The document discusses meniscus transplants, including:
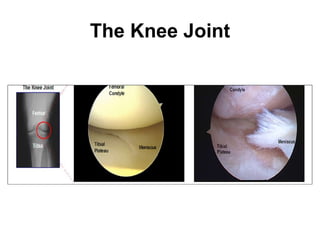
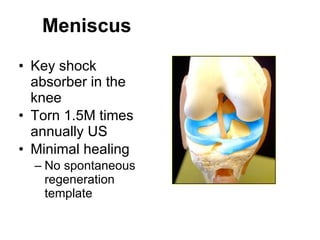
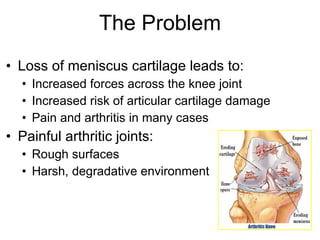
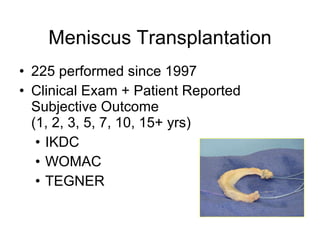
1) Meniscus transplantation can help reduce pain and improve function by restoring a biomechanically favorable environment in the knee.
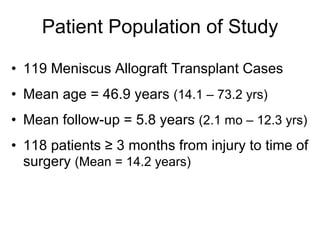
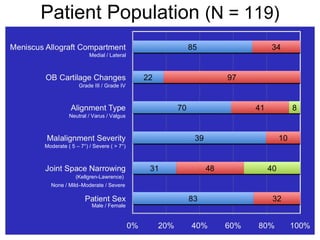
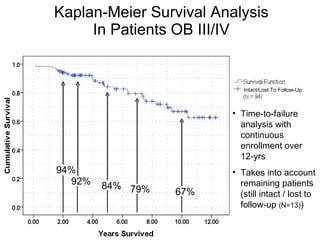
2) A long-term study of 119 meniscus transplant cases found a 79% success rate, with the main factors affecting survival being increased age and number of previous surgeries.
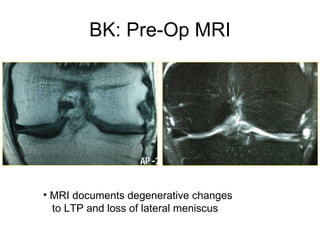
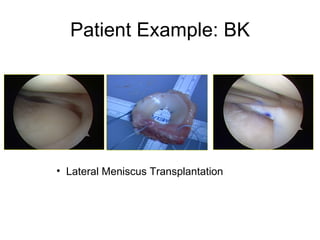
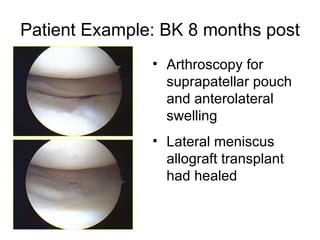
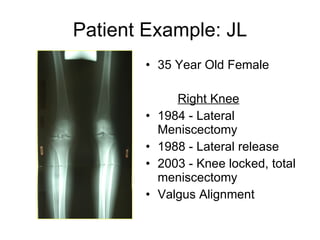
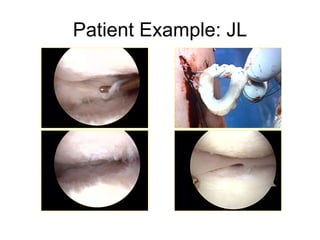
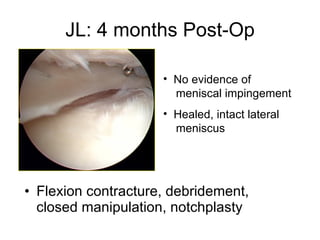
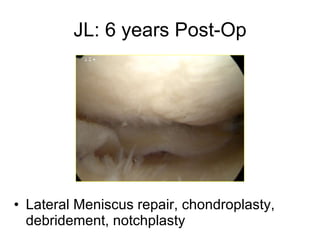
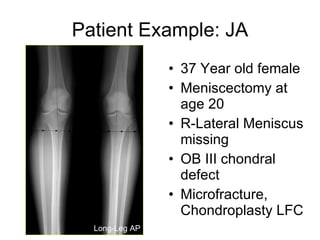
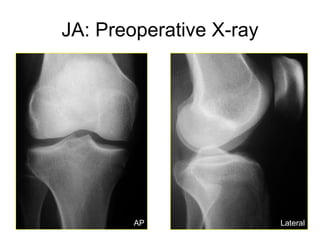
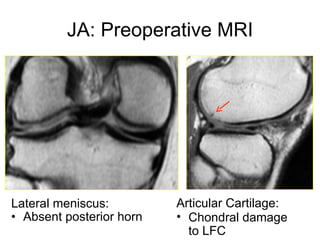
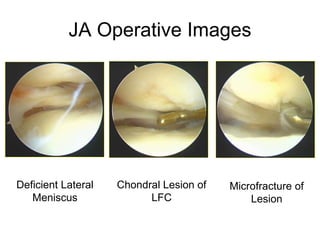
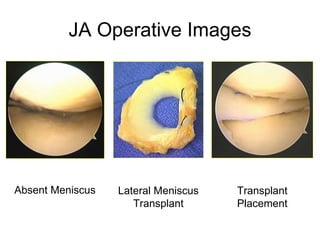
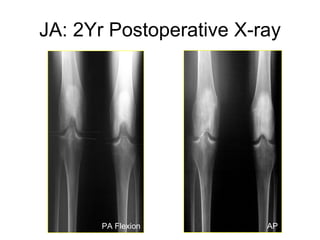
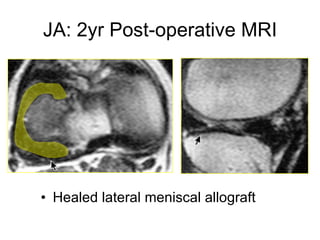
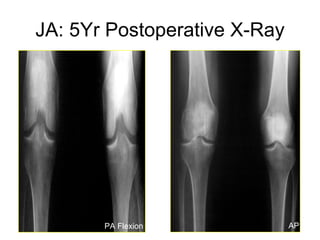
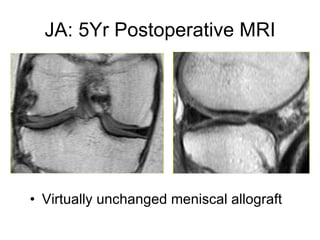
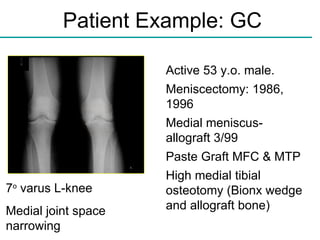
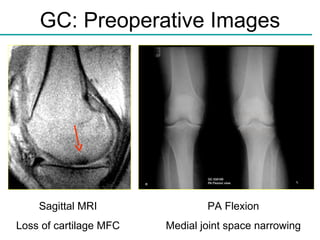
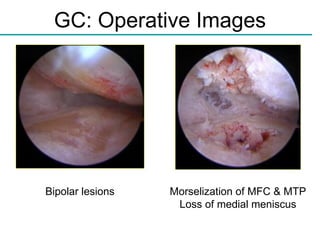
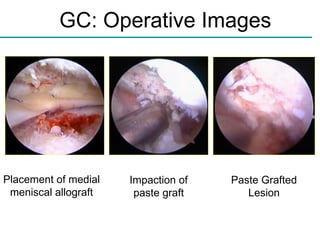
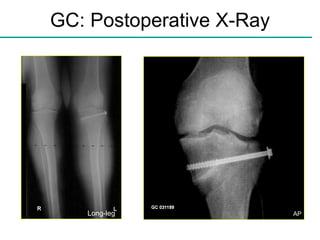
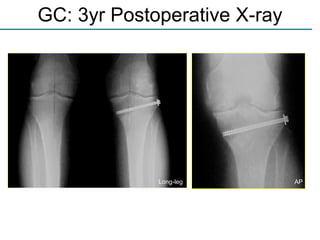
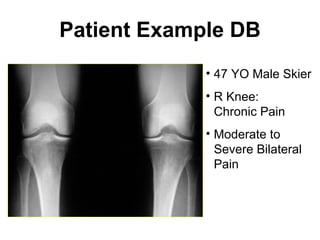
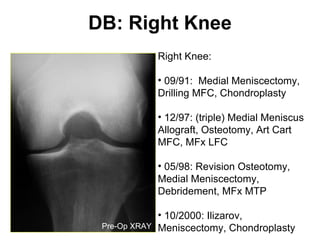
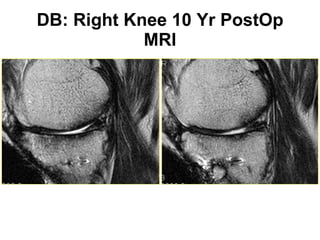
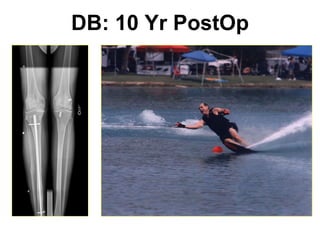
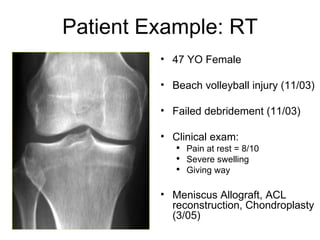
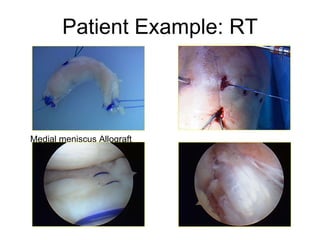
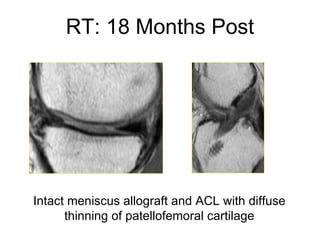
3) Case studies demonstrate that meniscus transplantation, combined with cartilage repair procedures, can provide long-term benefits for patients with meniscus injuries and cartilage damage.


![Results Procedure failure: Removal of allograft without revision (N = 7) , or progression to knee arthroplasty [N = 18 (TKA or UNI)]. 94/119 allograft cases successful (79%) Of 25 failures, Mean time-to-failure: 4.65 ± 2.99 years Range: 2.1 months – 10.37 years Kaplan-Meier estimated mean survival time was 9.93 ± 0.40 years [95%CI: 9.14,10.72] 13 patients were lost to follow-up](https://image.slidesharecdn.com/meniscustransplantslideshow-111111184958-phpapp02/85/Meniscus-Transplant-18-320.jpg)
![Effect of Age 53 patients over 50 (Mean = 56 yrs) KM mean survival = 8.84 years [95% CI: 7.51,10.17] 71.7% (38/53) Success Rate 1 allograft removed 2 mo. post-op 14 progressed to Joint Arthroplasty @ mean 5.1 years 66 patients under 50 (Mean = 39 yrs) KM mean survival = 10.67 years [95% CI: 9.76,11.58] 84.8% (56/66) Success Rate 6 allografts removed @ mean 4.0 years 4 Progressed to Joint Arthroplasty @ mean 5.2 years](https://image.slidesharecdn.com/meniscustransplantslideshow-111111184958-phpapp02/85/Meniscus-Transplant-25-320.jpg)