Hepatitis B, C & D Viruses
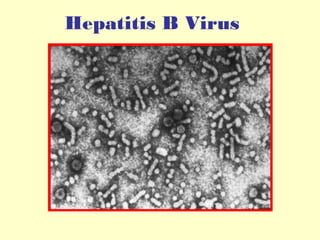
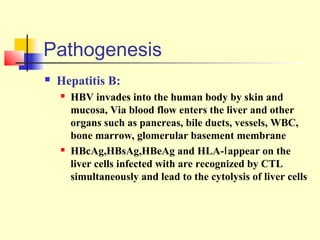
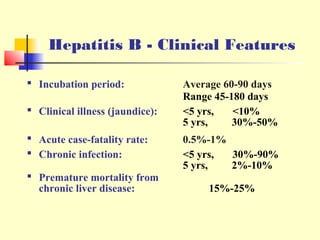
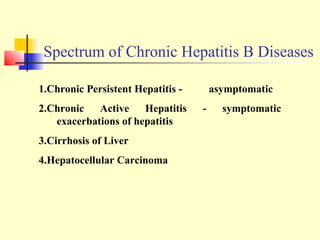
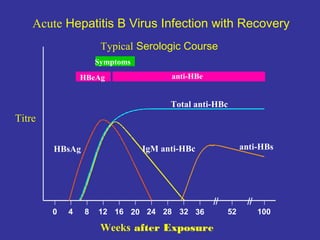
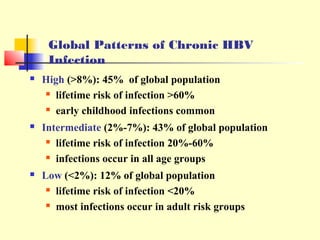
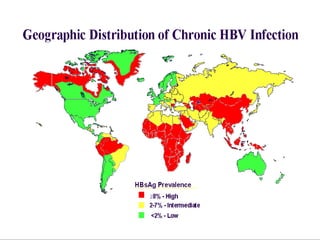
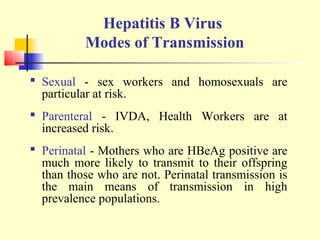
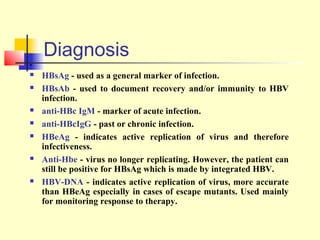
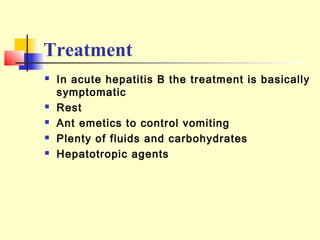
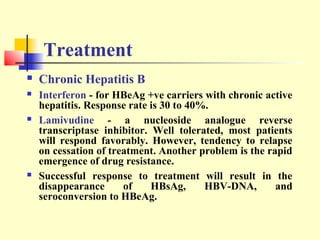
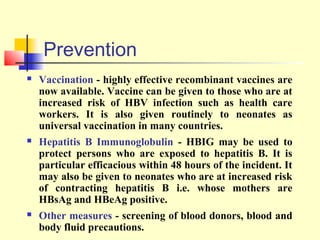
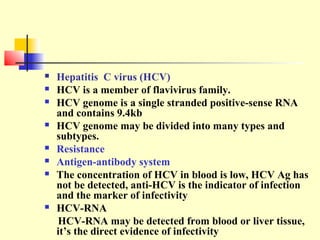
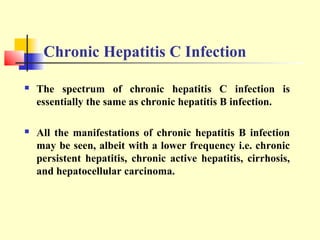
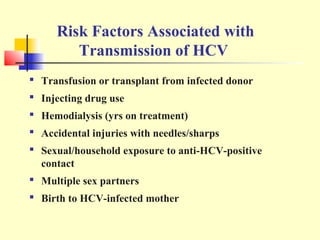
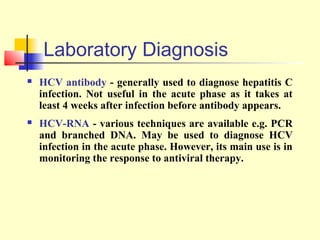
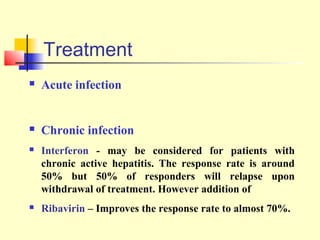
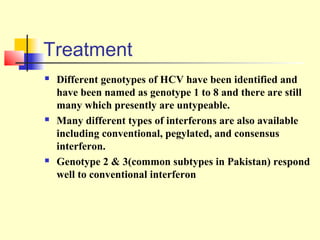
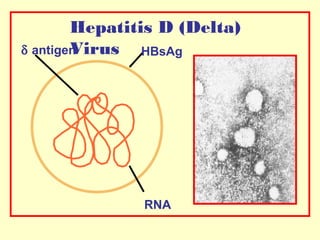
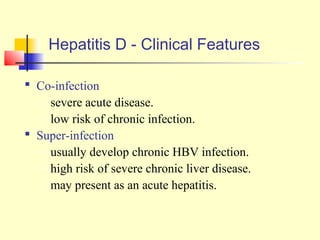
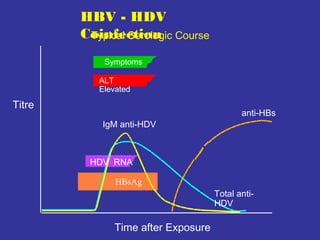
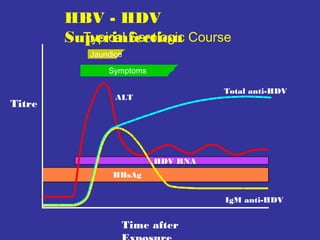
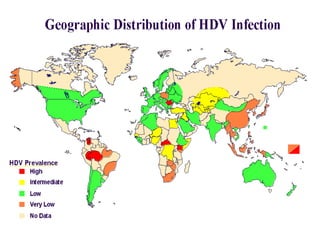
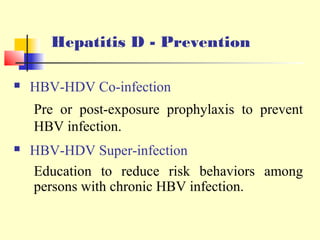
This document summarizes key information about hepatitis B, C, and D viruses. It discusses the etiology, pathology, clinical features, diagnosis, treatment and prevention of each virus. Hepatitis B virus is a hepadnavirus that can cause both acute and chronic infection. Hepatitis C virus is a flavivirus that often leads to chronic infection. Hepatitis D virus can only infect those also infected with hepatitis B and increases the severity of liver disease. Vaccination and blood screening are important prevention strategies for these viral hepatitises.