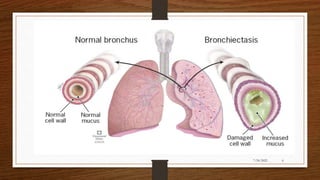
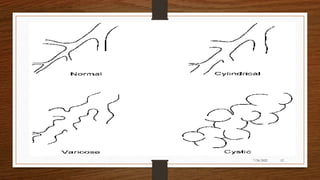
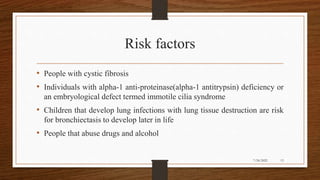
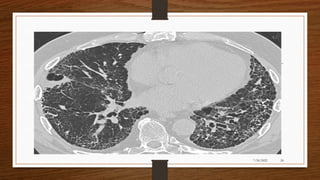
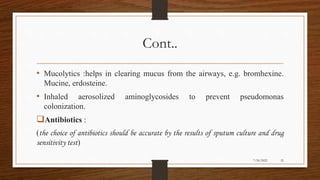
Bronchiectasis is a chronic lung disease characterized by irreversible dilation of the bronchi. It results from damage to the airways due to infection or inflammation that impairs mucus clearance. Common symptoms include chronic cough with sputum production. Diagnosis involves chest imaging and sputum culture. Treatment aims to clear secretions, treat infections, and manage symptoms. Nursing care focuses on airway clearance techniques, breathing exercises, infection control, nutrition support, and health education.