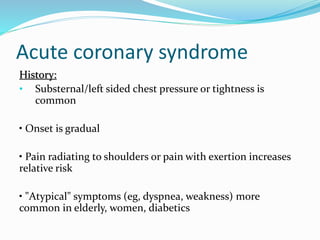
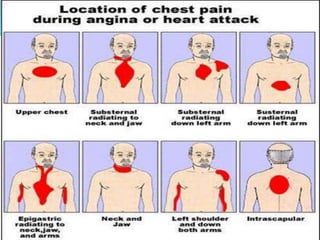
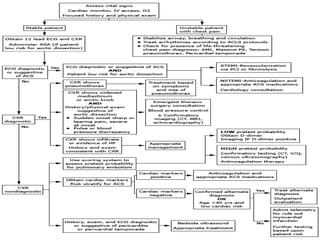
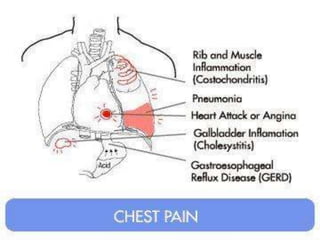
1. Acute coronary syndrome can present with substernal chest pressure, pain radiating to the shoulders, or pain with exertion. ECG may show ST elevations or new left bundle branch block indicating AMI. Troponin and CK-MB elevations are needed to diagnose AMI.
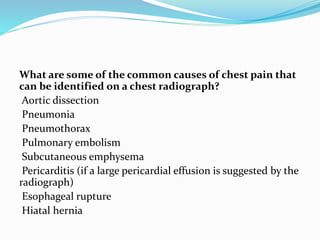
2. Aortic dissection often presents with sudden, severe chest pain and may be suggested on ECG by discrepancies in blood pressure between arms or signs of ischemia. Chest X-ray may show a widened mediastinum.
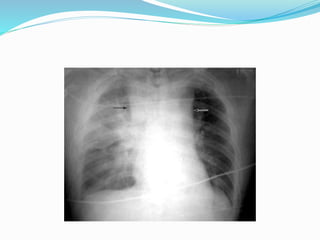
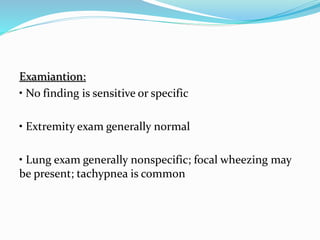
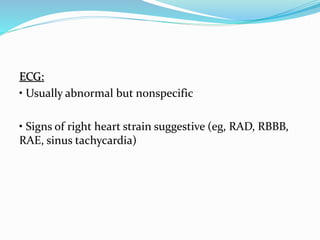
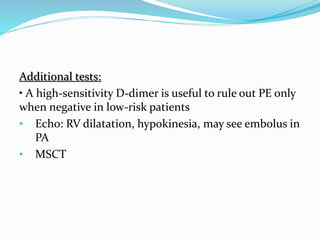
3. Pulmonary embolism presentations can vary widely but often include dyspnea. ECG may show signs of right heart strain. Most chest X-rays are normal but some show