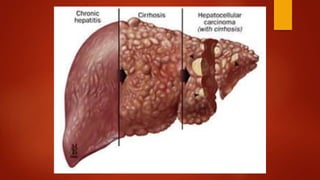
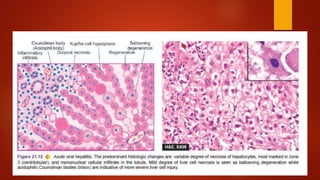
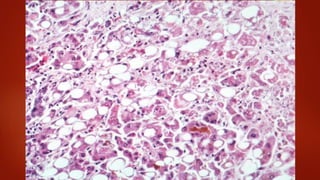
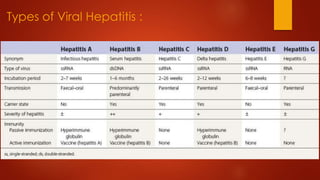
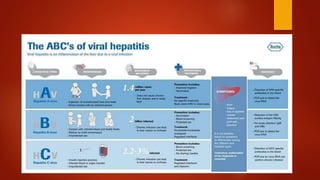
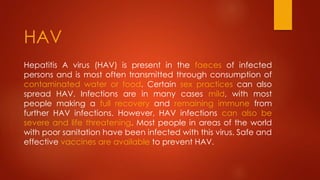
Hepatitis refers to inflammation of the liver, which is commonly caused by viral infections. There are 5 main types of hepatitis viruses - A, B, C, D and E. Hepatitis A and E are typically spread through contaminated food or water, while hepatitis B, C and D usually occur through contact with infected body fluids. Acute hepatitis may present with few or no symptoms, while chronic hepatitis can progress to fibrosis, cirrhosis or liver cancer over many years if left untreated. Diagnosis involves physical exam, imaging, liver function tests and blood tests to detect viral antibodies.