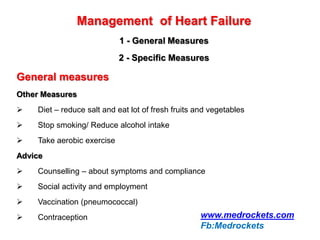
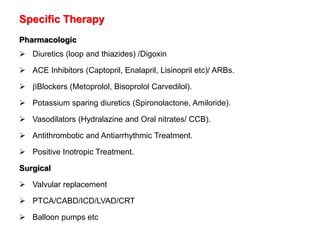
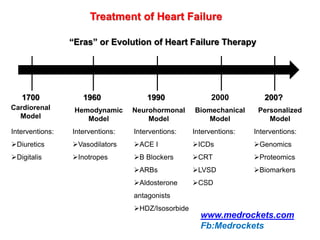
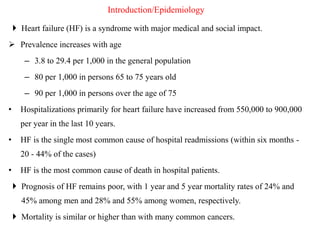
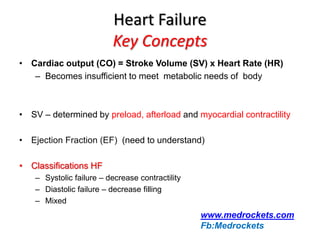
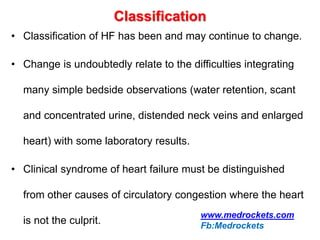
Heart failure is a common and serious condition where the heart muscle is unable to pump sufficiently. It can have multiple causes and the prevalence increases significantly with age. Prognosis remains poor with high mortality rates. Diagnosis involves evaluating symptoms, signs, and testing like echocardiogram. Management focuses on general measures like diet, exercise, and reducing risk factors as well as specific treatments targeting the underlying cause and physiology of heart failure.
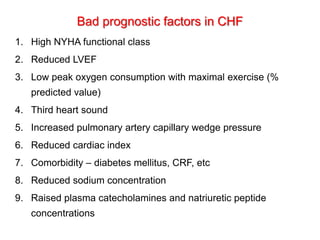
![Terminology
Congestive Heart Failure: Similar to the preceding but with features
of circulatory congestion such as jugular venous distention, rales,
peripheral edema and ascites.
Compensated Heart Failure: Is used in reference to patients with
chronic heart failure whose symptoms and signs of pulmonary or
peripheral congestion are relieved by therapy, although, the EDV and
EDP often remain elevated and the EF remains reduced.
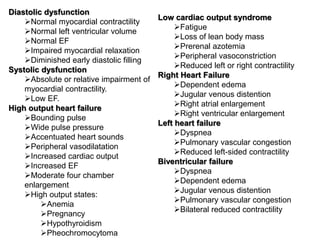
Systolic Heart Failure: Reflects a decrease in normal emptying
capacity [usually with an EF < 45 %] that is usually associated with a
compensatory increase in diastolic volume.
Diastolic Heart Failure: Is said to be present when the filling of one
or both ventricles is impaired, while the emptying capacity is normal.](https://image.slidesharecdn.com/heartfailure-180110155110/85/Heart-failure-7-320.jpg)
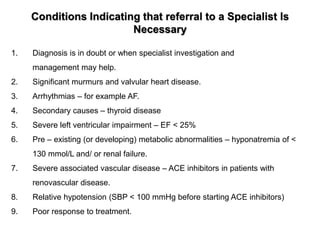
![NYH Association Functional Classification [NYHA]
Class I: Asymptomatic- Patients with cardiac disease but without resulting limitations of
physical activity, i.e., ordinary physical activity does not cause undue fatigue, palpitation,
dyspnea or anginal pain.
Class II: Mild- Patients with cardiac disease resulting in slight limitation of physical activity.
These patients are comfortable at rest. Ordinary physical activity results in fatigue,
palpitation, dyspnea or anginal pain.
Class III: Moderate - Patients with cardiac disease resulting in marked limitation of physical
activity. These patients are comfortable at rest. Less than ordinary physical activity
causes fatigue, palpitation, dyspnea or anginal pain.
Class IV: Severe - Patients with cardiac disease resulting in inability to carry on any physical
activity without discomfort. Symptoms of cardiac insufficiency or of the anginal syndrome
may be present even at rest. If any physical activity is undertaken, discomfort is
increased.](https://image.slidesharecdn.com/heartfailure-180110155110/85/Heart-failure-15-320.jpg)