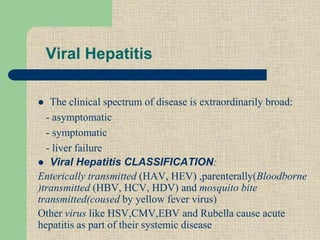
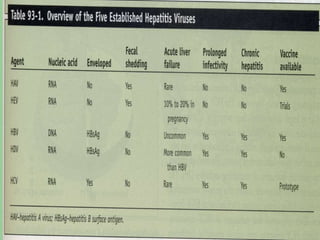
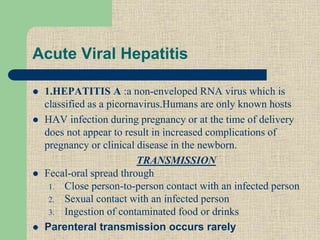
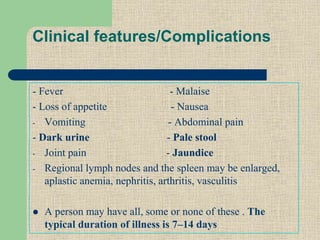
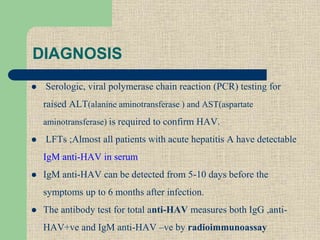
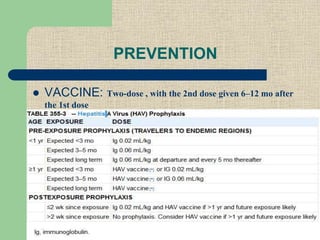
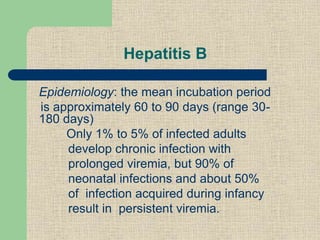
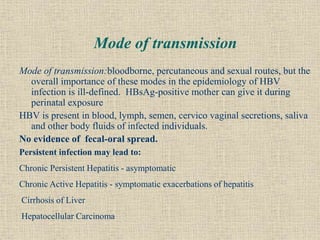
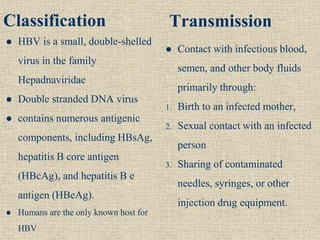
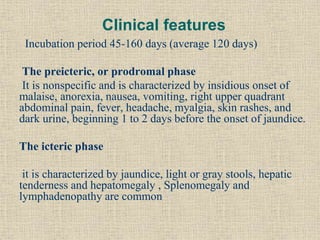
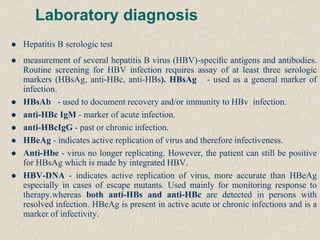
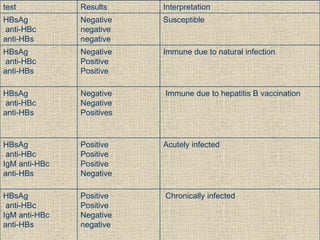
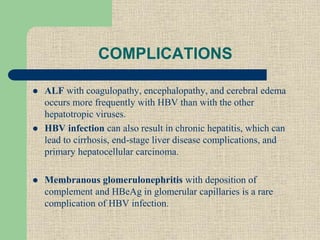
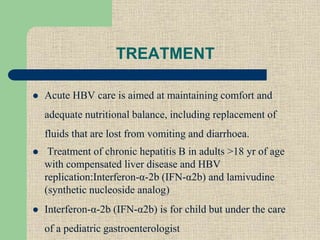
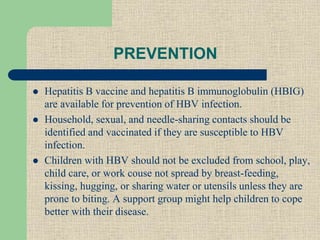
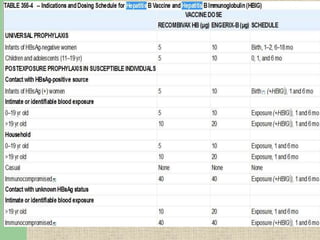
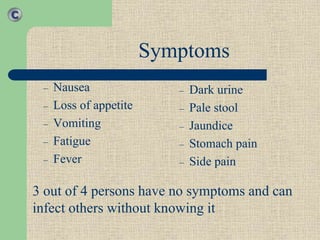
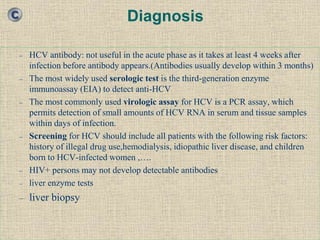
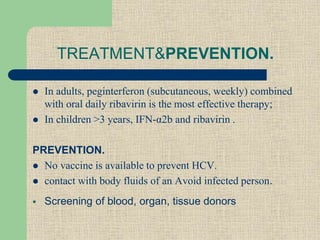
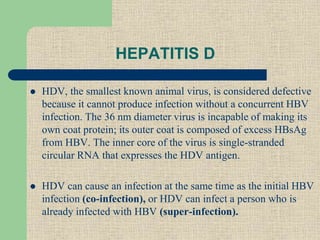
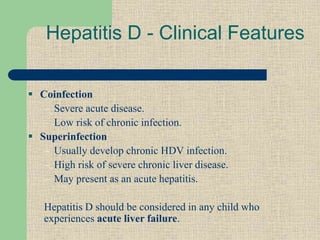
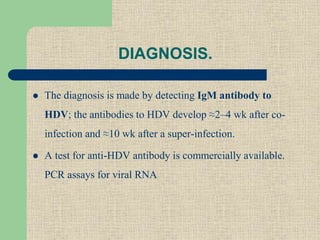
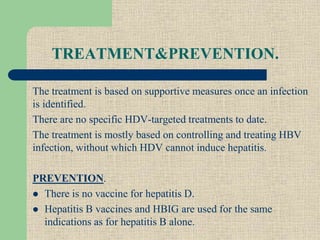
Hepatitis is an inflammatory process affecting the liver, commonly caused by various viruses, including Hepatitis A, B, and C. The clinical manifestations can range from asymptomatic to severe liver failure, and treatment is largely supportive, particularly in acute cases, while vaccination is key for prevention of Hepatitis A and B. Hepatitis D requires concurrent HBV infection to induce disease and lacks specific treatments, underscoring the importance of managing HBV infections.