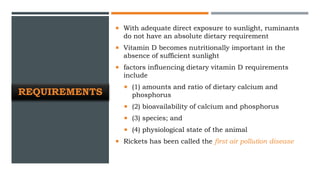
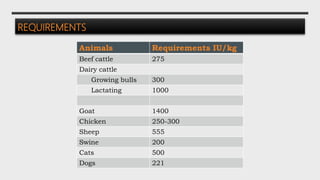
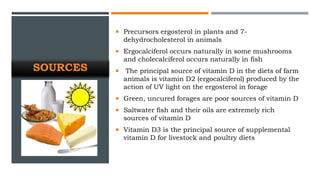
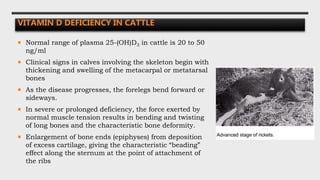
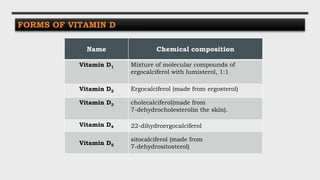
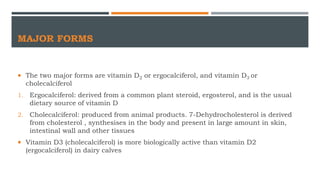
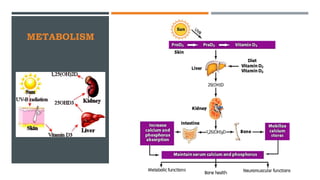
This document discusses vitamin D, including its types, metabolism, absorption, storage, functions, requirements, sources, deficiency, and toxicity. The two major forms are vitamins D2 and D3. Vitamin D is absorbed in the small intestine and transported to the liver and kidney where it is converted to its active form, 1,25-dihydroxyvitamin D. This active form regulates calcium and phosphorus absorption in the intestine and their deposition in bone. Requirements vary by species but adequate sunlight can meet animal requirements. Deficiency causes rickets in young animals due to poor bone mineralization.
![CONVERSION OF METABOLICALLY ACTIVE FORM
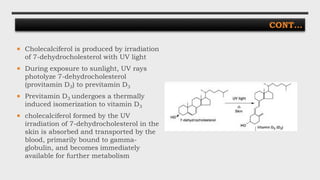
In the liver, the microsomal system
hydroxylates the 25-position carbon in the side
chain to produce 25-hydroxy-vitamin D3 [25-
(OH)D3]
25-(OH)D3 is then transported to the kidney on
the vitamin D transport globulin, where it can
be converted in the proximal convoluted cells
to 1,25-dihydroxy-vitamin D [1,25-(OH)2D3]
1,25-(OH)2D3 is then transported to the
intestine, bones or elsewhere in the body,
where it is involved in the metabolism of
calcium and phosphorus
Hormonal form, 1,25-(OH)2D3, is the
metabolically active form of the vitamin that
functions in intestine and bone](https://image.slidesharecdn.com/vitd-190903201623/85/Vitamin-D-9-320.jpg)