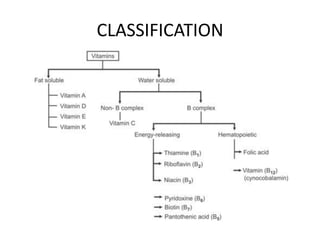
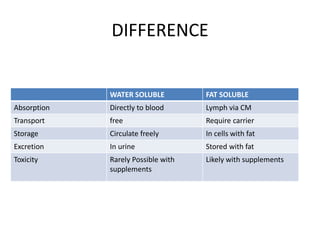
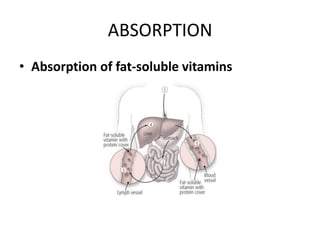
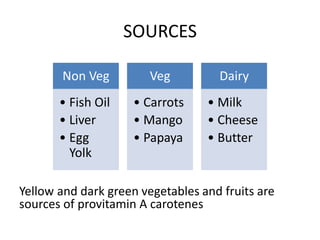
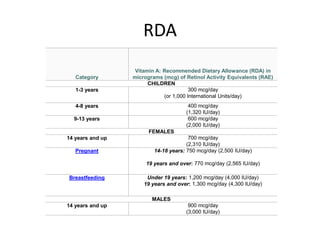
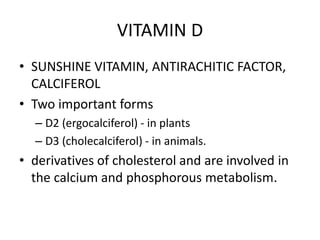
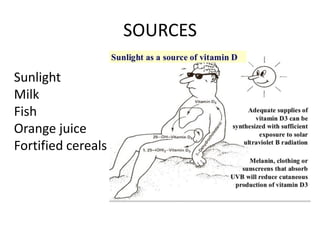
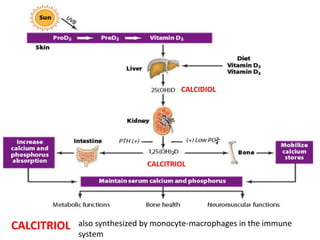
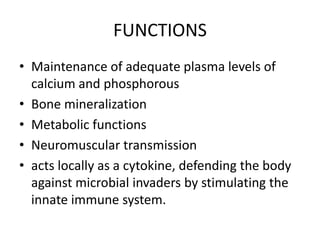
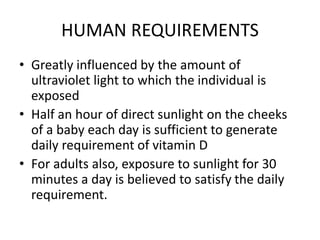
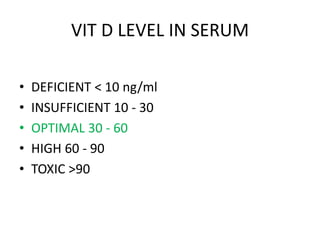
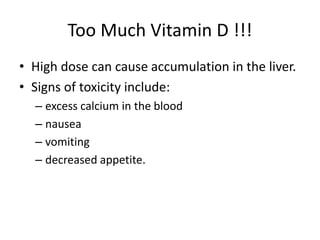
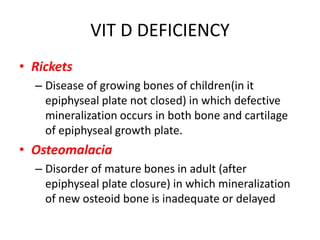
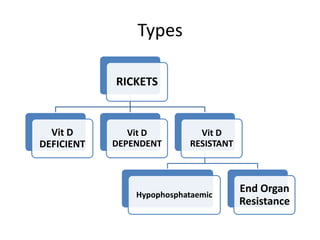
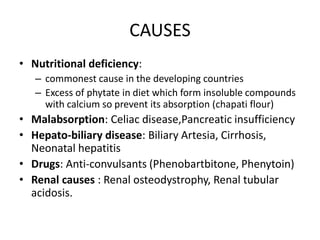
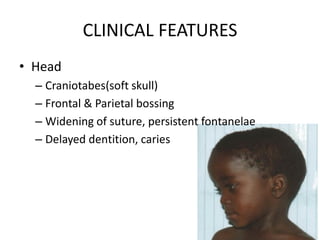
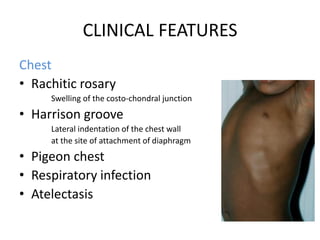
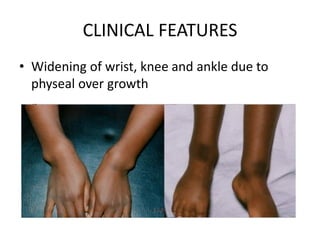
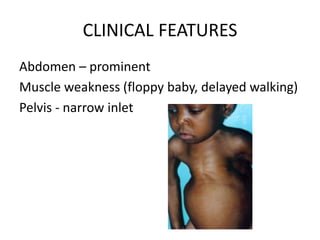
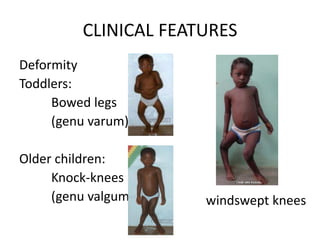
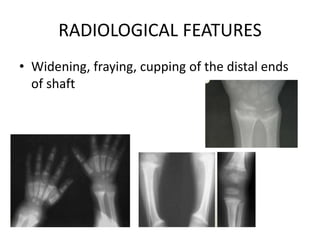
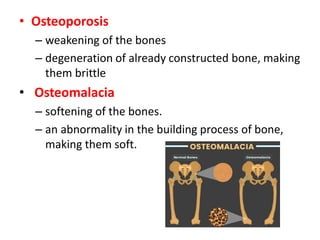
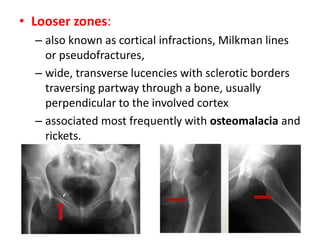
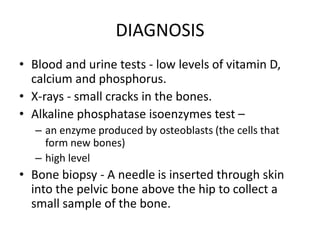
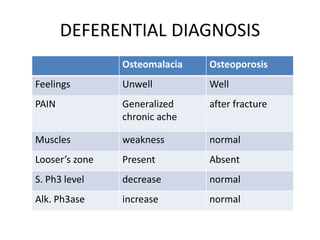
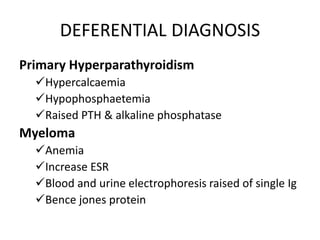
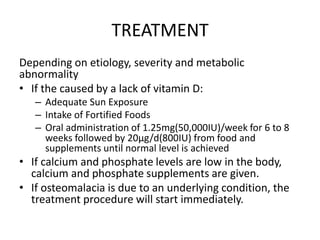
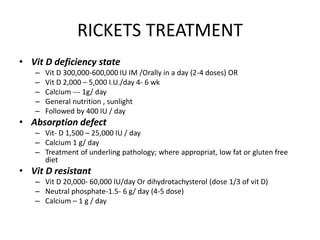
This document provides information on vitamins A and D, including their classification, sources, functions, deficiencies, and more. It begins with an introduction to vitamins and their classification as either fat-soluble (A, D, E, K) or water-soluble (C and B complex). Specific details are given for vitamin A and D, including dietary sources, recommended daily allowances, absorption, roles in bone health and vision, deficiency diseases like rickets and osteomalacia, and treatment. The summary concludes with prevention through a healthy diet and vitamin D synthesis from sunlight.