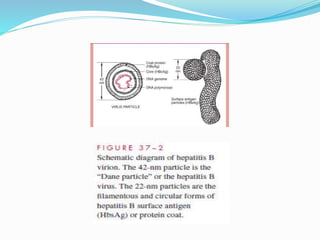
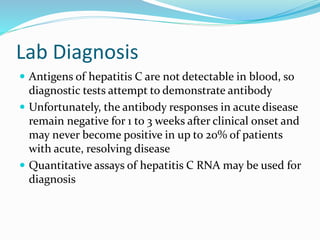
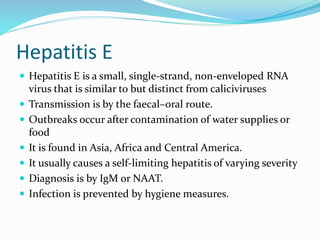
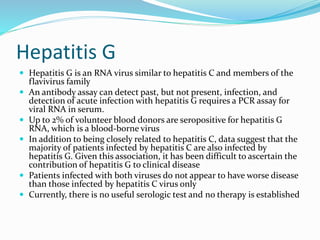
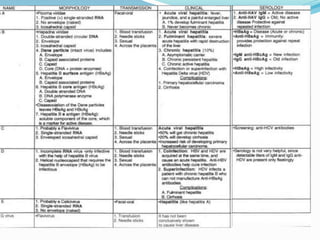
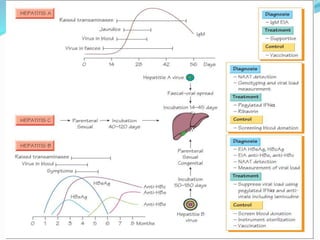
This document discusses several types of hepatitis viruses. It covers hepatitis A virus, hepatitis B virus, hepatitis C virus, hepatitis D virus, and hepatitis E virus. For each virus, it describes key aspects such as transmission, pathogenesis, clinical manifestations, diagnosis, and prevention. Hepatitis viruses can cause liver inflammation and damage, and some may lead to chronic infection or liver cancer if not addressed. Vaccines exist to prevent hepatitis A and B.