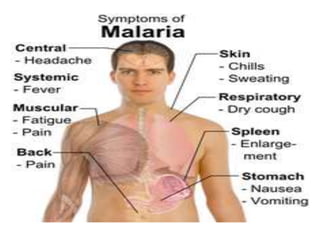
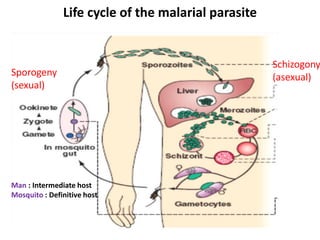
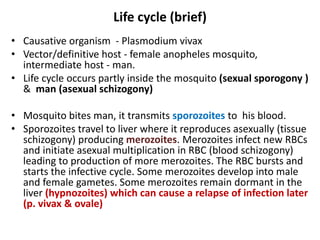
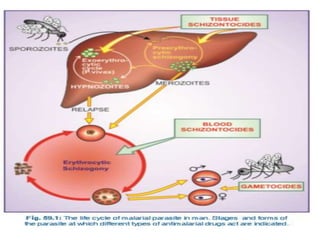
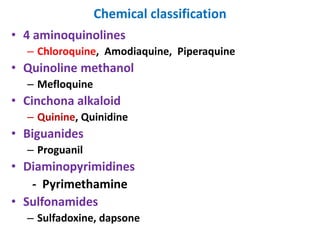
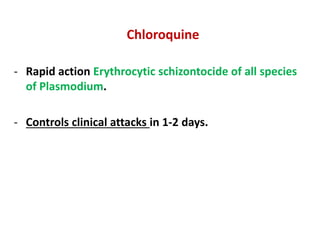
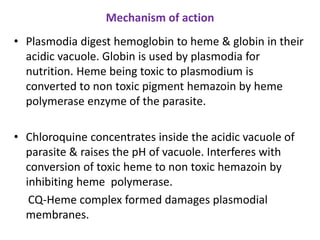
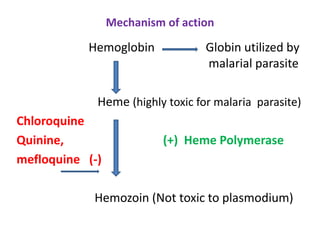
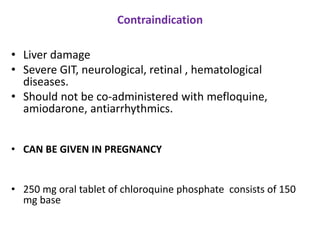
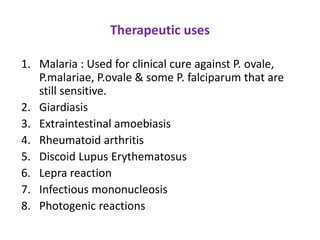
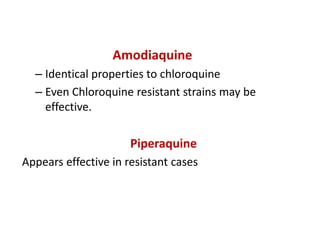
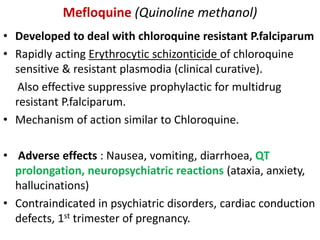
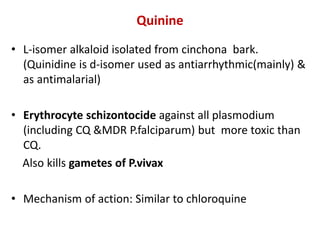
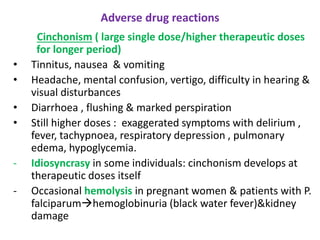
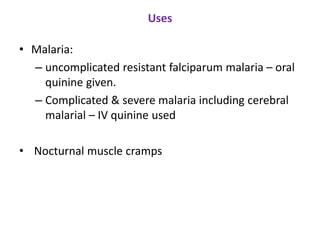
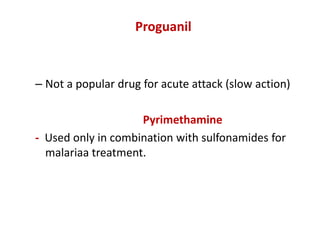
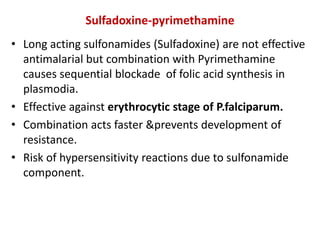
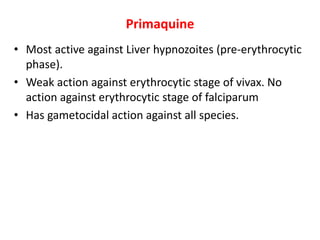
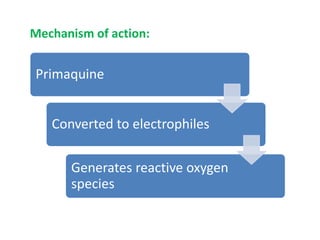
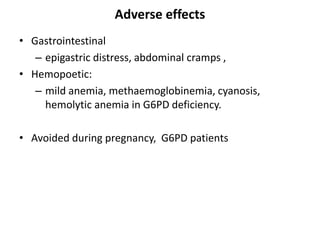
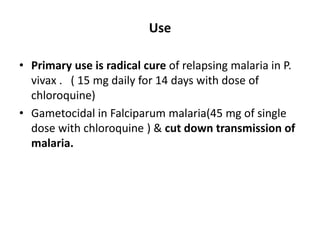
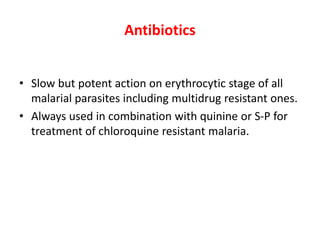
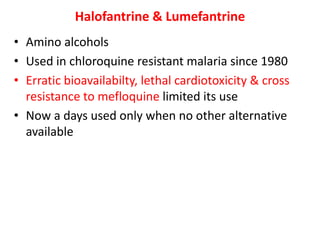
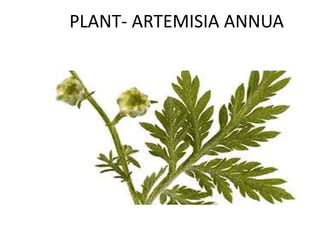
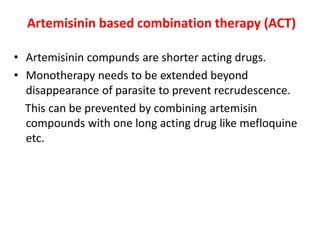
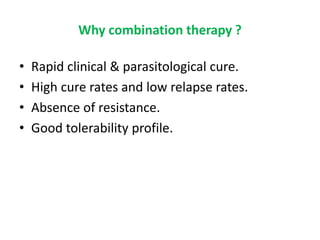
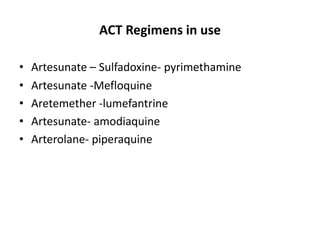
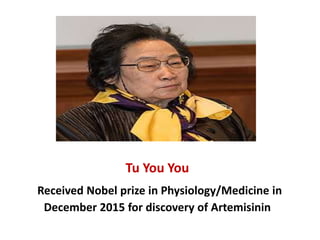
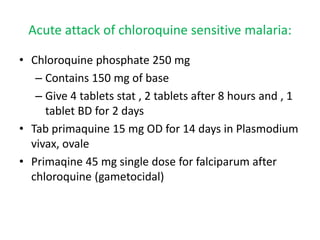
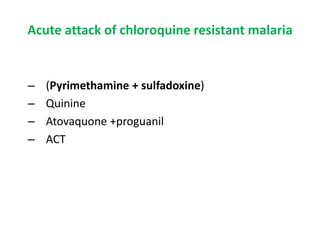
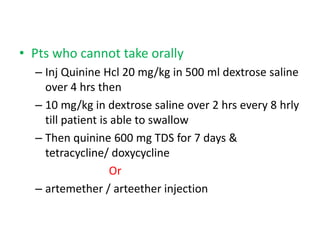
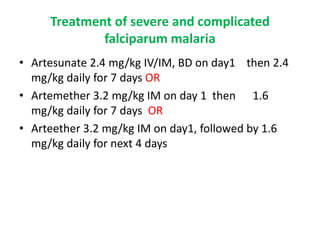
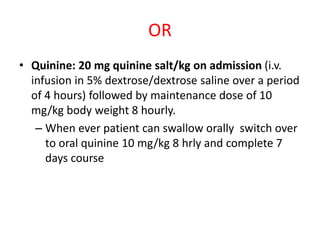
This document discusses antimalarial drugs. It begins by introducing malaria and its causative parasites. It then describes the life cycle of the malaria parasite, involving stages in both the human host and mosquito vector. The objectives and classifications of antimalarial drugs are outlined. Key drugs like chloroquine, primaquine, quinine, and artemisinins are then described in detail, including their mechanisms of action, uses, and adverse effects. Combination therapies using artemisinins are emphasized as the most effective strategy to prevent drug resistance from emerging.