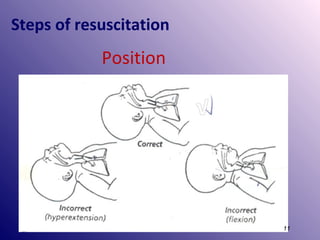
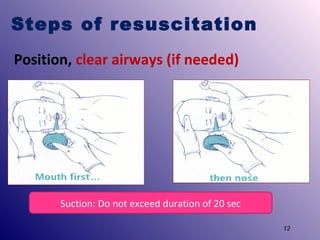
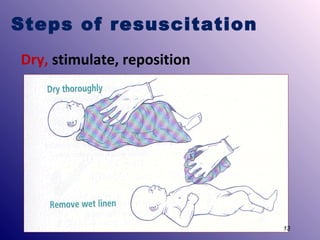
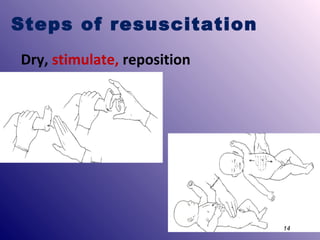
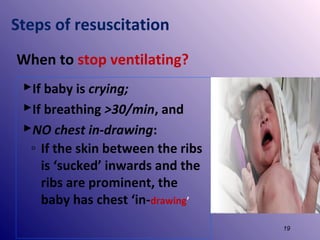
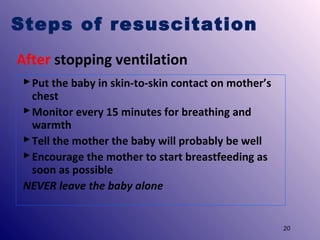
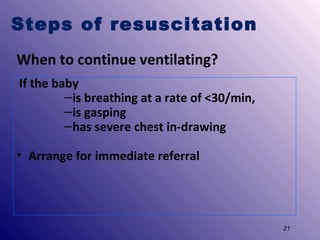
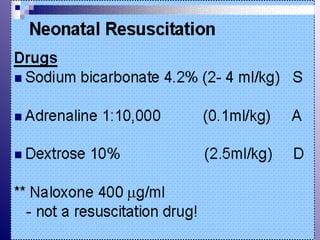
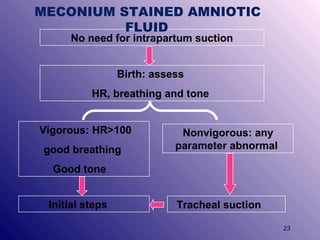
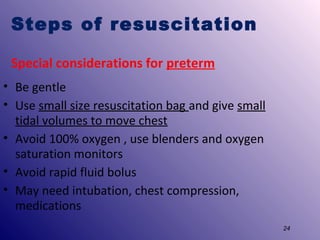
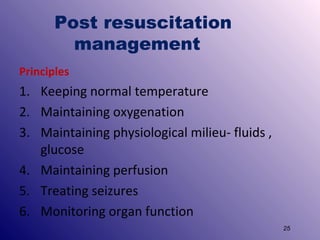
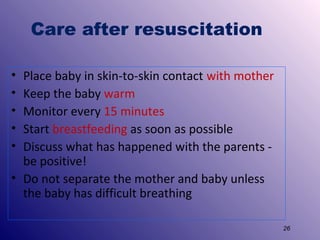
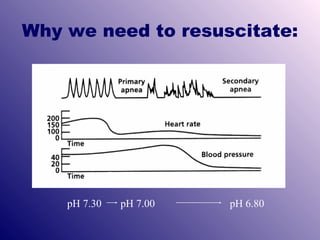
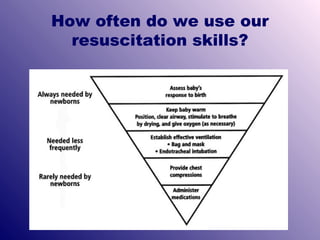
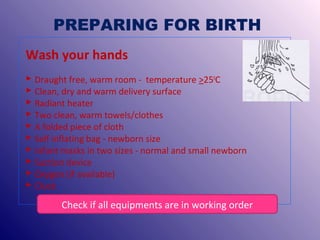
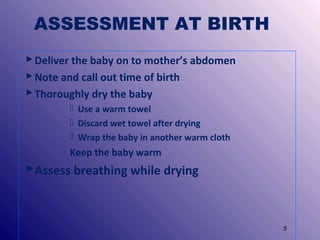
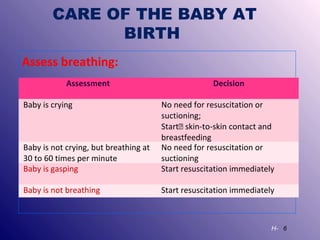
This document provides guidance on resuscitating newborn babies. It outlines the steps needed to prepare for birth, including ensuring necessary equipment is available and in working order. It describes how to assess the baby at birth and determine if resuscitation is required based on breathing, heart rate, and muscle tone. The key steps of newborn resuscitation are also summarized, including positioning, clearing airways, drying, stimulating, and ventilating the baby if needed. Special considerations for preterm babies and post-resuscitation care of keeping the baby warm and with the mother are also highlighted.
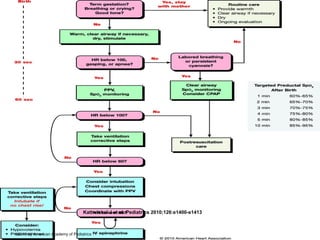

![Steps of resuscitation
If the baby is not breathing or gasping
◦ Call for help!
◦ Cut cord quickly, transfer to a firm, warm surface
[under a radiant heater]
◦ Inform the mother that baby has difficulty breathing
and you will help the baby to breathe
◦ Start newborn resuscitation
9](https://image.slidesharecdn.com/resuscitation-enc-3-140115121452-phpapp02/85/Resuscitation-enc-3-9-320.jpg)