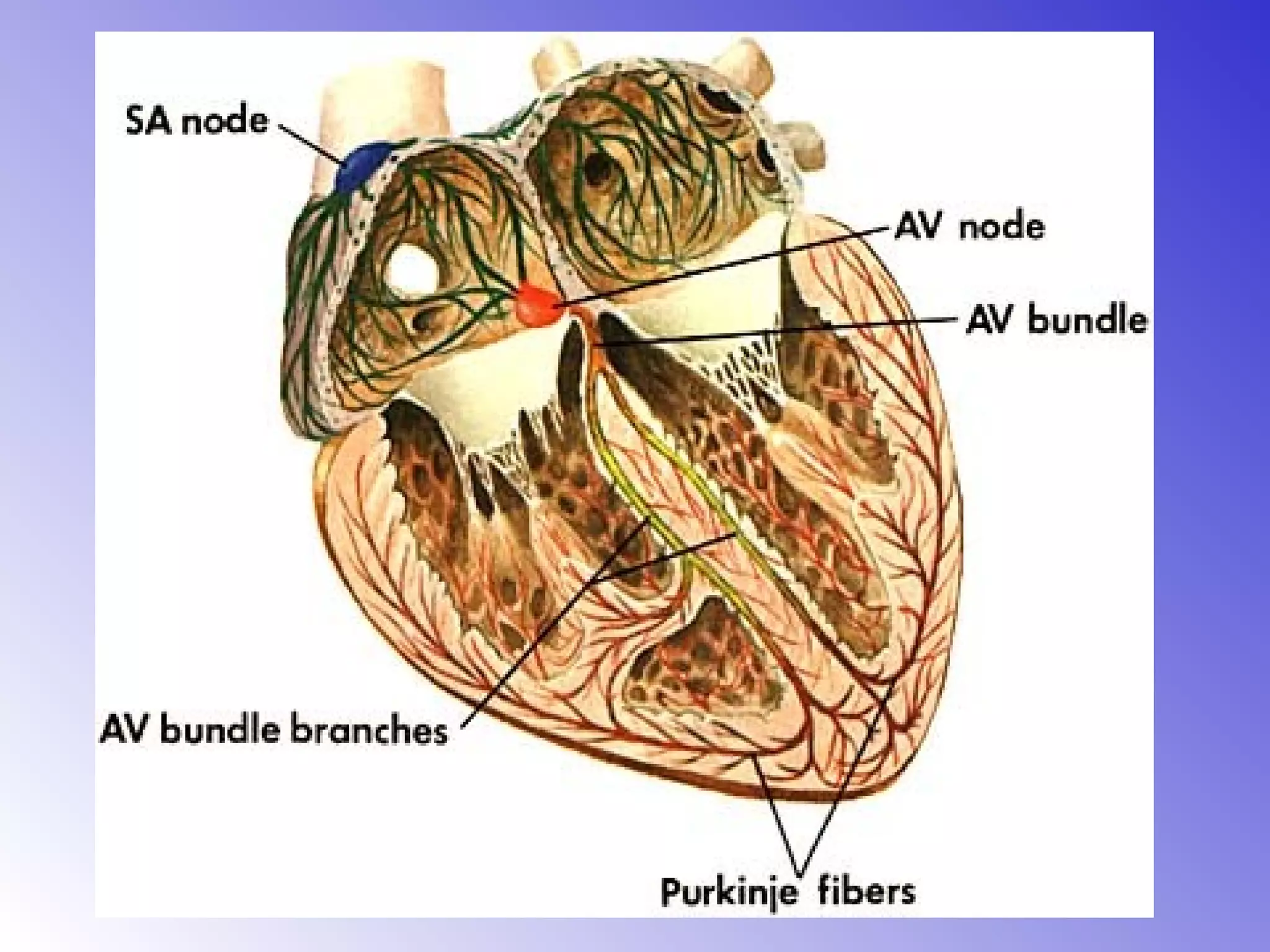
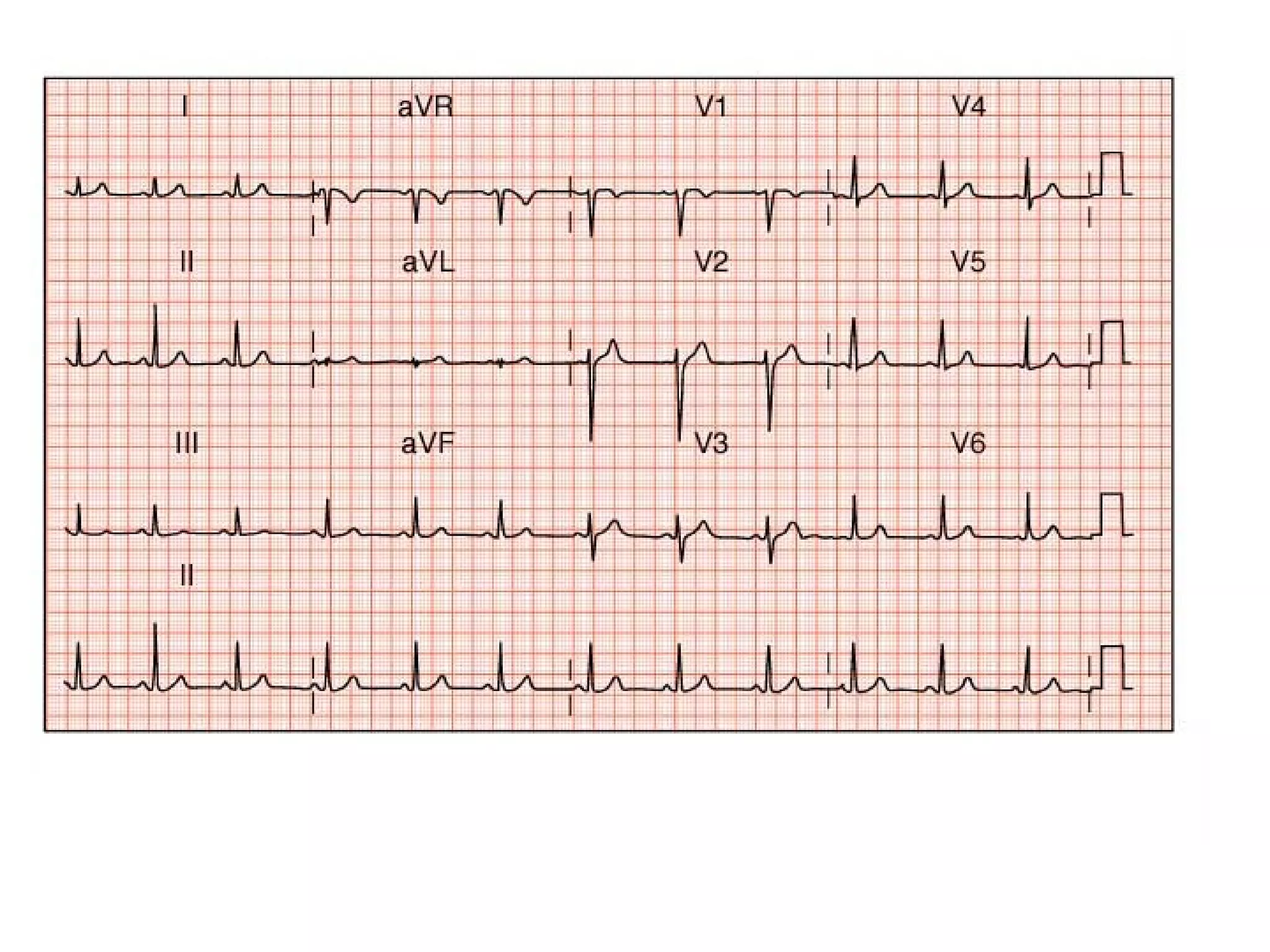
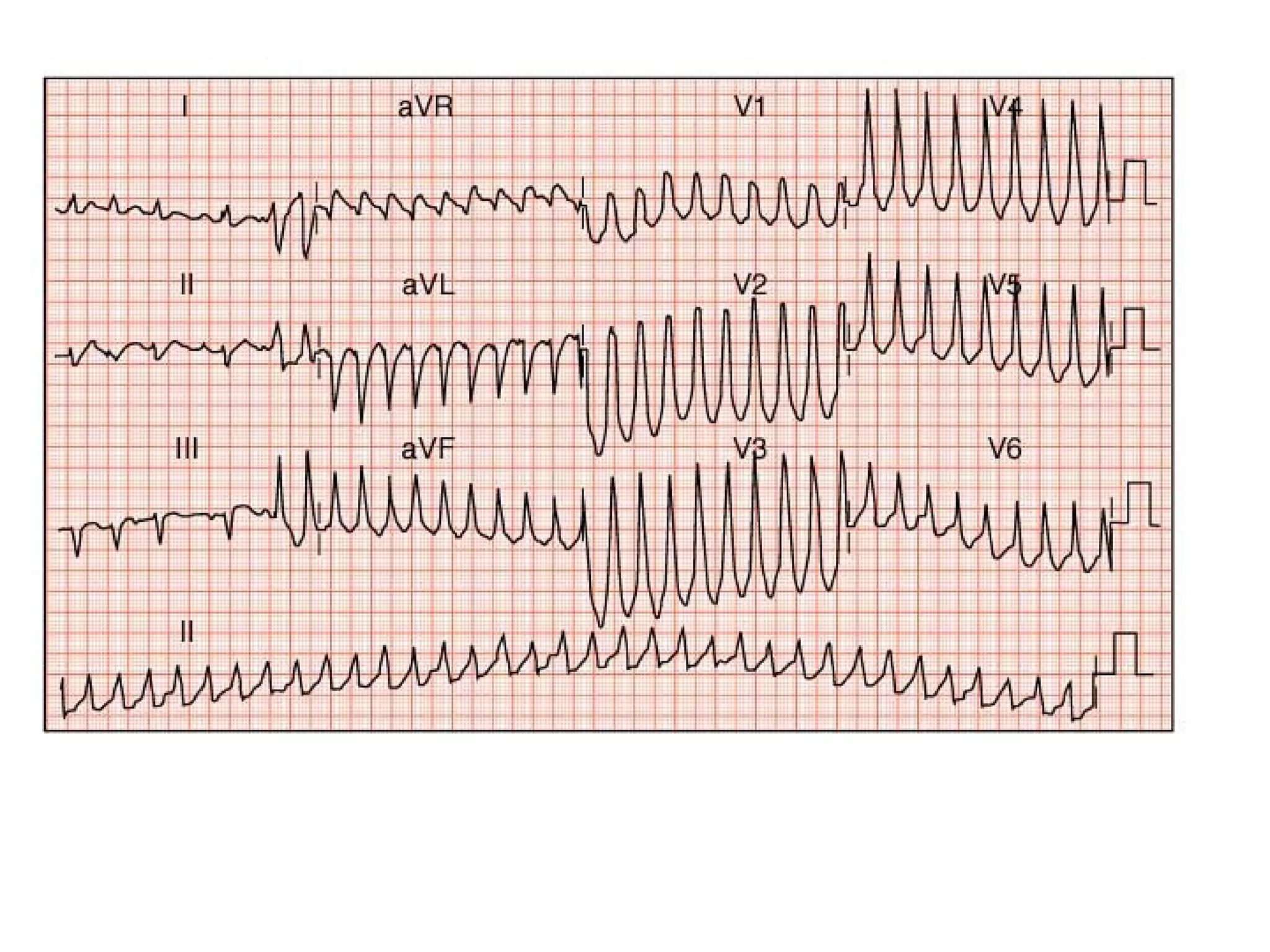
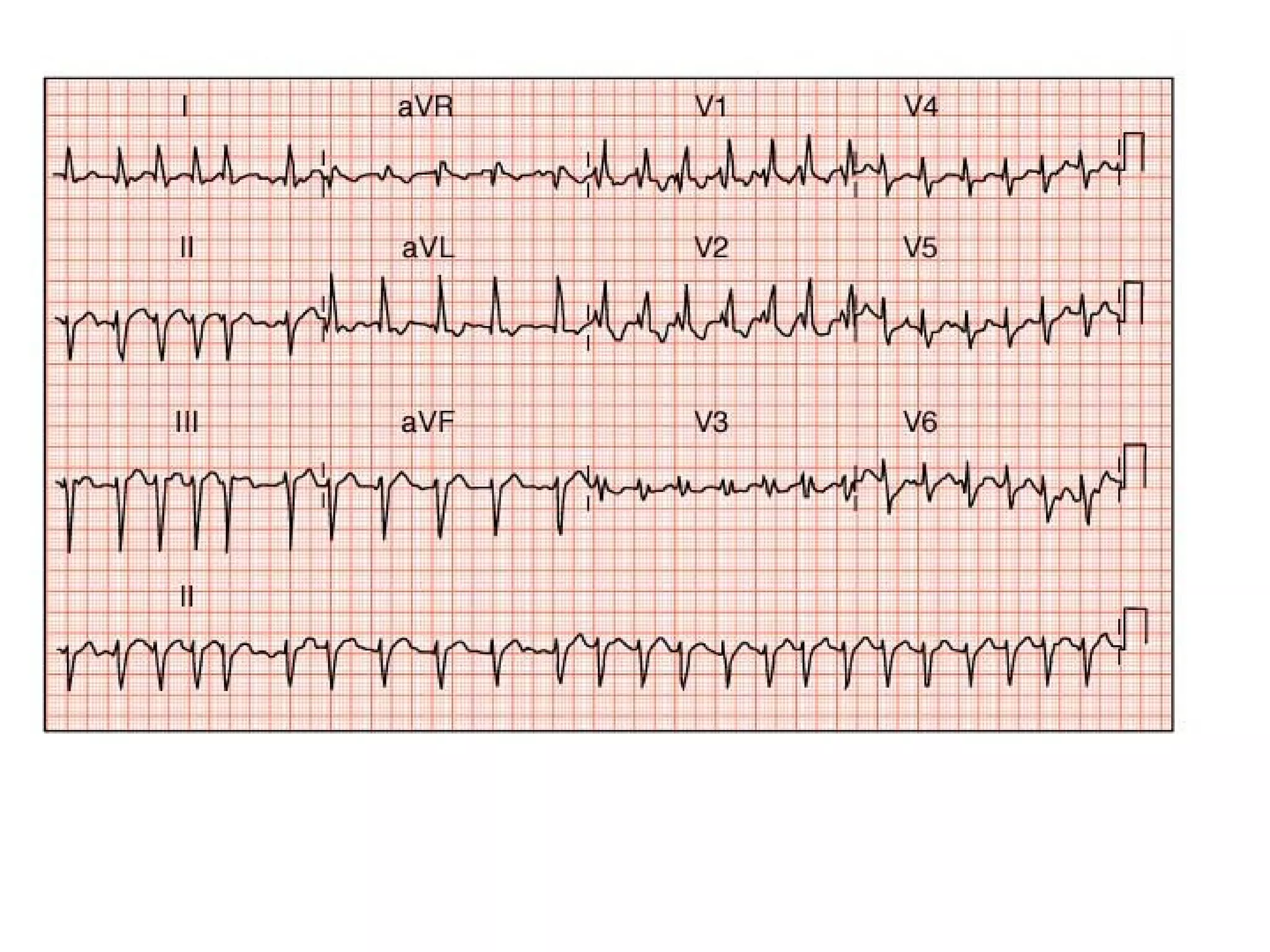
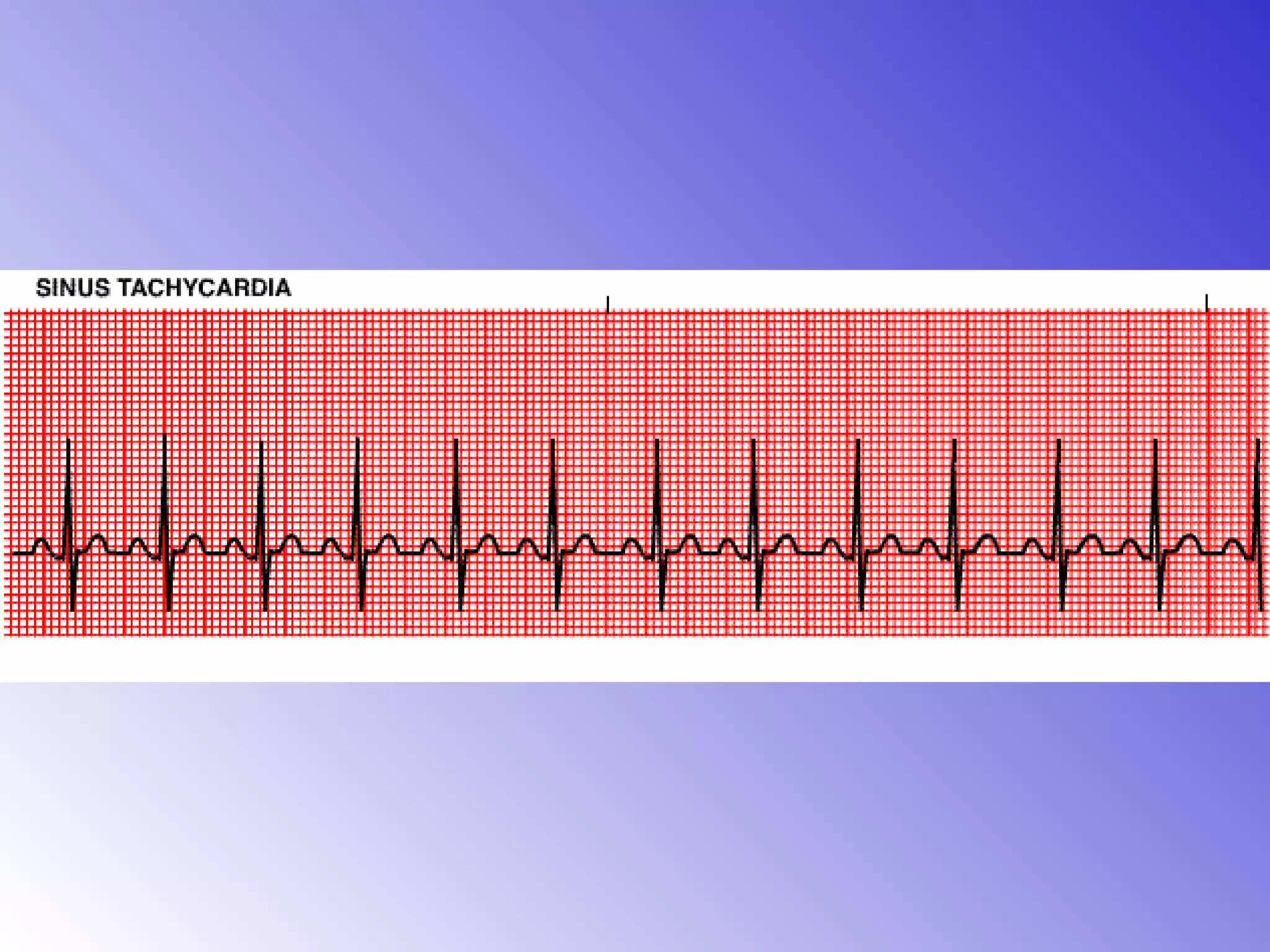
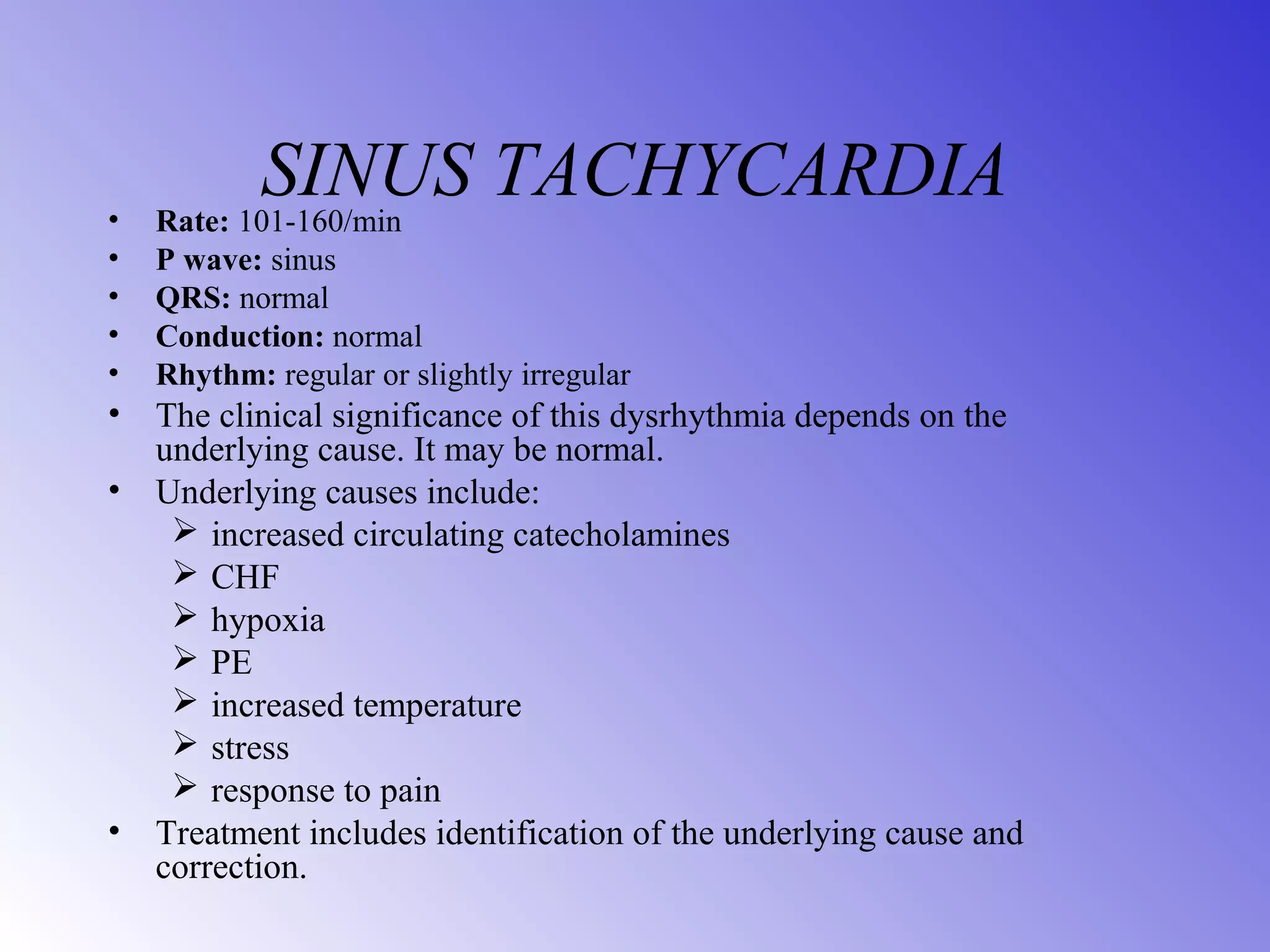
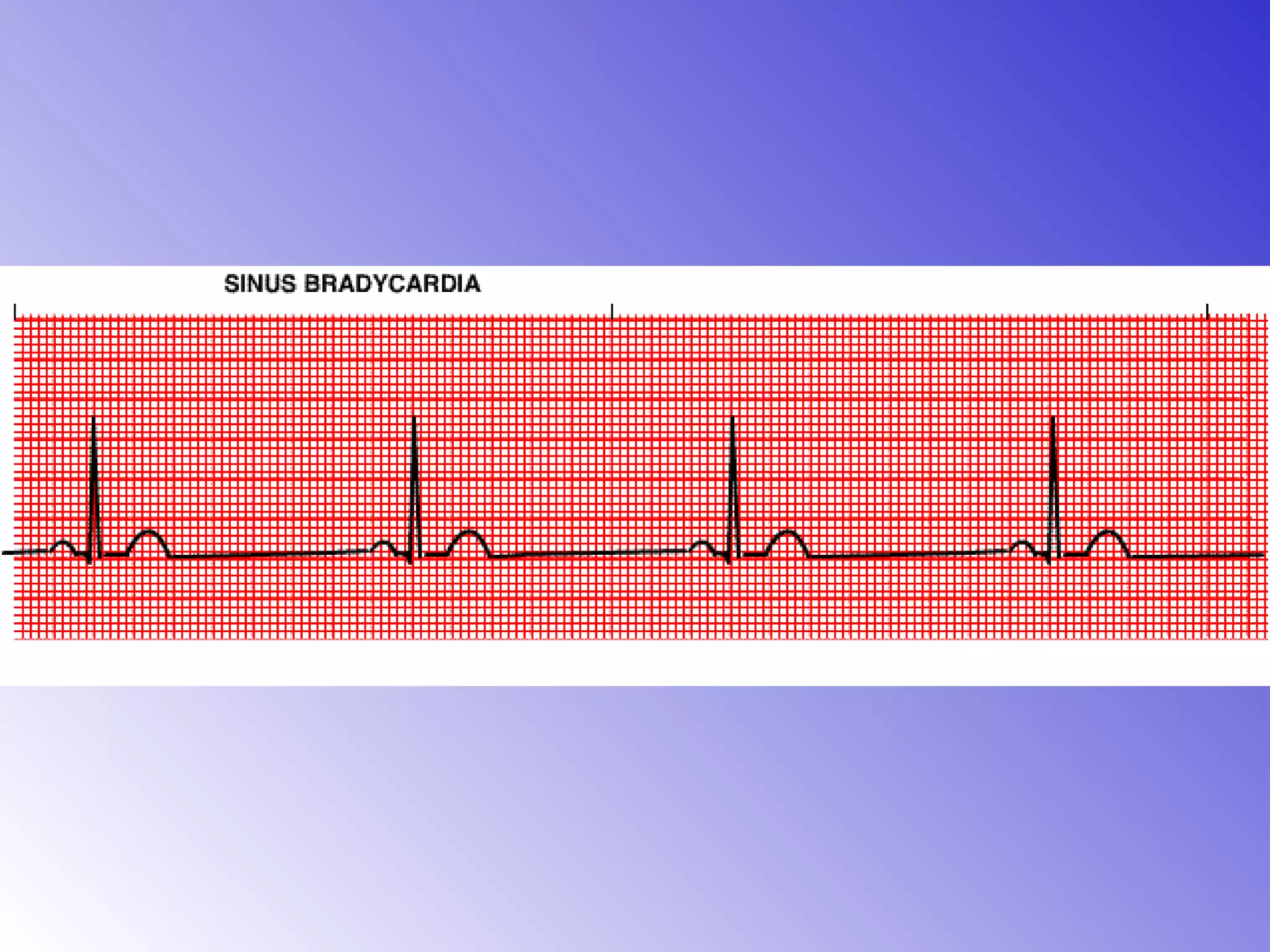
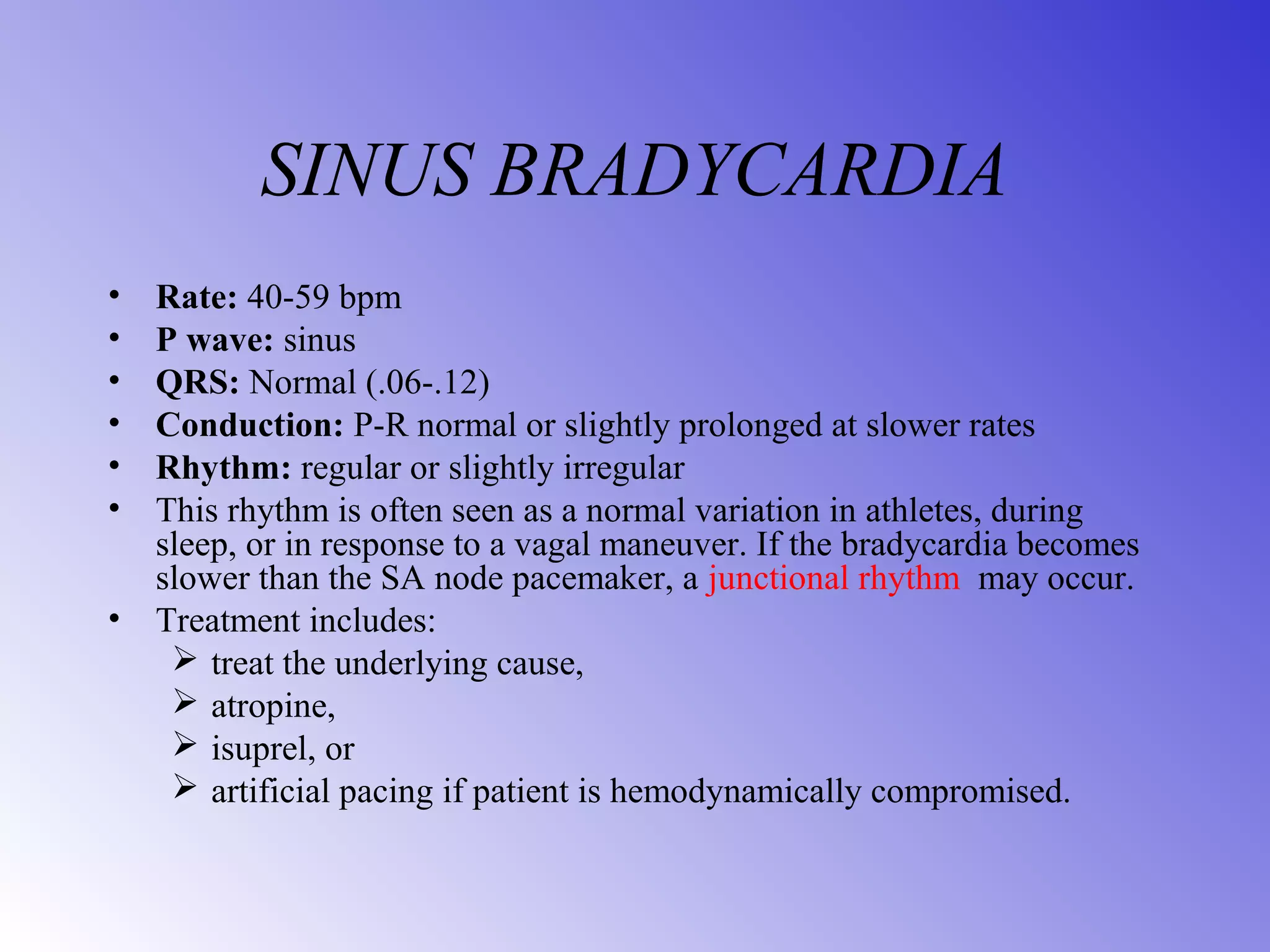
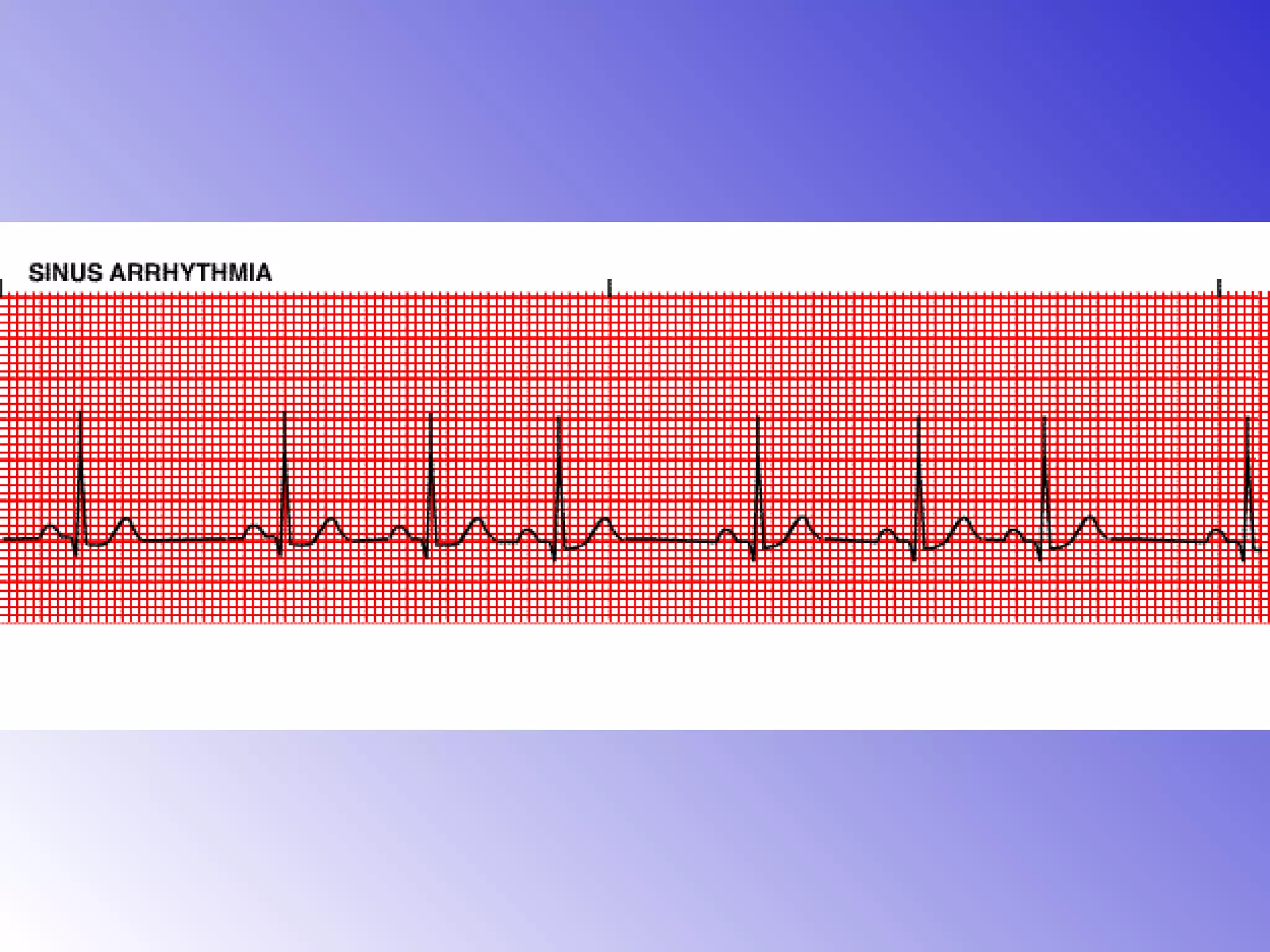
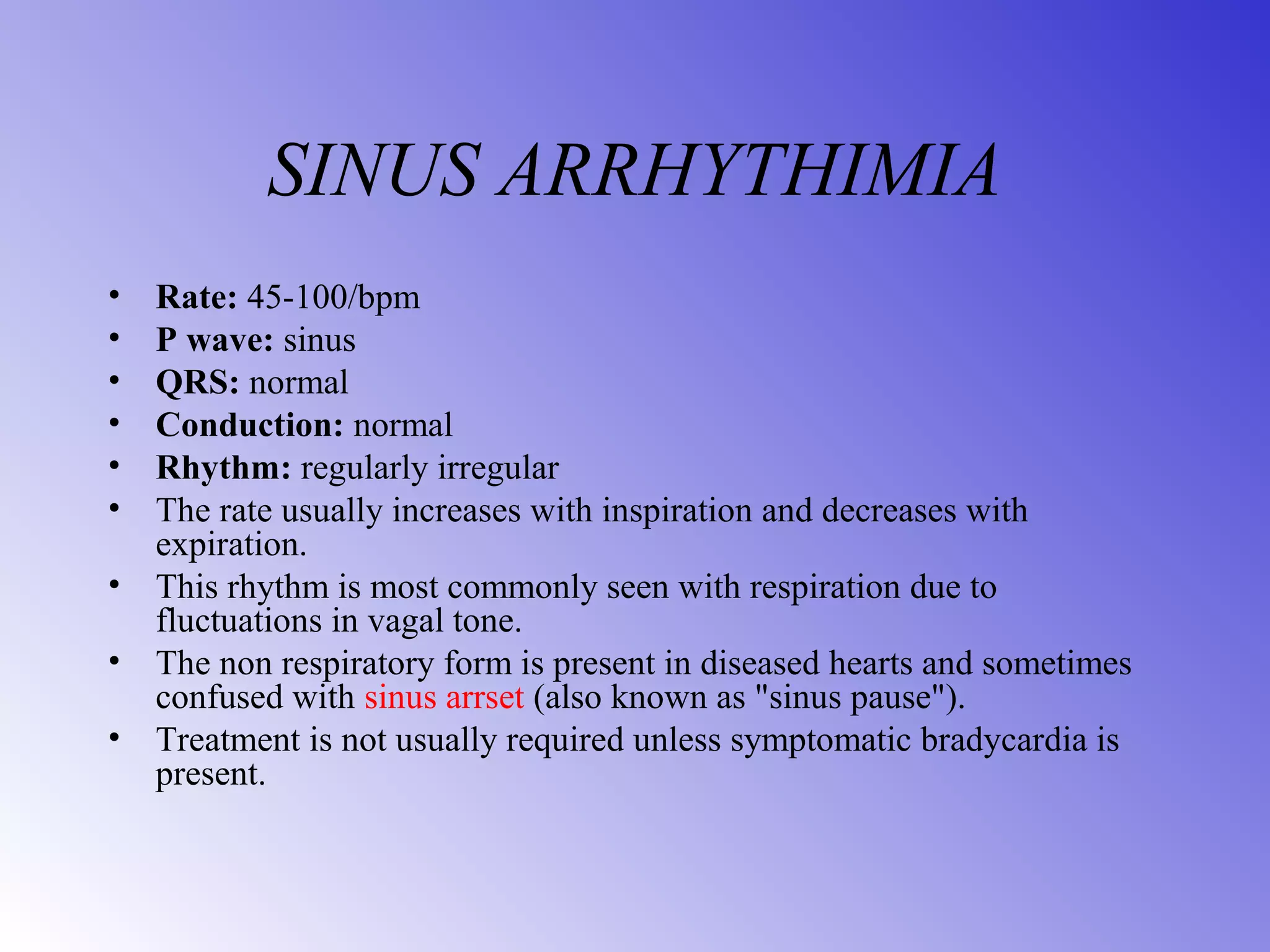
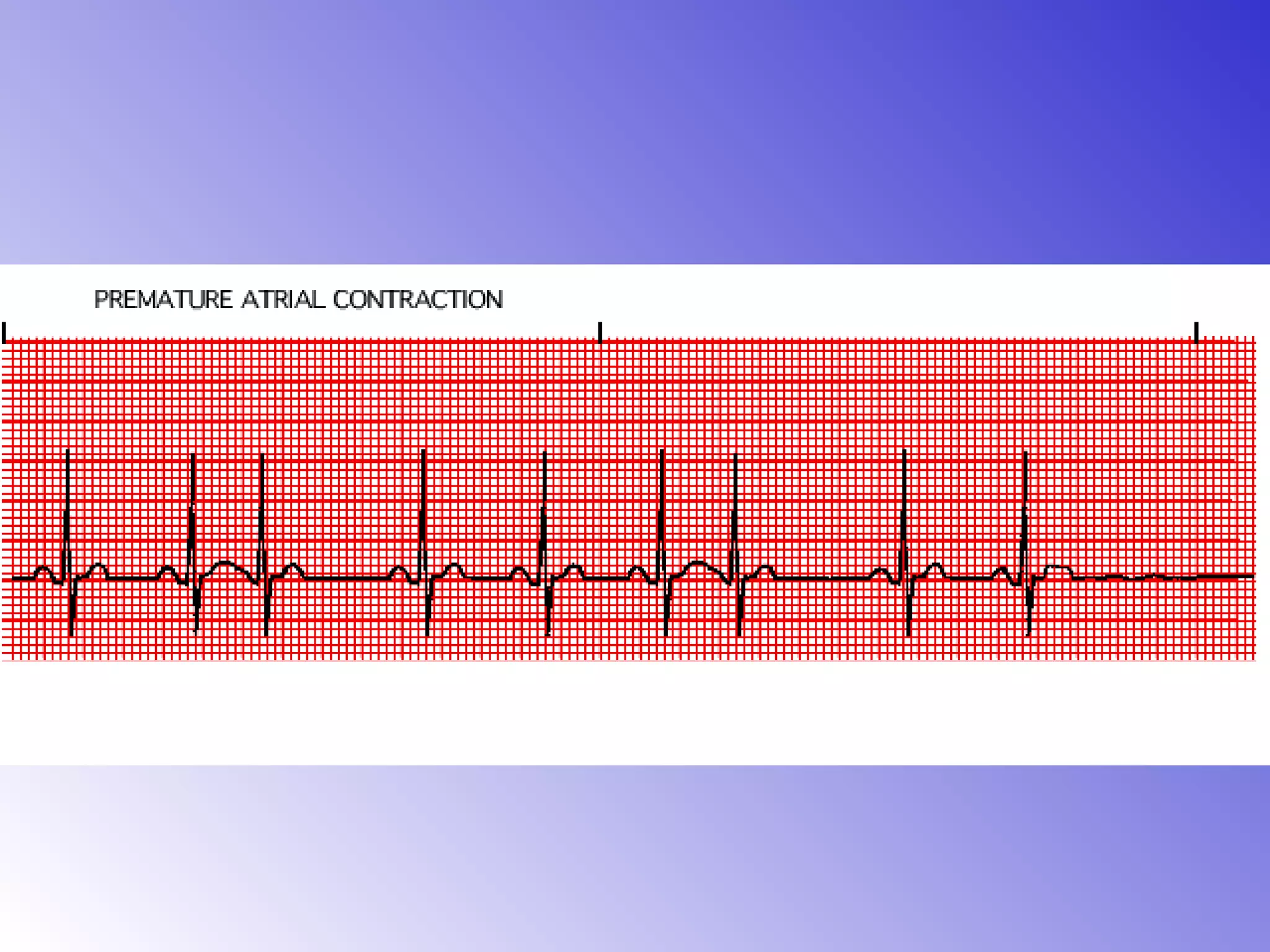
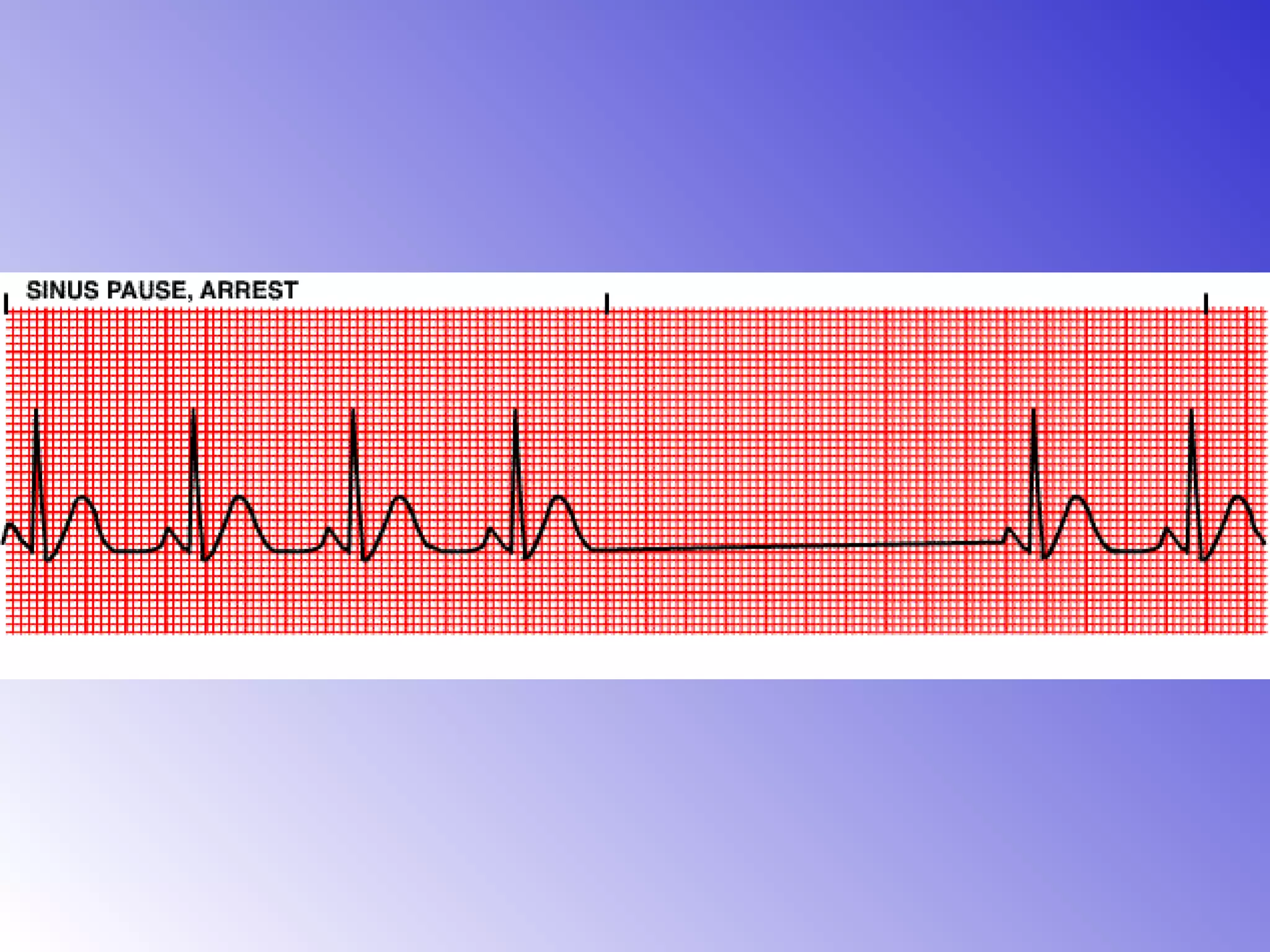
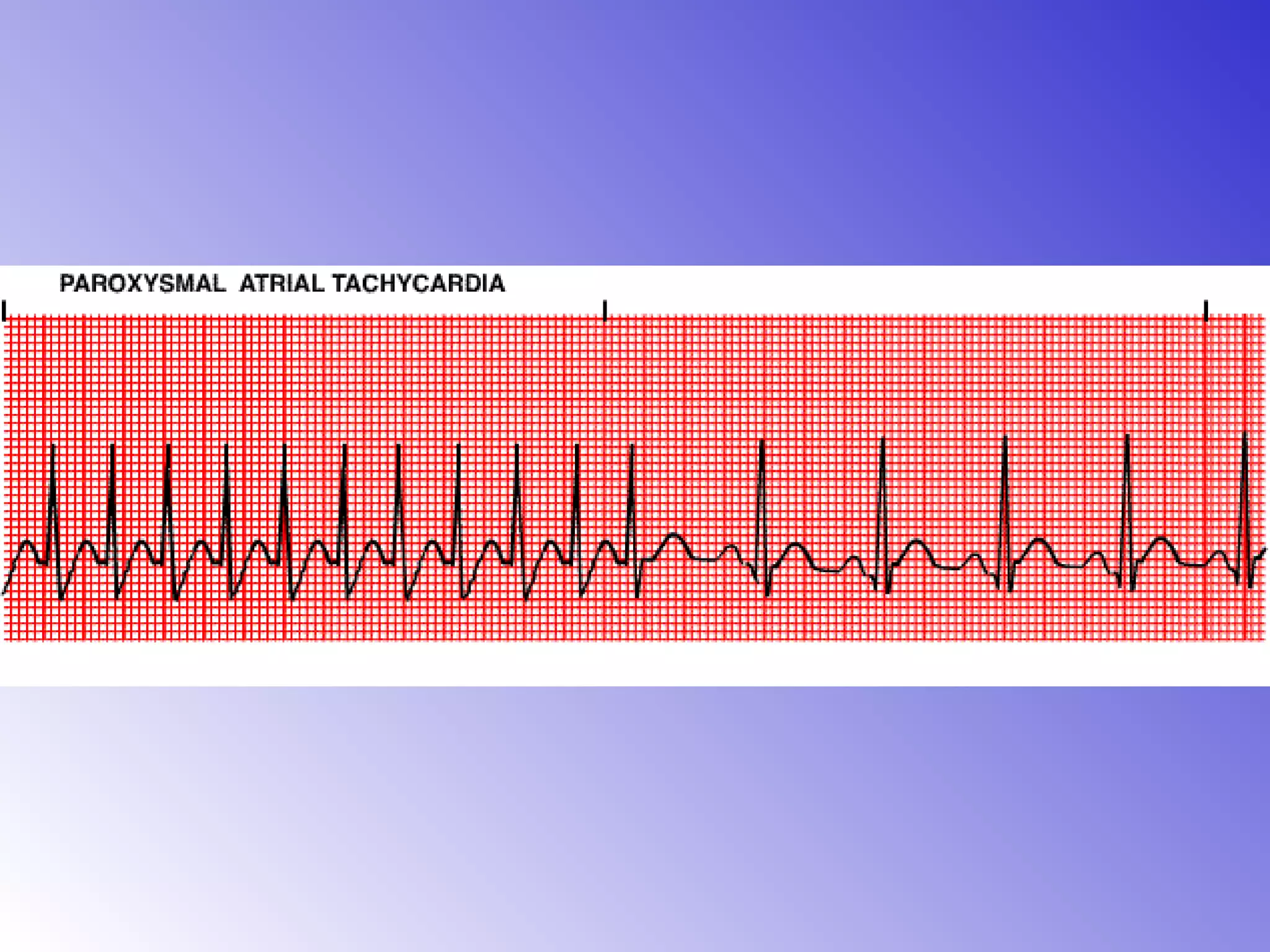
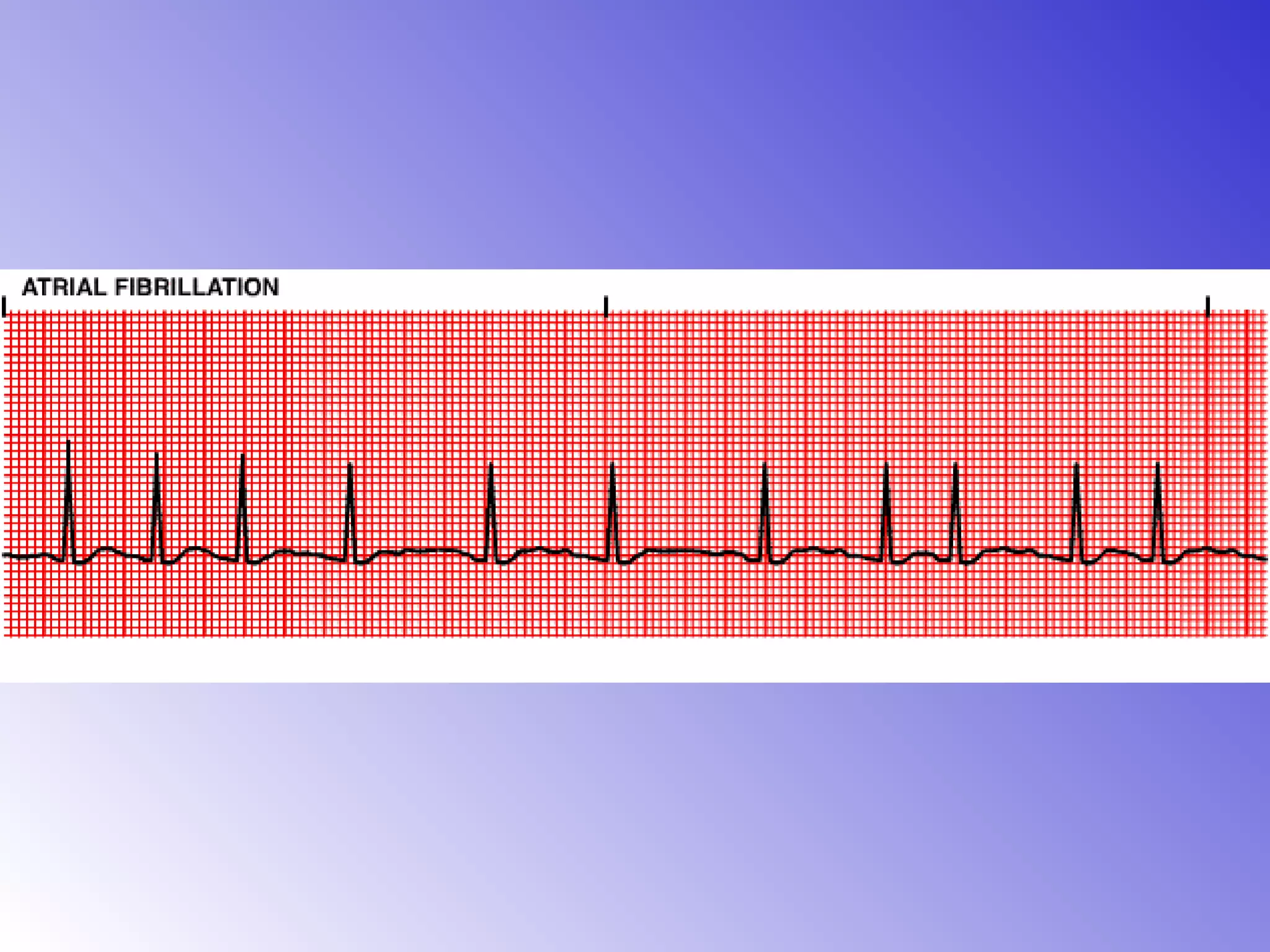
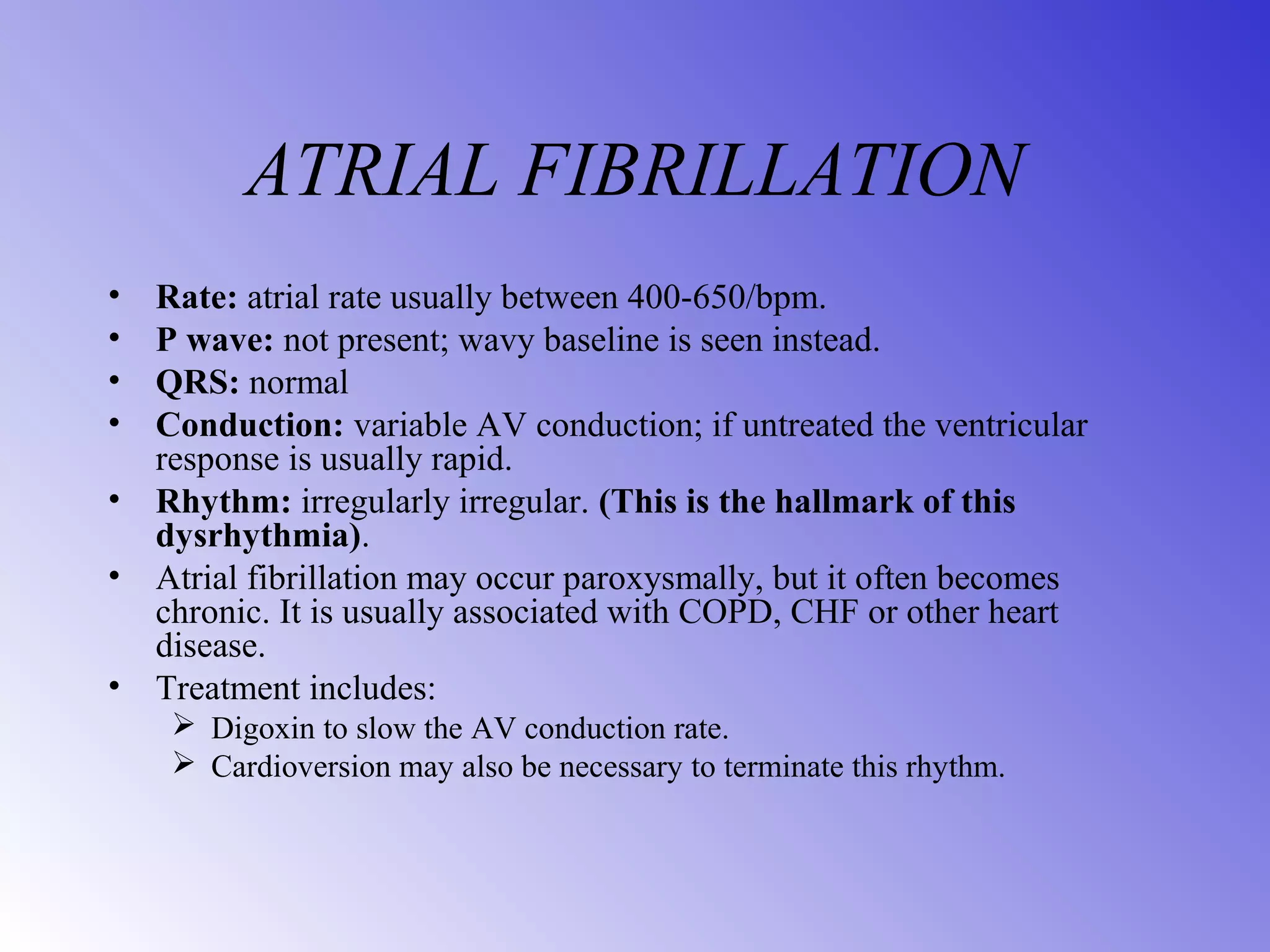
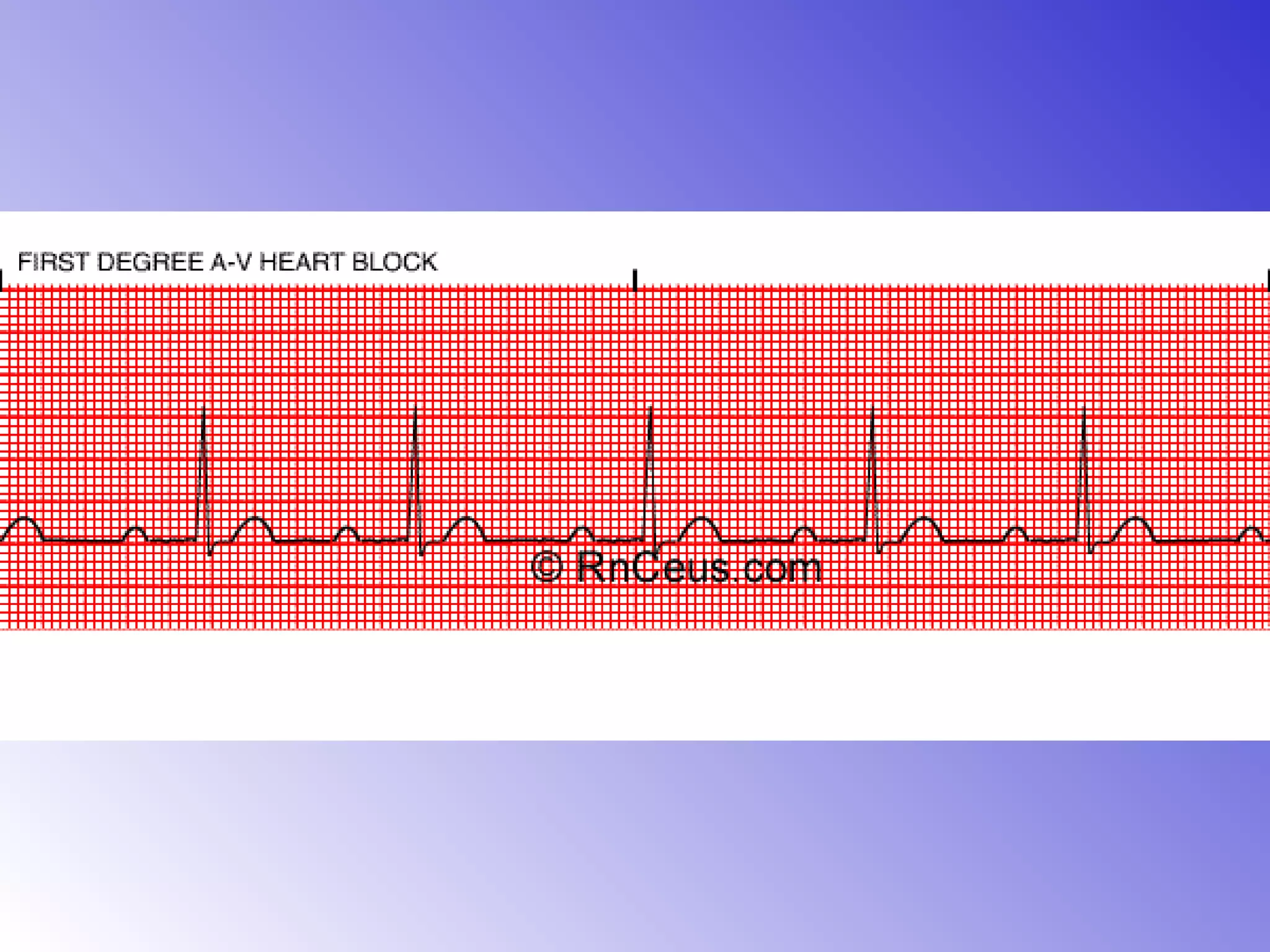
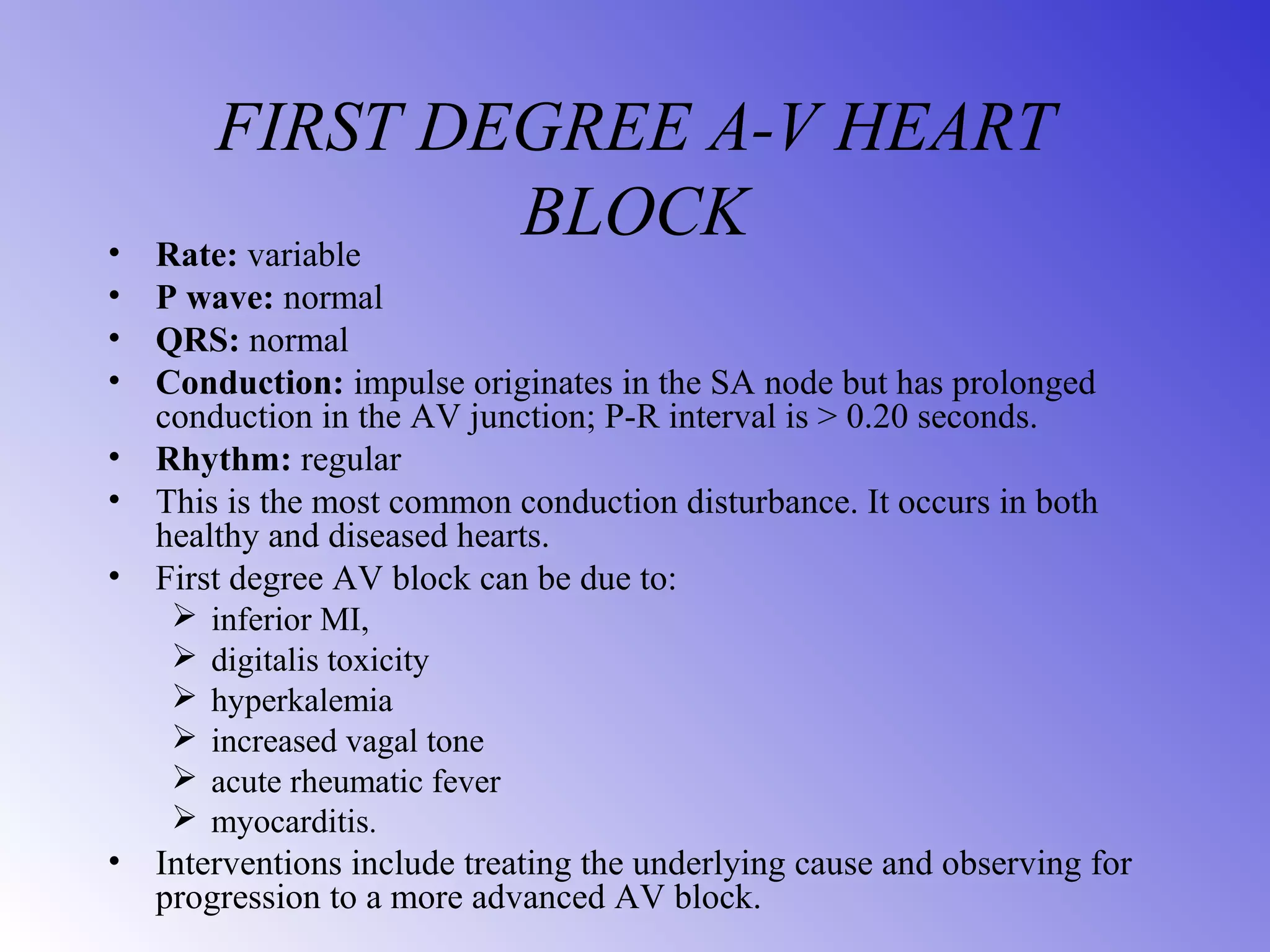
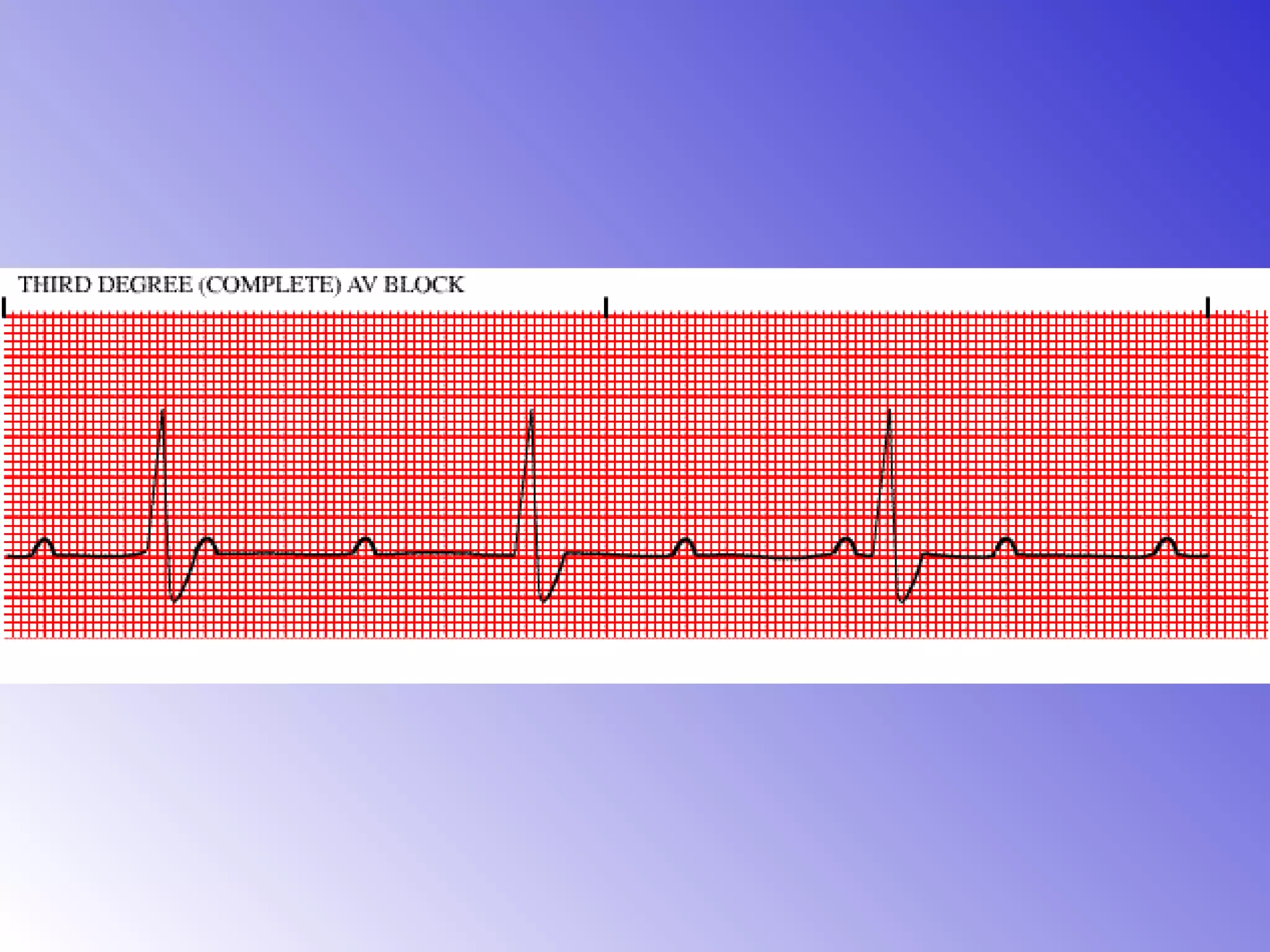
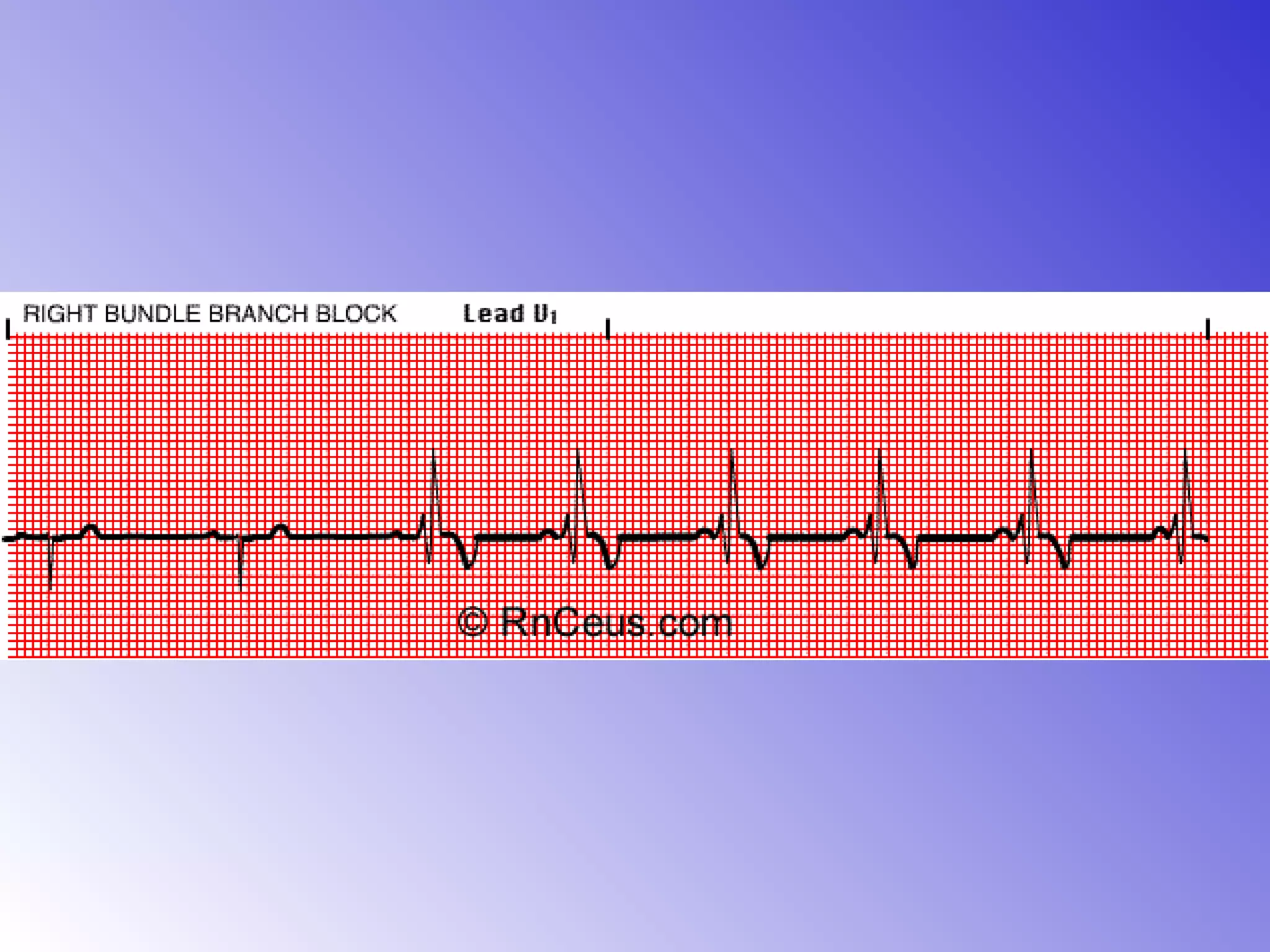
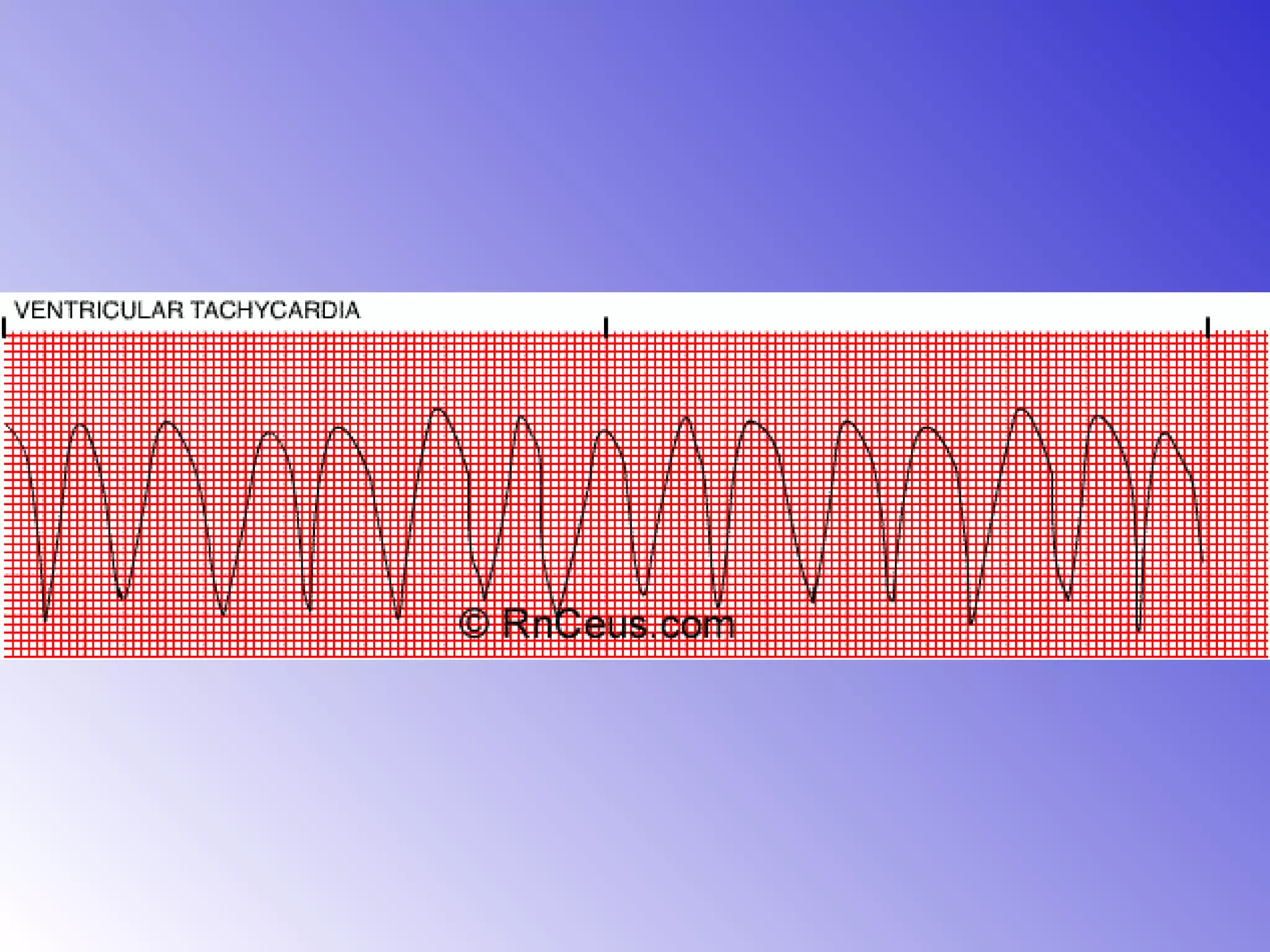
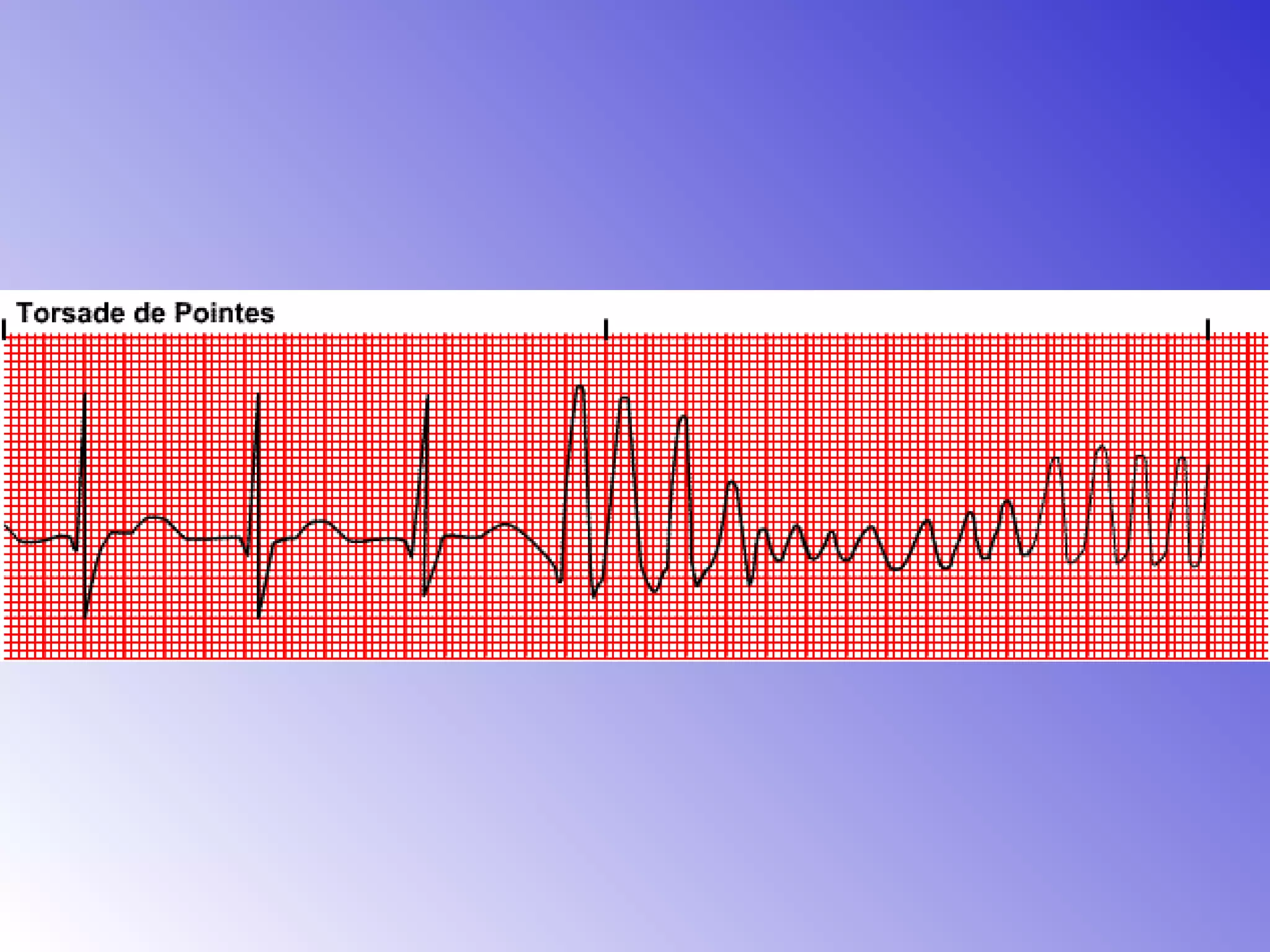
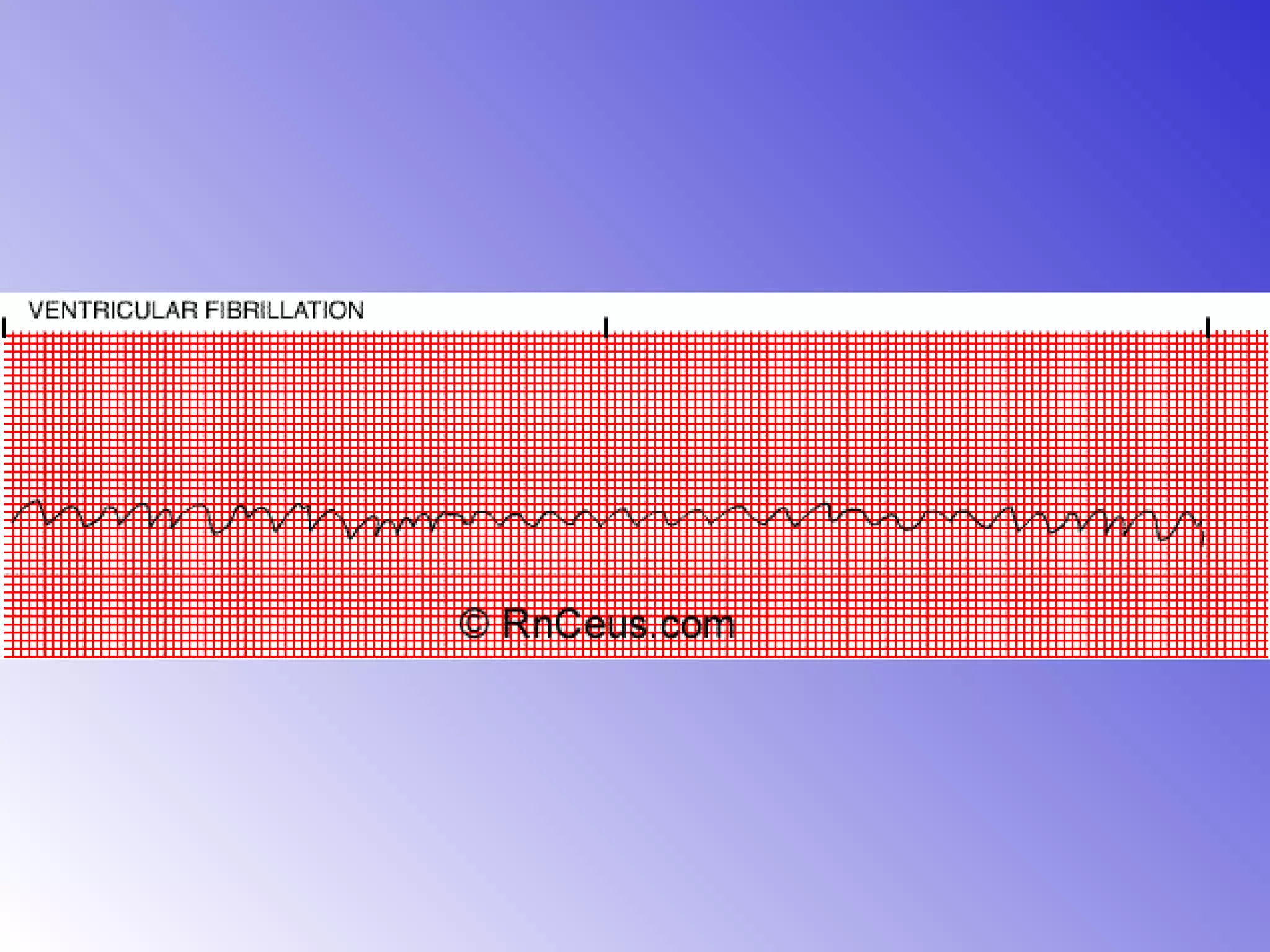
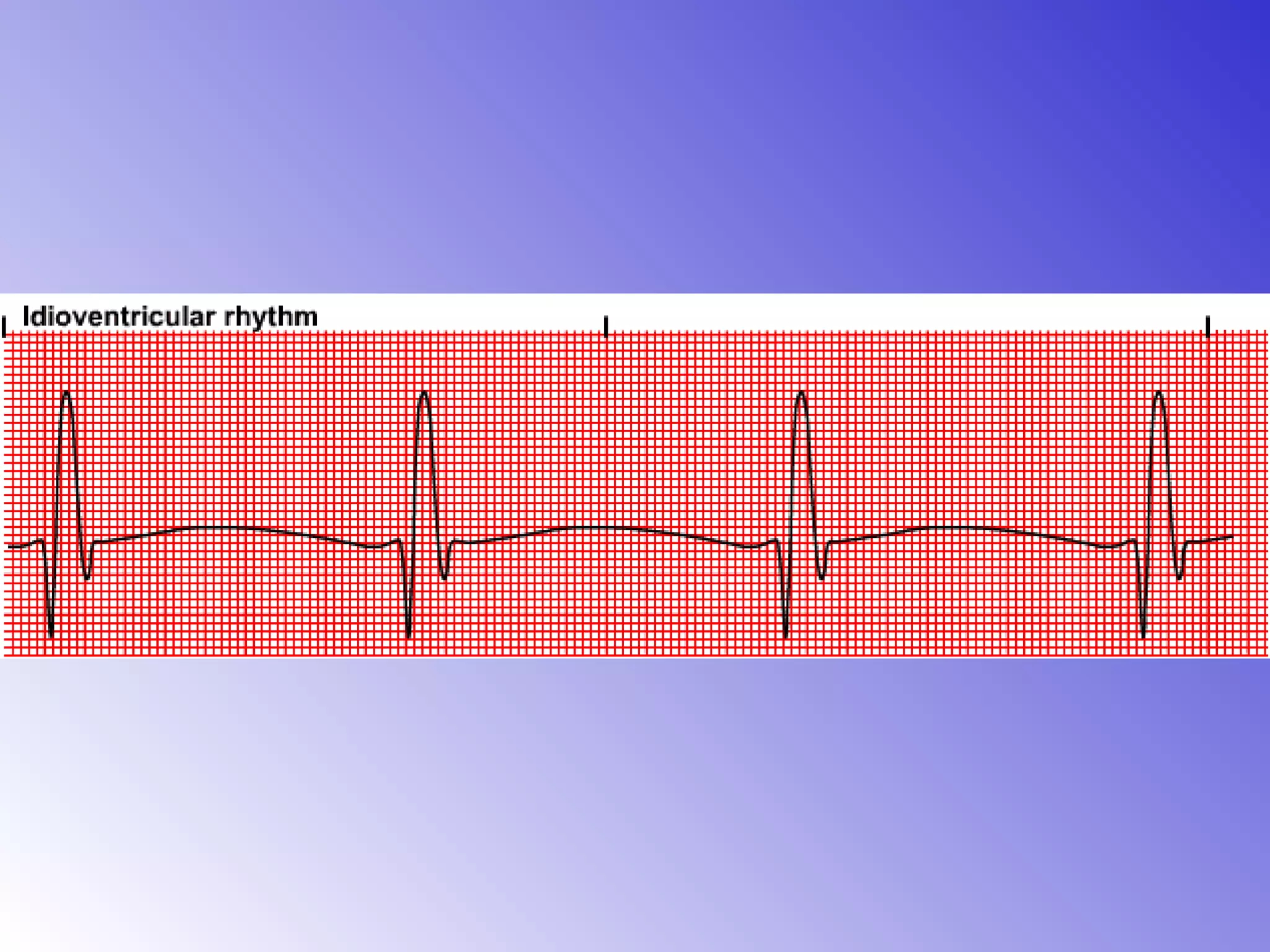
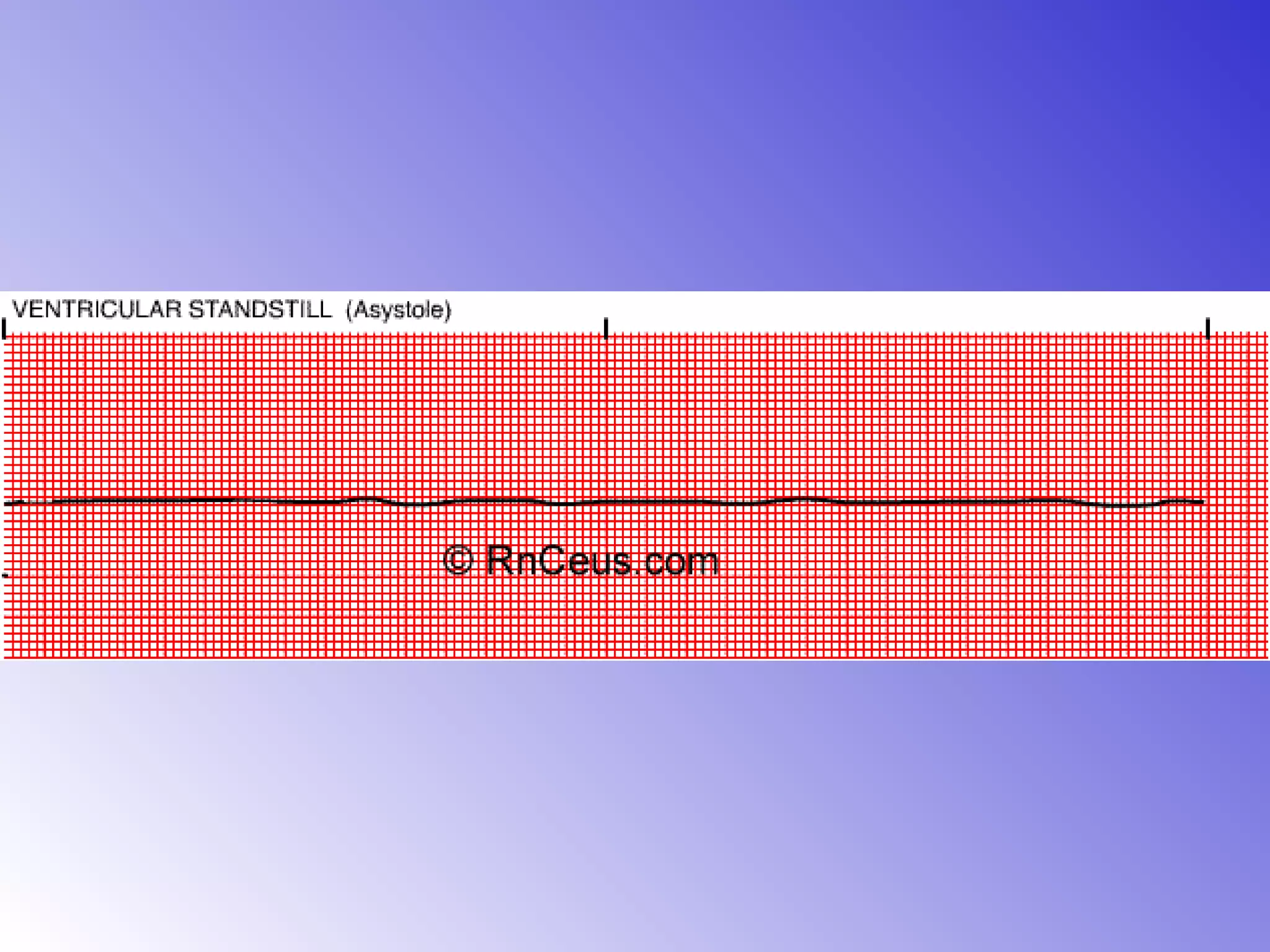
This document provides an overview of various types of arrhythmias including their typical presentation, underlying causes, characteristic ECG patterns, and treatment approaches. Key types are discussed such as sinus tachycardia, atrial fibrillation, various degrees of heart block, premature ventricular contractions, ventricular tachycardia, ventricular fibrillation, and asystole. For each, the rate, P wave, QRS complex, conduction, and rhythm are defined and potential causes and management strategies are outlined. The document serves as a guide for clinicians in identifying and treating different cardiac arrhythmias.