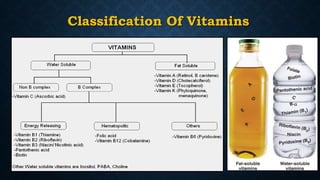
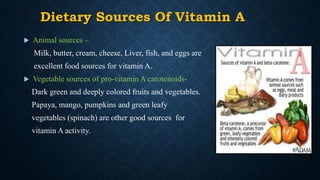
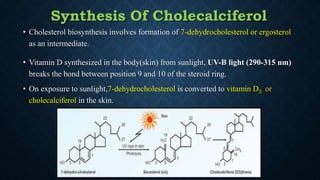
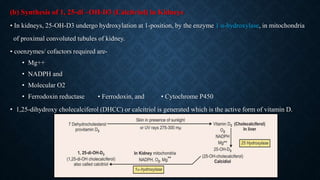
Vitamins are organic nutrients essential for various biochemical functions and must be acquired through diet, classified as fat-soluble (A, D, E, K) or water-soluble (B, C). This document details the chemistry, functions, and deficiencies of vitamins A and D, highlighting their crucial roles in vision, growth, and calcium metabolism. It also discusses recommended dietary allowances, sources, and the consequences of vitamin deficiencies and hypervitaminosis.