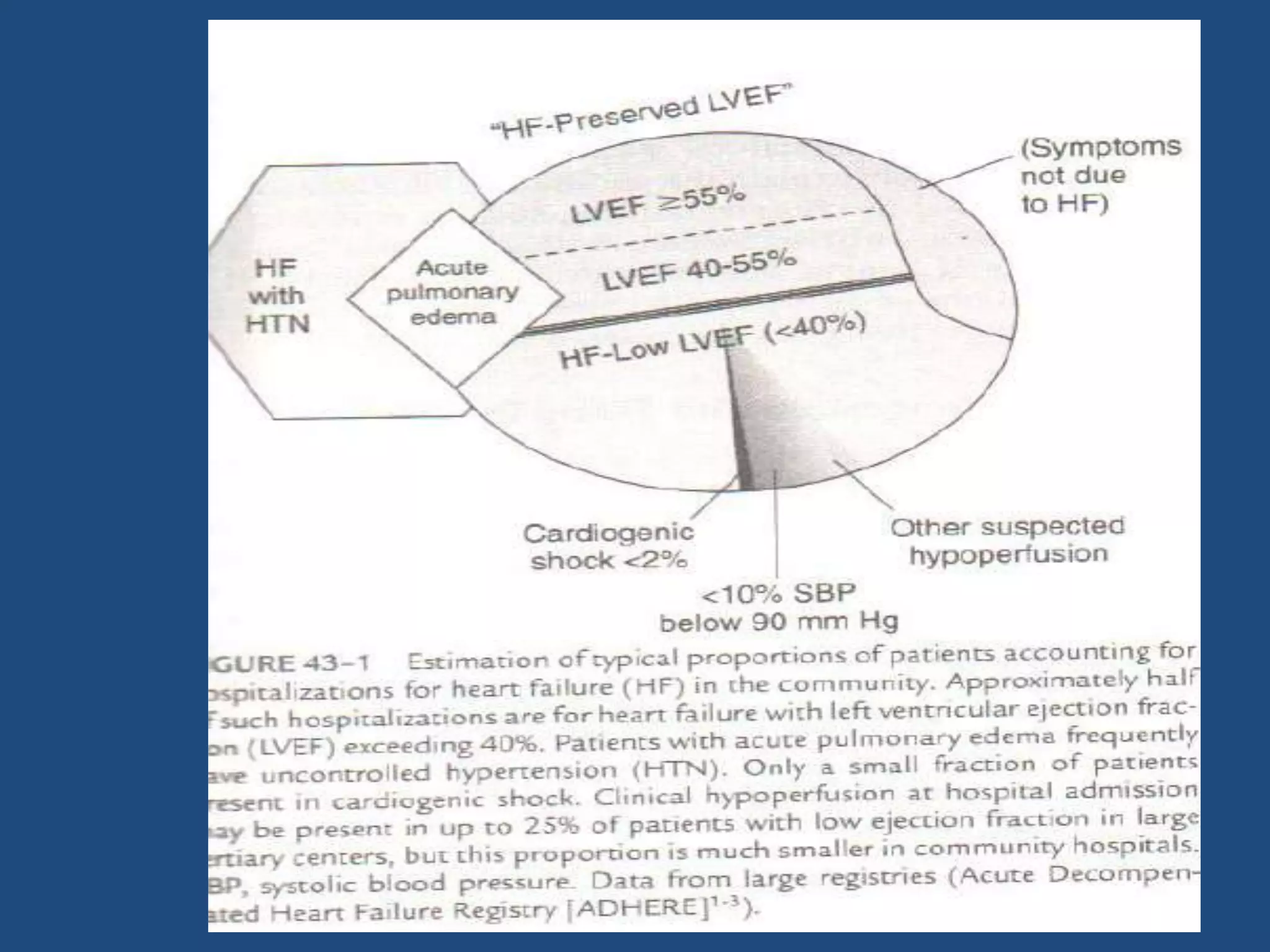
This document discusses the management of acute decompensated heart failure (ADHF). It outlines assessing patients for ADHF through clinical signs and symptoms, initial investigations including ECG, labs, and imaging. Treatment involves immediate relief of symptoms through intensive monitoring and care, identifying precipitating causes, stabilizing the patient, and modifying medical therapy which may include diuretics, vasodilators, inotropes, and managing underlying conditions. Goals include symptom relief, hemodynamic monitoring, addressing congestion or hypoperfusion, and developing discharge plans.