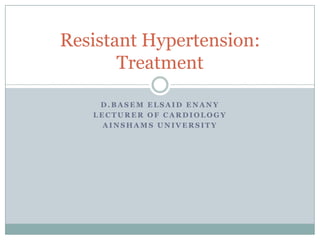
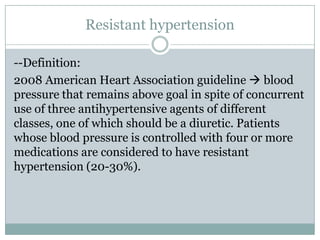
This document discusses resistant hypertension and its treatment. It defines resistant hypertension as blood pressure that remains above goal despite use of three antihypertensive agents from different classes including a diuretic. Treatment involves identifying and treating secondary causes, adjusting medications that raise blood pressure, monitoring blood pressure outside the office, making lifestyle changes, and using pharmacologic therapies like diuretics, aldosterone antagonists, and catheter-based renal denervation. While renal denervation showed promise in early trials, the SYMPLICITY HTN-3 trial found it did not significantly reduce blood pressure compared to a sham procedure.





![CHOICE OF REGIMEN
--The triple combination of an ACE inhibitor or ARB, a long-
acting dihydropyridine calcium channel blocker (usually
amlodipine), and a long-acting thiazide diuretic (preferably
chlorthalidone) is often effective and generally well tolerated.
--Uncontrolled with such a three drug regimen at maximum
recommended and tolerated doses spironolactone: 12.5
mg/day (which requires splitting of a 25 mg tablet) before
titrating to 25 and, if necessary, 50 mg/day.
The risk of adverse effects such as gynecomastia, breast
tenderness, and erectile dysfunction increases with higher
doses.
[eplerenone, is now generic and does not induce the side effects
seen with spironolactone]](https://image.slidesharecdn.com/htnresistant-140403095039-phpapp01/85/Resistant-hypertension-8-320.jpg)
![--Some patients with resistant hypertension are being treated with a three
drug regimen different:
If the patient is on hydrochlorothiazide, switch to chlorthalidone.
If the current regimen includes a drug not from the three recommended drug
classes, add the missing preferred drug and assess the response. Do not
discontinue any drugs, as long as they are well tolerated, before achieving
blood pressure control.
--If the patient is still hypertensive, additional medications are added
sequentially. Possible agents that may be used include vasodilating beta
blockers (labetalol, carvedilol, or nebivolol), centrally acting agents (clonidine
or guanfacine)[may be effective, but adverse effects are common], and direct
vasodilators (hydralazine or minoxidil) [Fluid retention and tachycardia are
common side effects. Minoxidil also causes hirsutism, which may be a
particular problem in women that may require switching to
hydralazine(lupus
like=withdrawal, nausea, vomiting, flushing,tachycardia), and pericarditis].](https://image.slidesharecdn.com/htnresistant-140403095039-phpapp01/85/Resistant-hypertension-9-320.jpg)