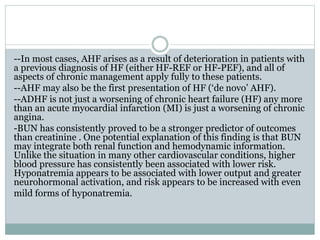
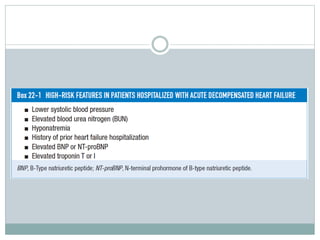
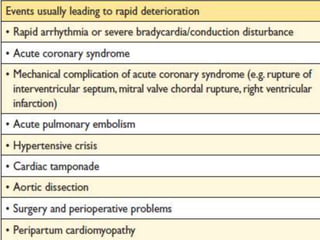
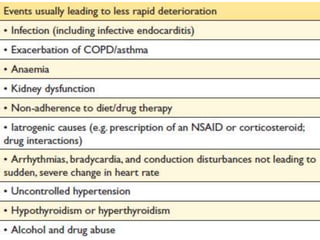
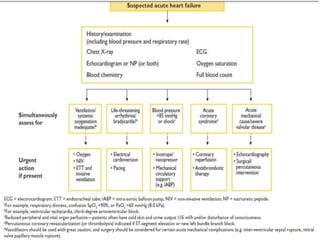
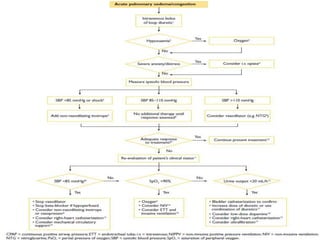
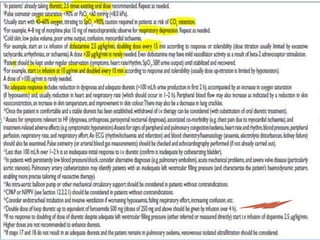
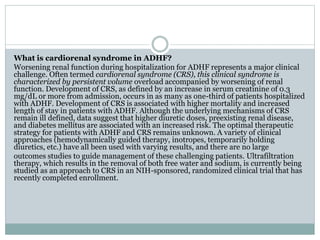
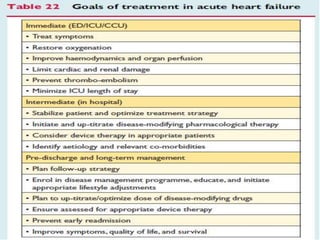
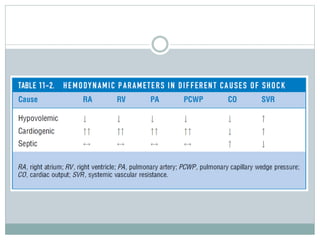
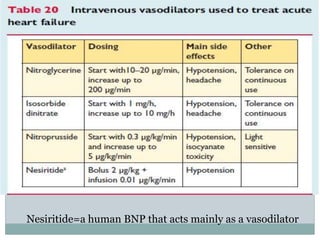
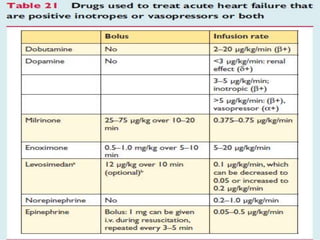
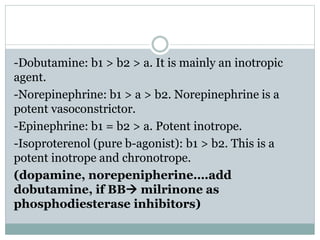
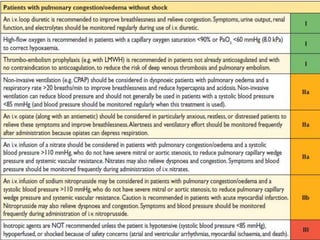
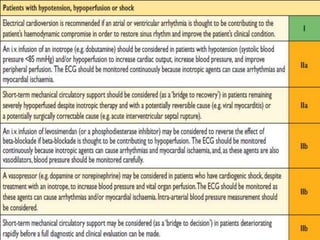
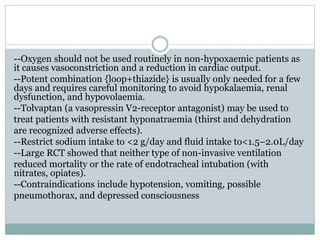
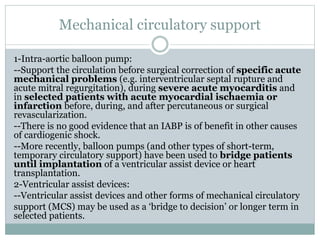
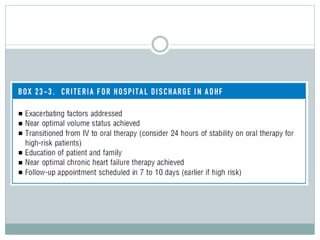
This document discusses acute heart failure (AHF), including its definition, initial signs of end organ dysfunction, potential end organ dysfunction, and causes. It notes that AHF often arises from a deterioration of chronic heart failure and may be a first presentation. It also discusses biomarkers like BUN and hyponatremia as predictors of outcomes. The document covers diuretic use and its association with adverse events, as well as approaches to decongestion. It defines cardiorenal syndrome in AHF and notes its association with worse outcomes. Various inotropic agents are also discussed.