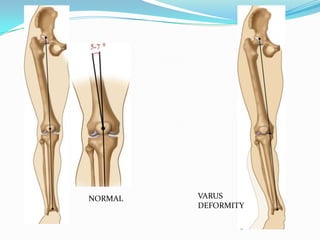
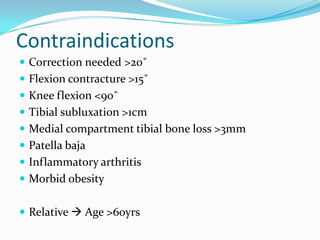
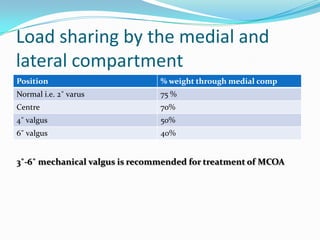
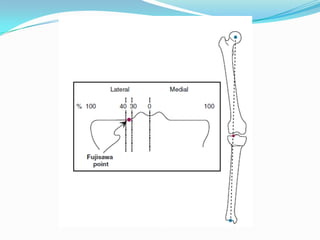
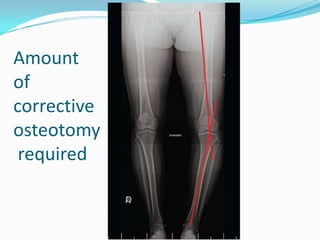
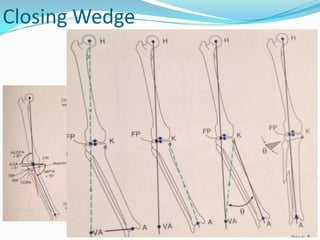
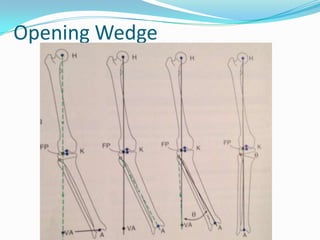
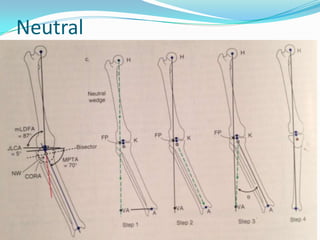
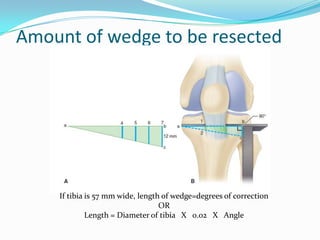
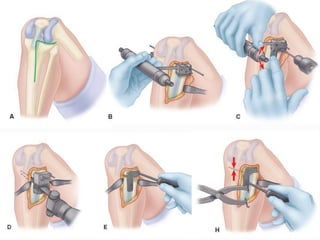
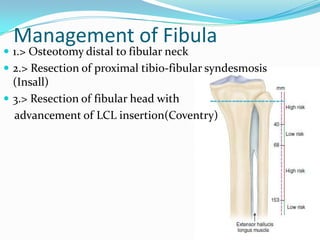
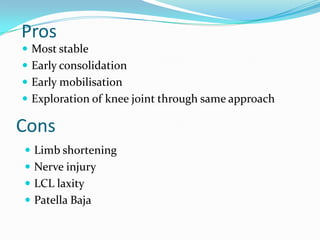
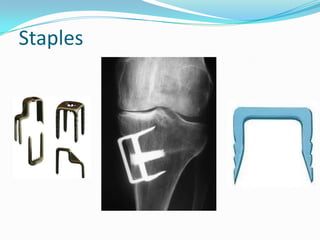
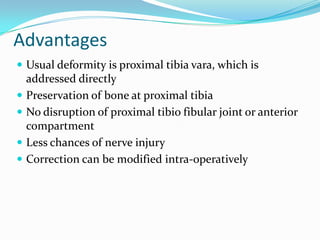
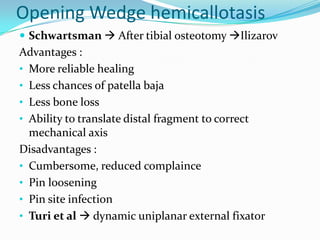
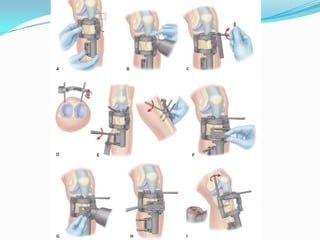
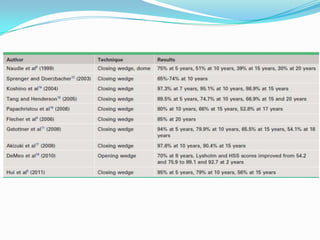
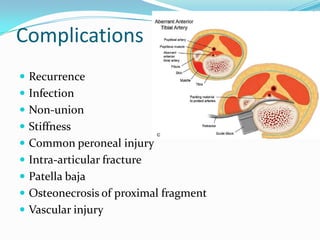
This document discusses high tibial osteotomy (HTO), a procedure that corrects knee alignment to relieve pressure from arthritic areas. It was first described in 1961 and involves cutting and reshaping the tibia to transfer weight from an arthritic to a healthier area of cartilage. The document outlines indications, contraindications, techniques like closing wedge and opening wedge osteotomy, management of the fibula, fixation methods, advantages and disadvantages of different techniques, expected results, and potential complications. HTO is a well-established procedure for unicompartmental knee arthritis with typical satisfactory results in 80% of cases.