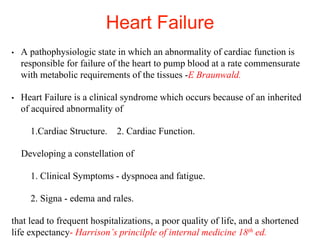
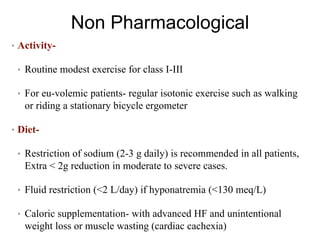
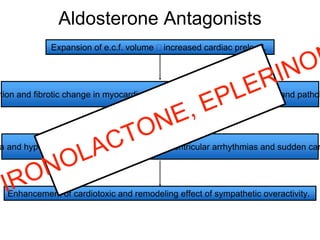
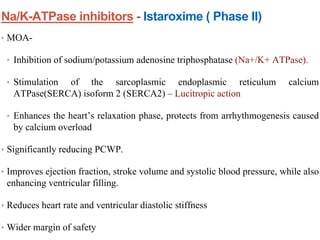
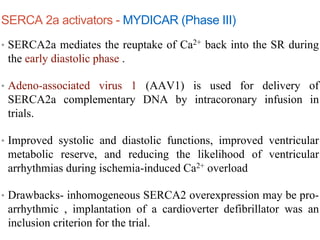
This document provides an overview of recent advances in the pharmacotherapy of congestive cardiac failure (CCF). It discusses the definition, epidemiology, classification, etiology and pathophysiology of heart failure. It then examines the signs and symptoms and management approaches, including both non-pharmacological and pharmacological measures. The pharmacological section focuses on the mechanisms of action of common drug classes used to treat CCF, such as diuretics, ACE inhibitors, beta-blockers, aldosterone antagonists, and inotropic drugs.