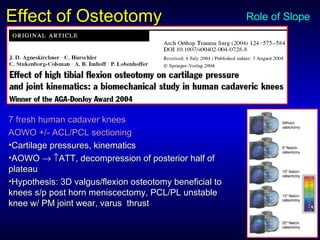
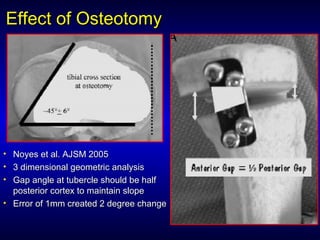
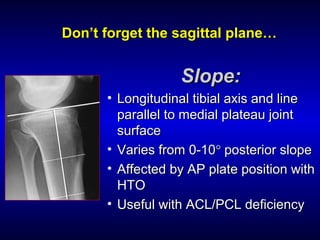
2) Wedge geometry is complex, as the correction depends on both coronal and sagittal plane alignment.
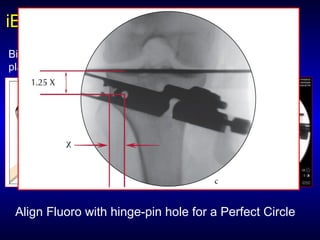
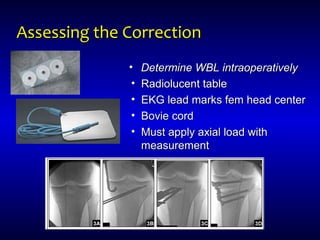
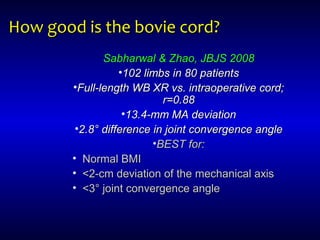
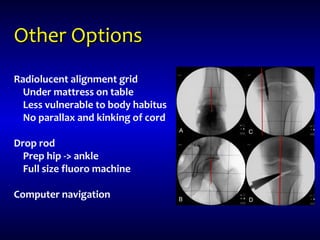
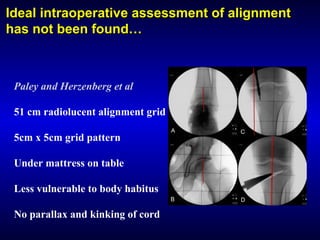
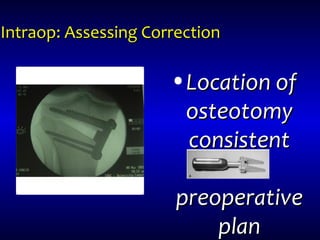
3) Intraoperative assessment of alignment is challenging, and while the bovie cord provides a reasonable estimate, alternatives like radiolucent grids may improve accuracy by reducing parallax error.

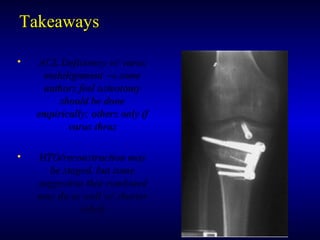
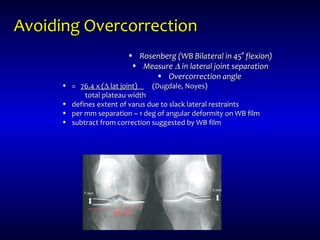
![Avoiding overcorrection…Avoiding overcorrection…
• Rosenberg (WB Bilateral in 45° flexion)Rosenberg (WB Bilateral in 45° flexion)
• MeasureMeasure ΔΔ in lateral joint separationin lateral joint separation
• Overcorrection angleOvercorrection angle
• = 76.4 x [(Δ lat joint)/total plateau width]= 76.4 x [(Δ lat joint)/total plateau width]
• Defines extent of varus due toDefines extent of varus due to
slack lateral restraintsslack lateral restraints
• per mm separation ~ 1 deg ofper mm separation ~ 1 deg of
angular deformity on WB filmangular deformity on WB film
• Subtract from correctionSubtract from correction
suggested by WB filmsuggested by WB film](https://image.slidesharecdn.com/arthrexhtotalk5-150123135044-conversion-gate02/85/Medial-Opening-Wedge-High-Tibial-Osteotomy-15-320.jpg)