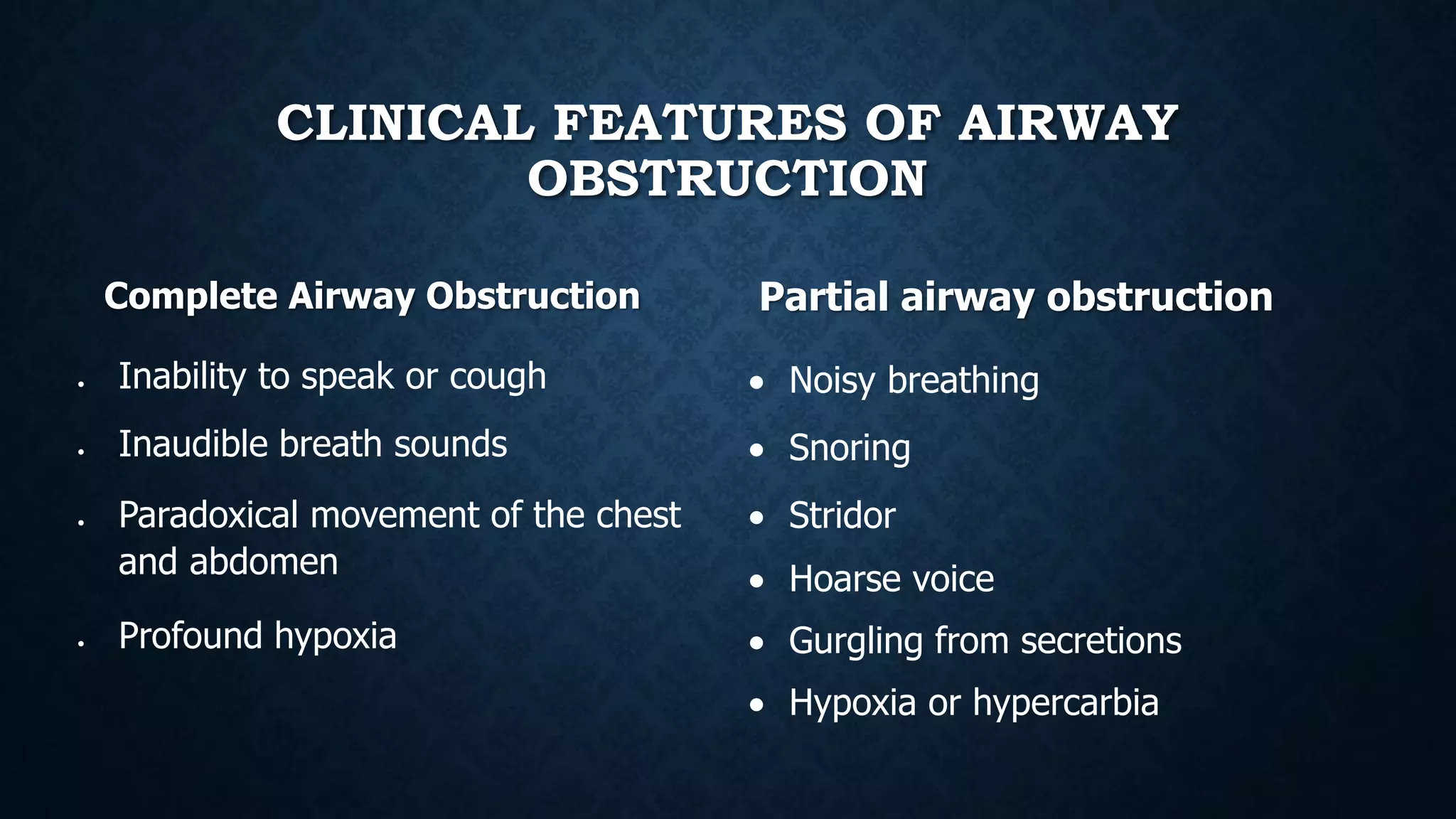
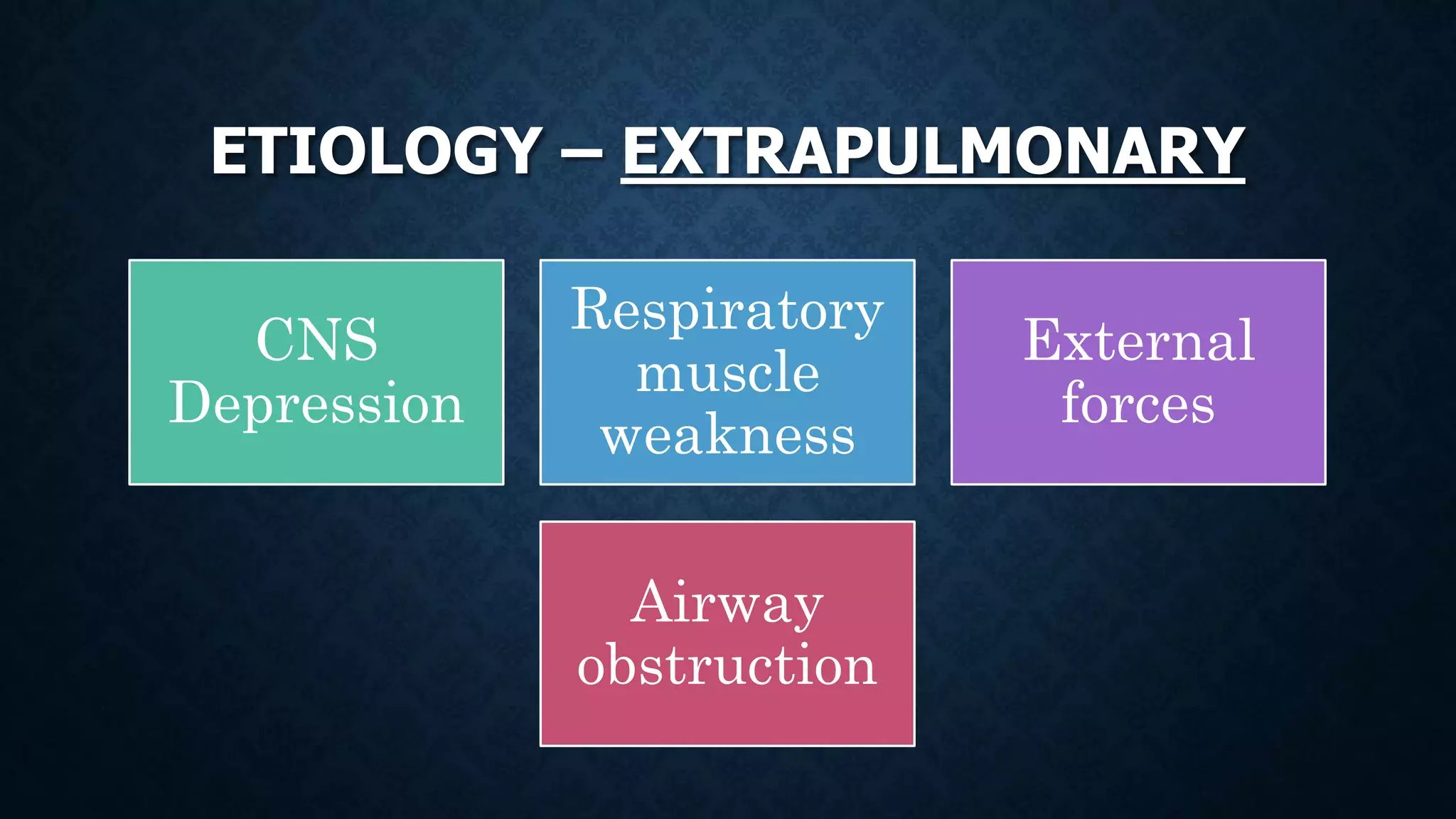
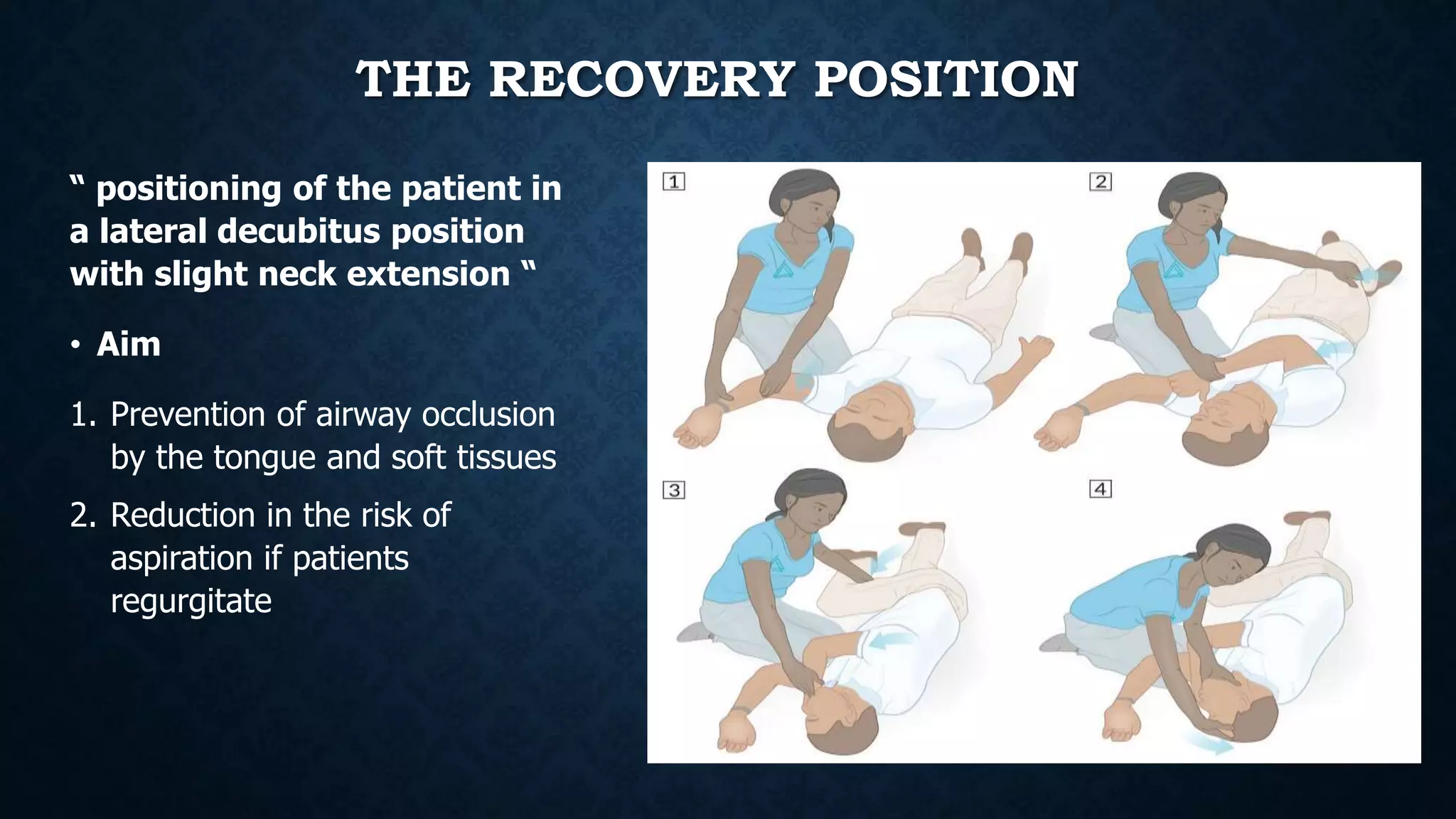
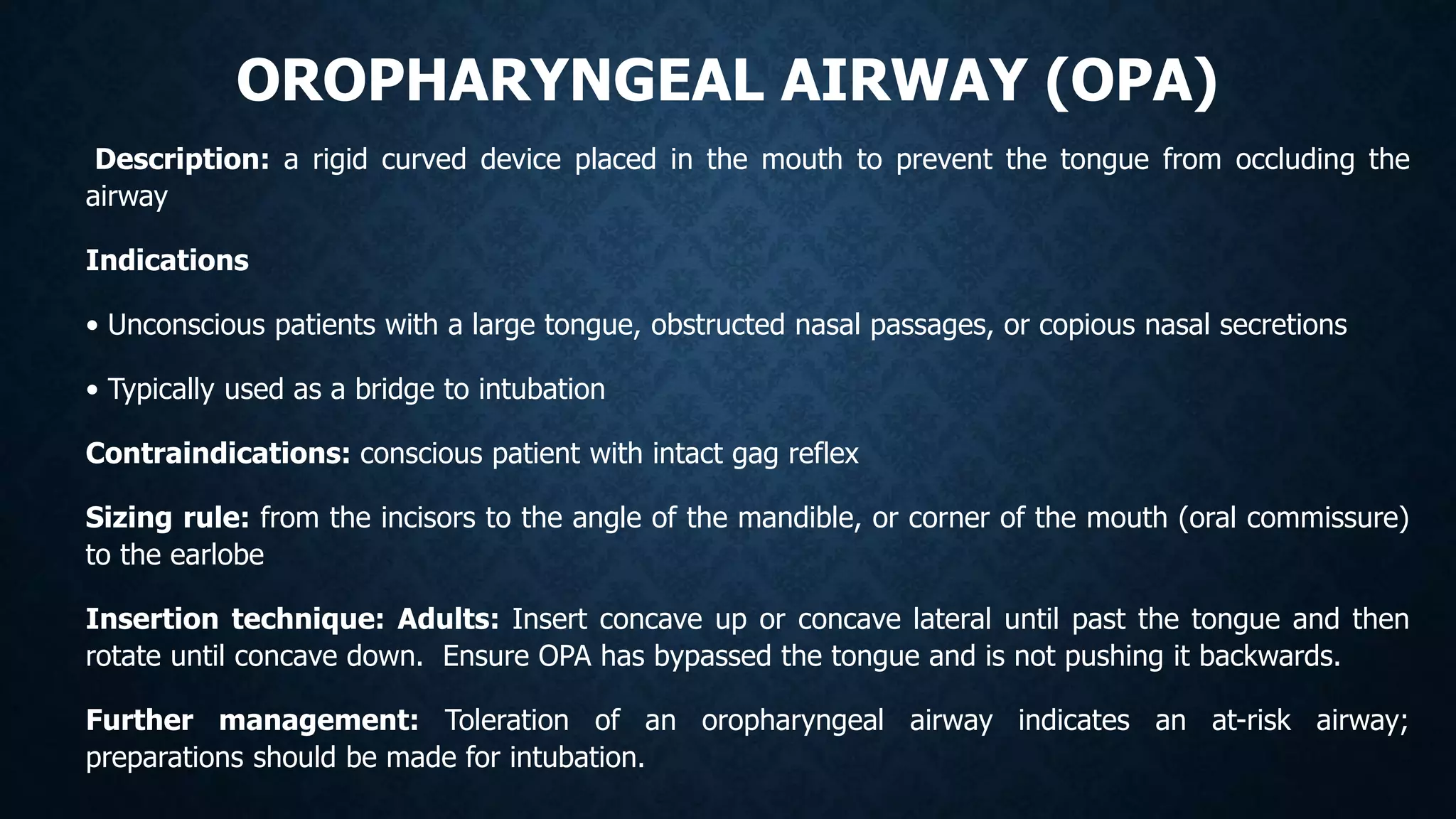
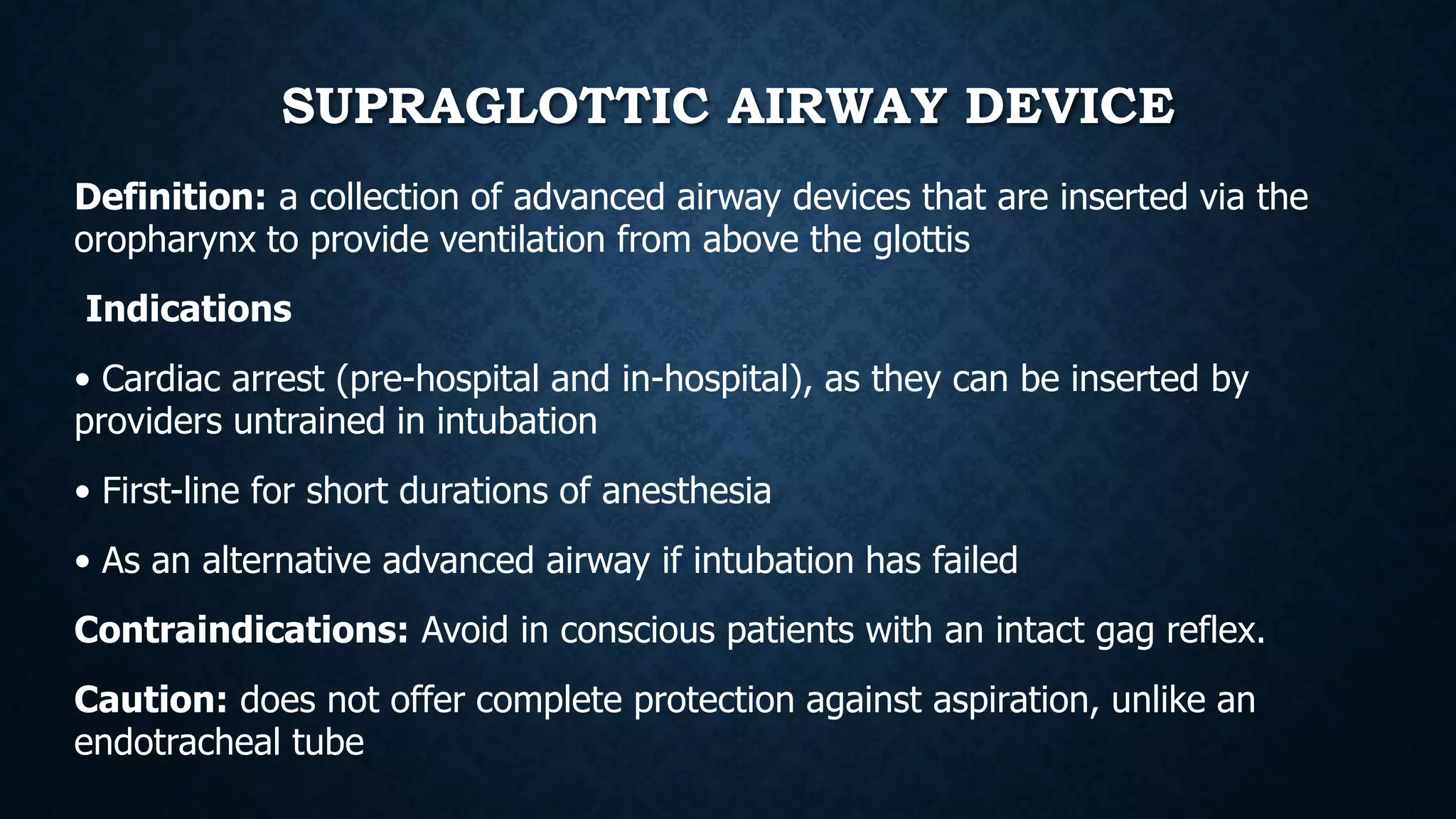
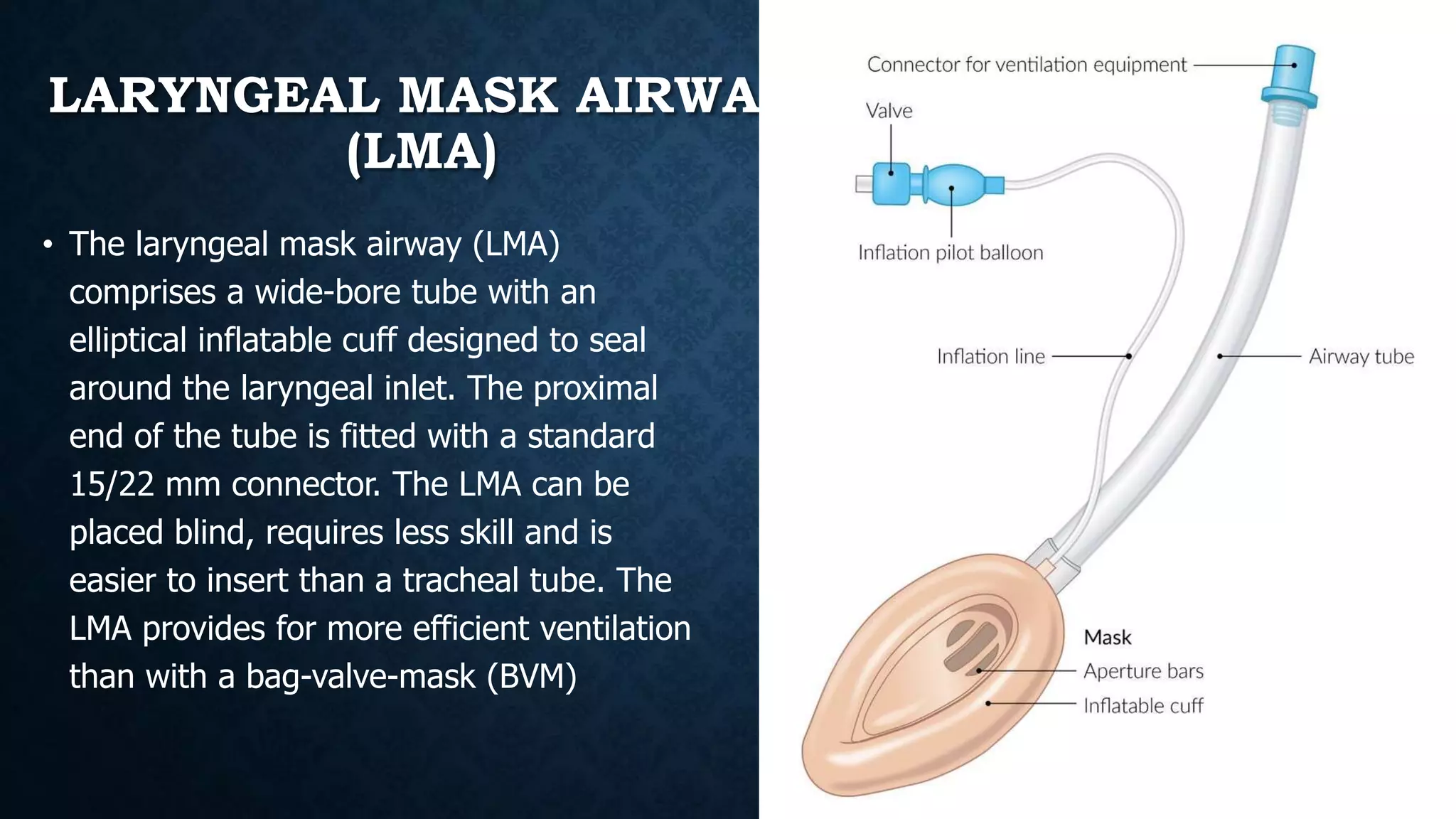
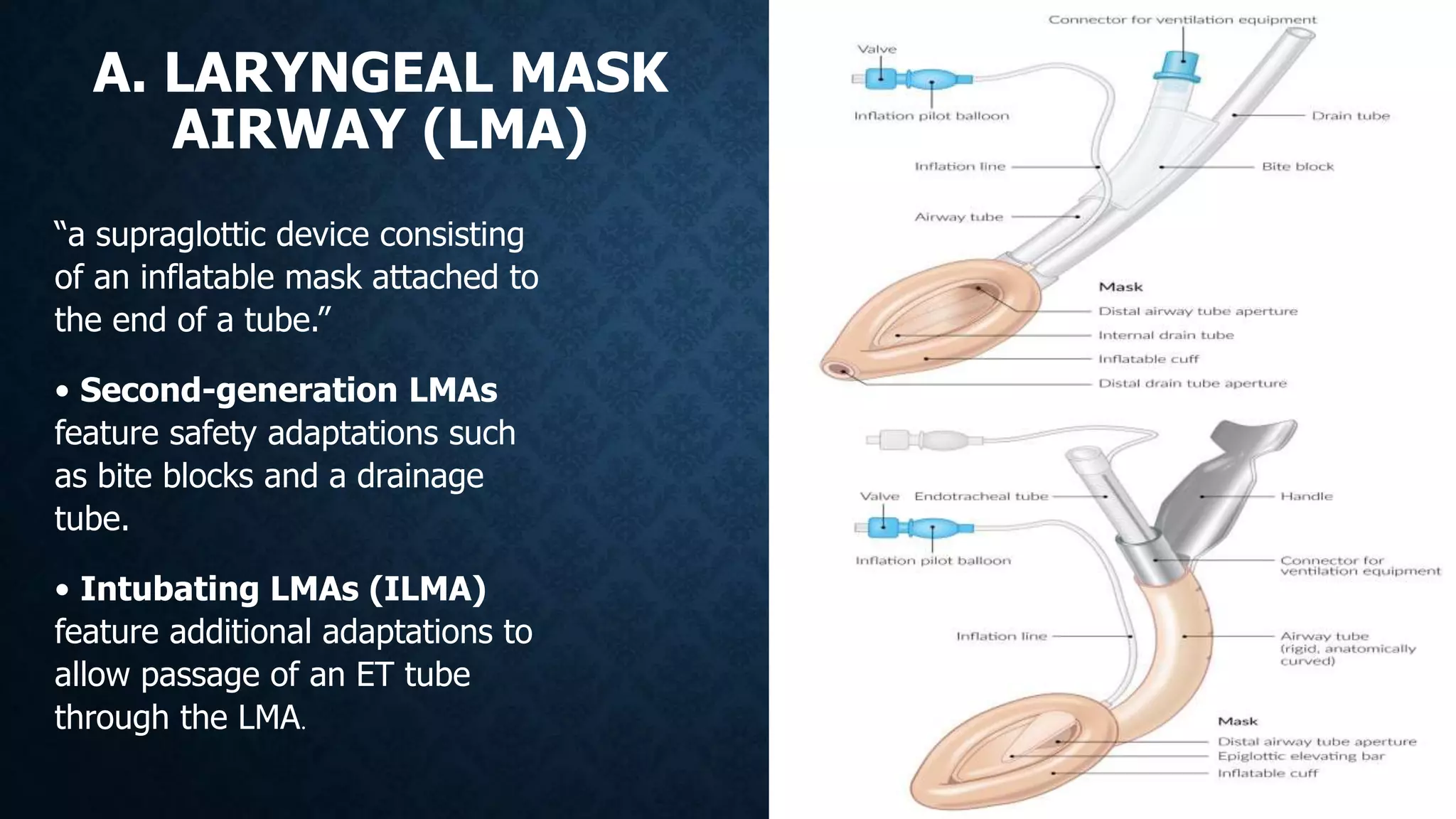
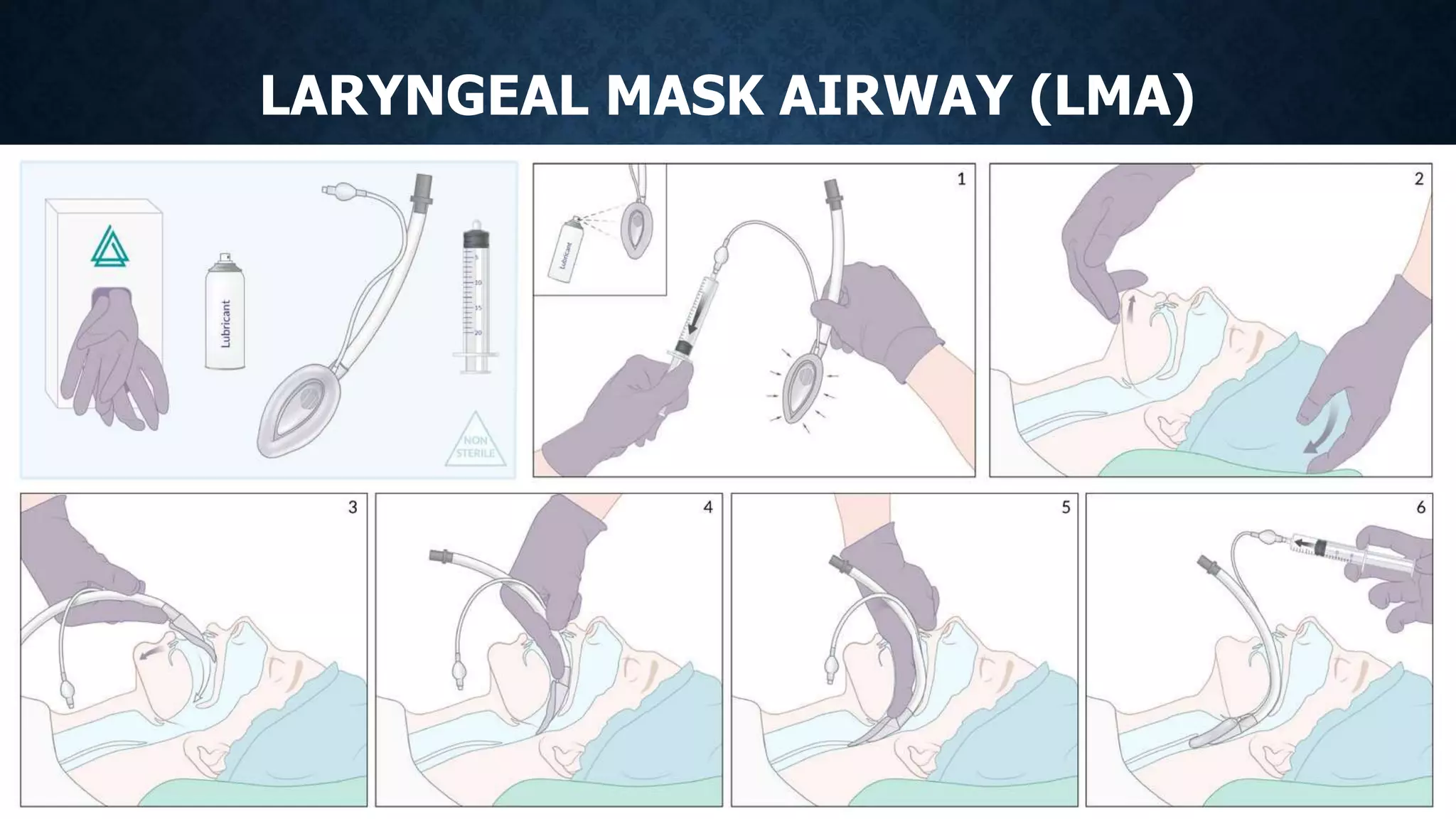
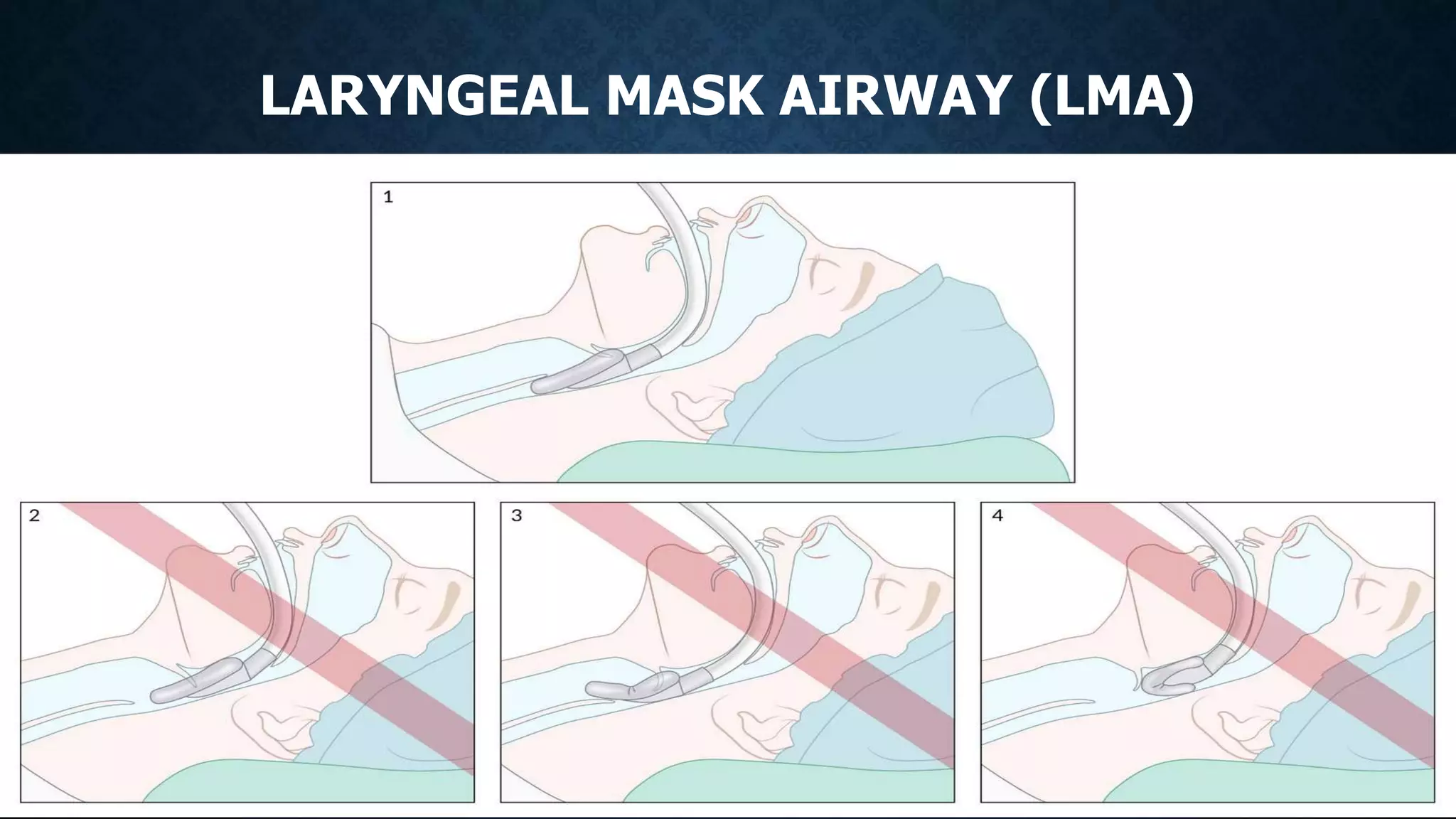
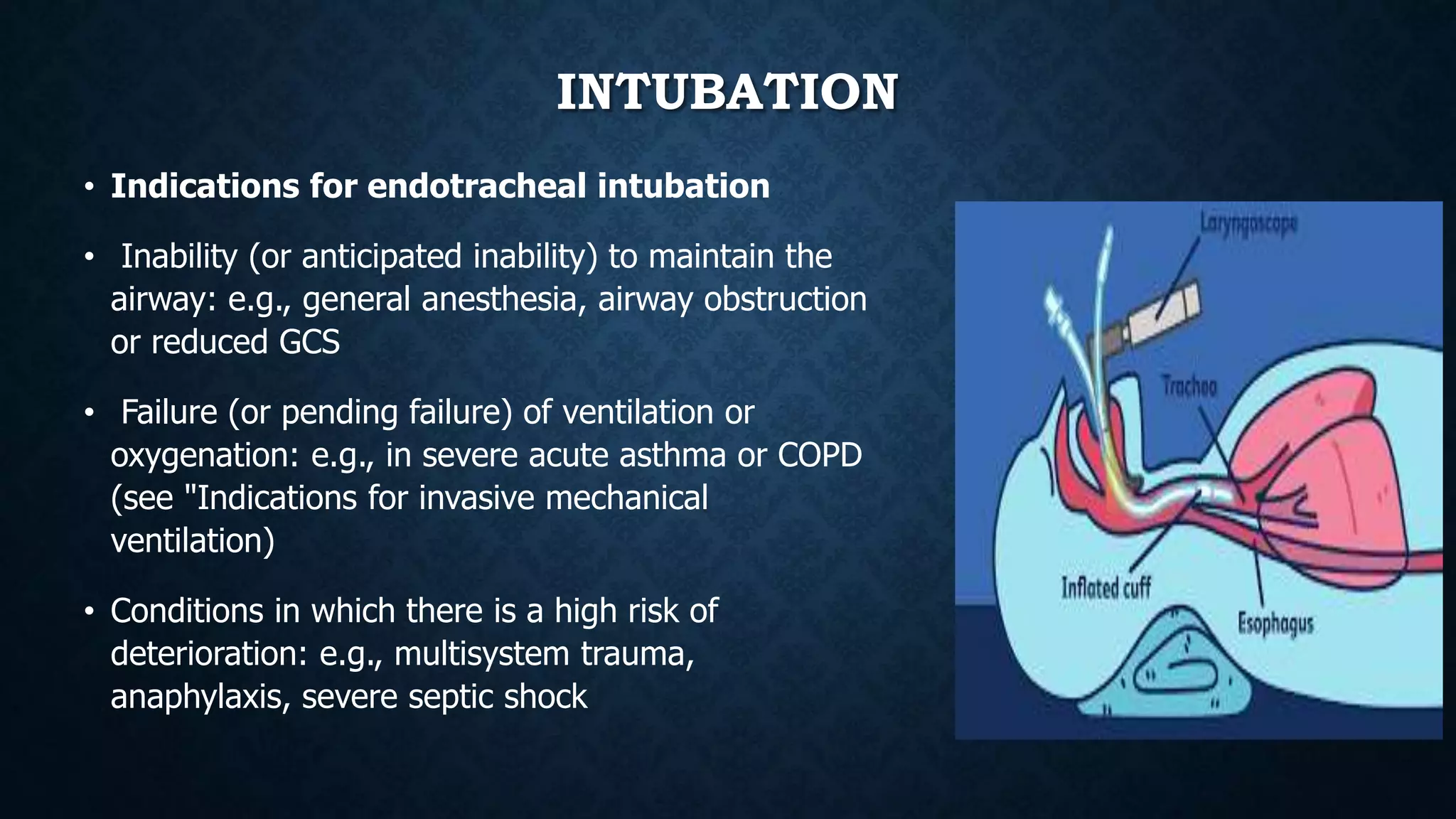
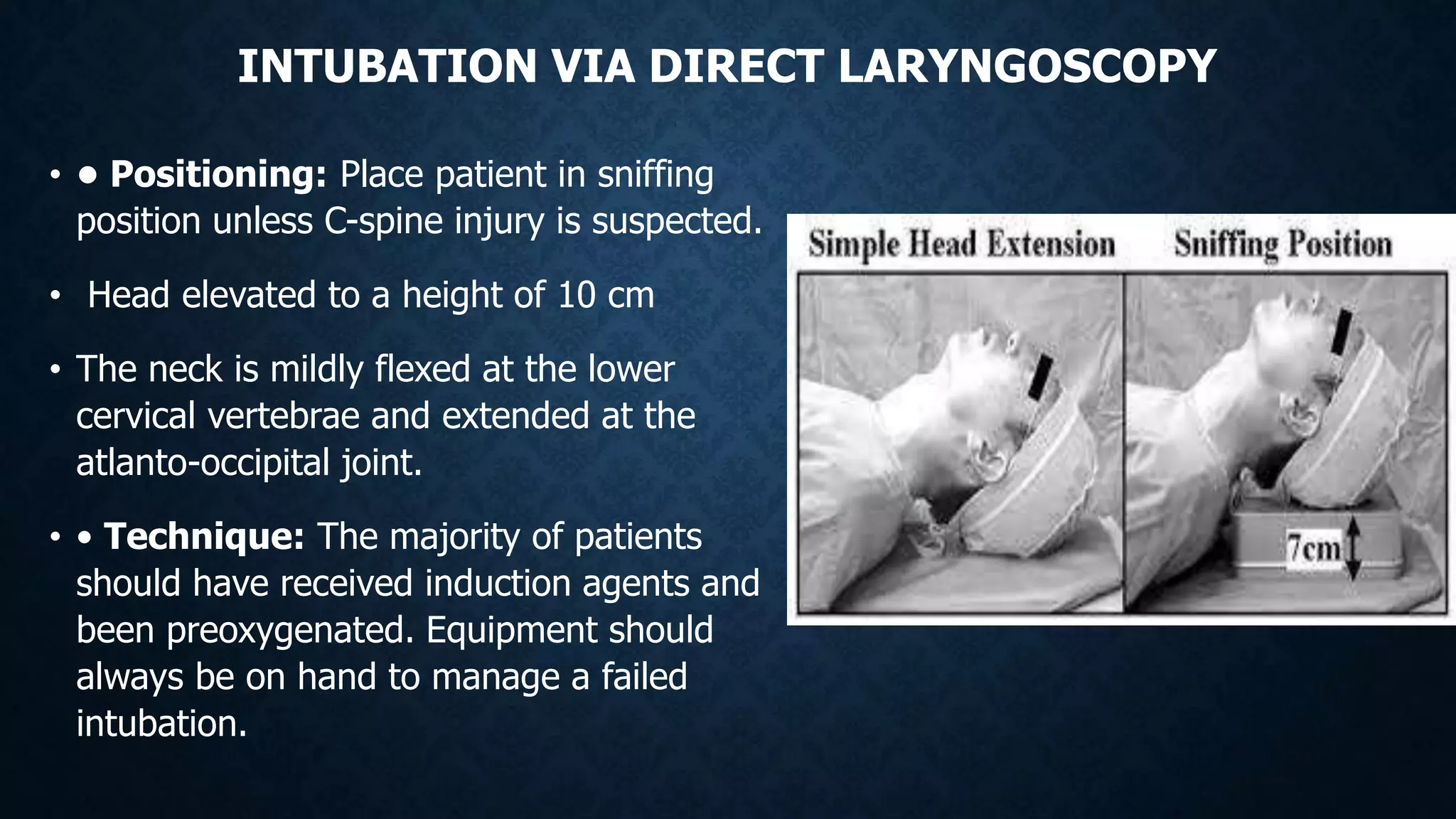
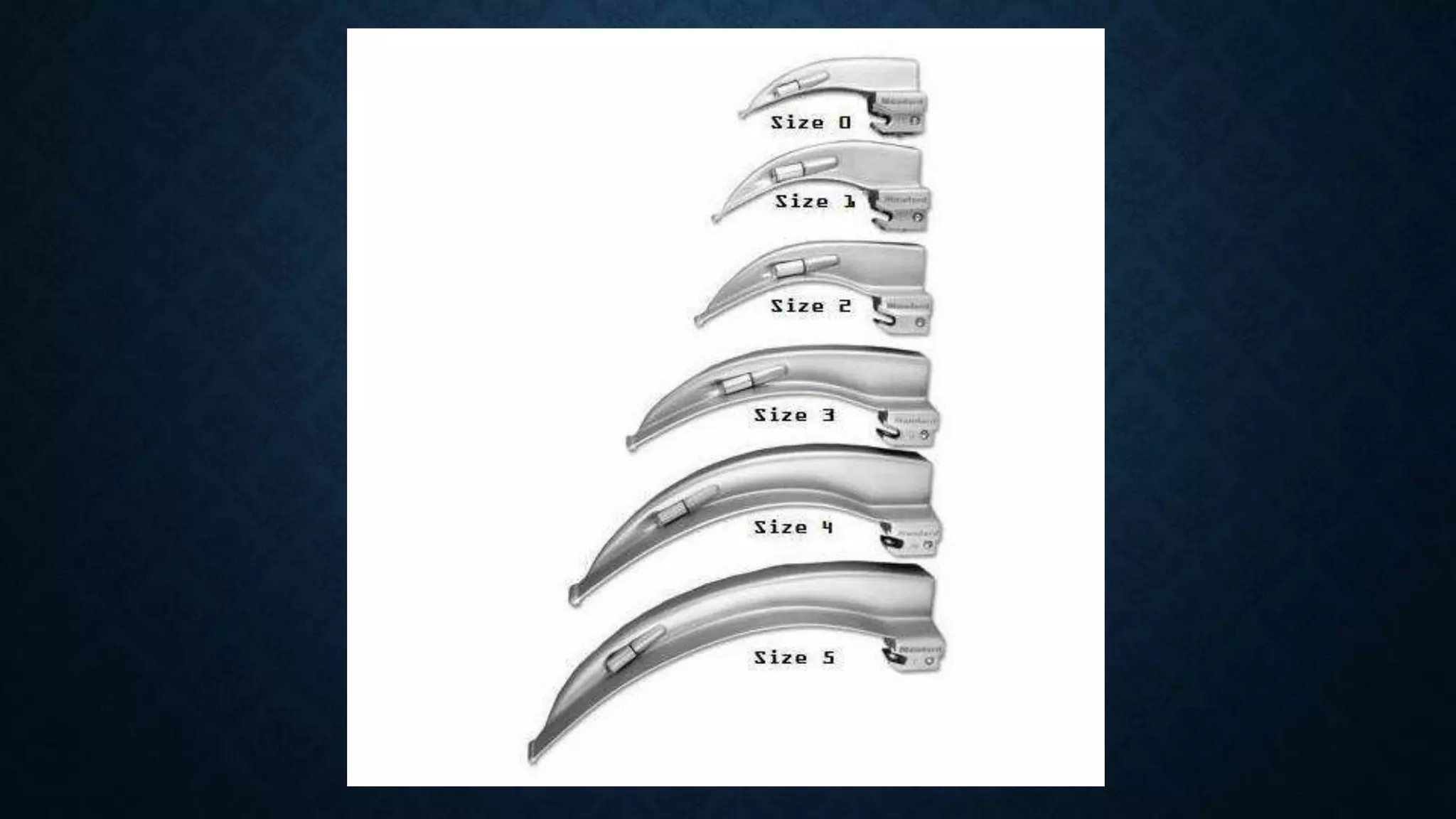
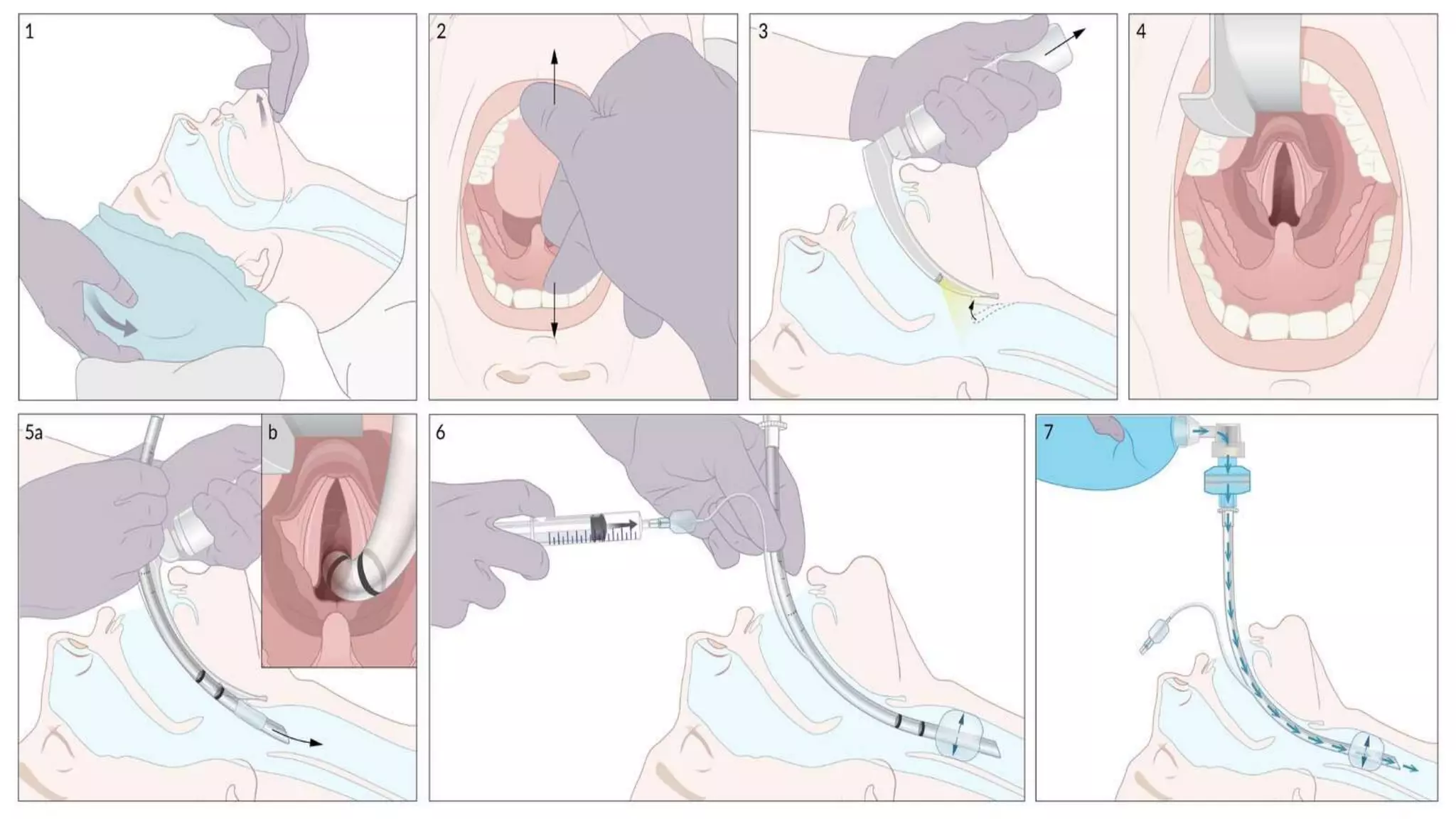
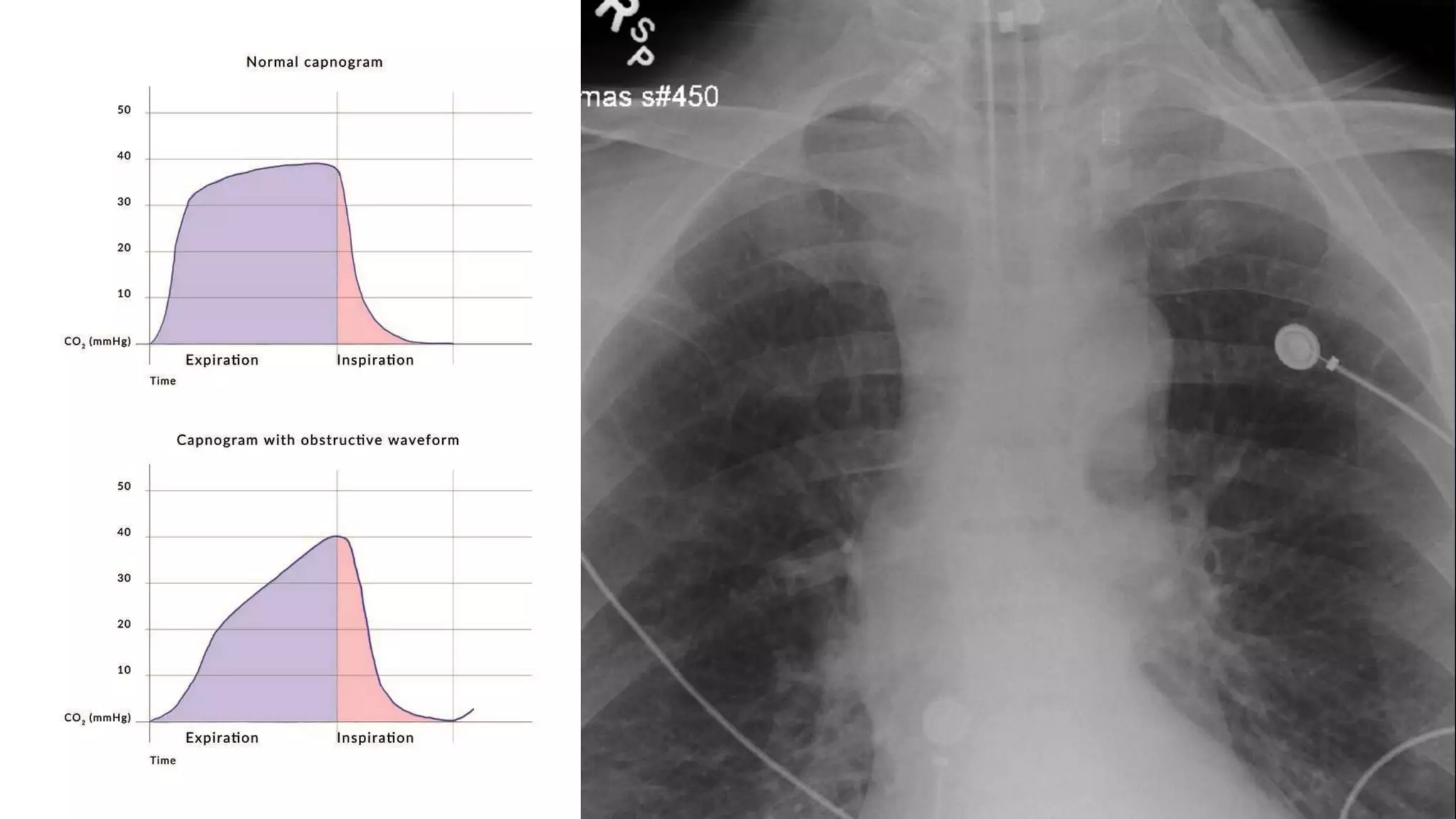
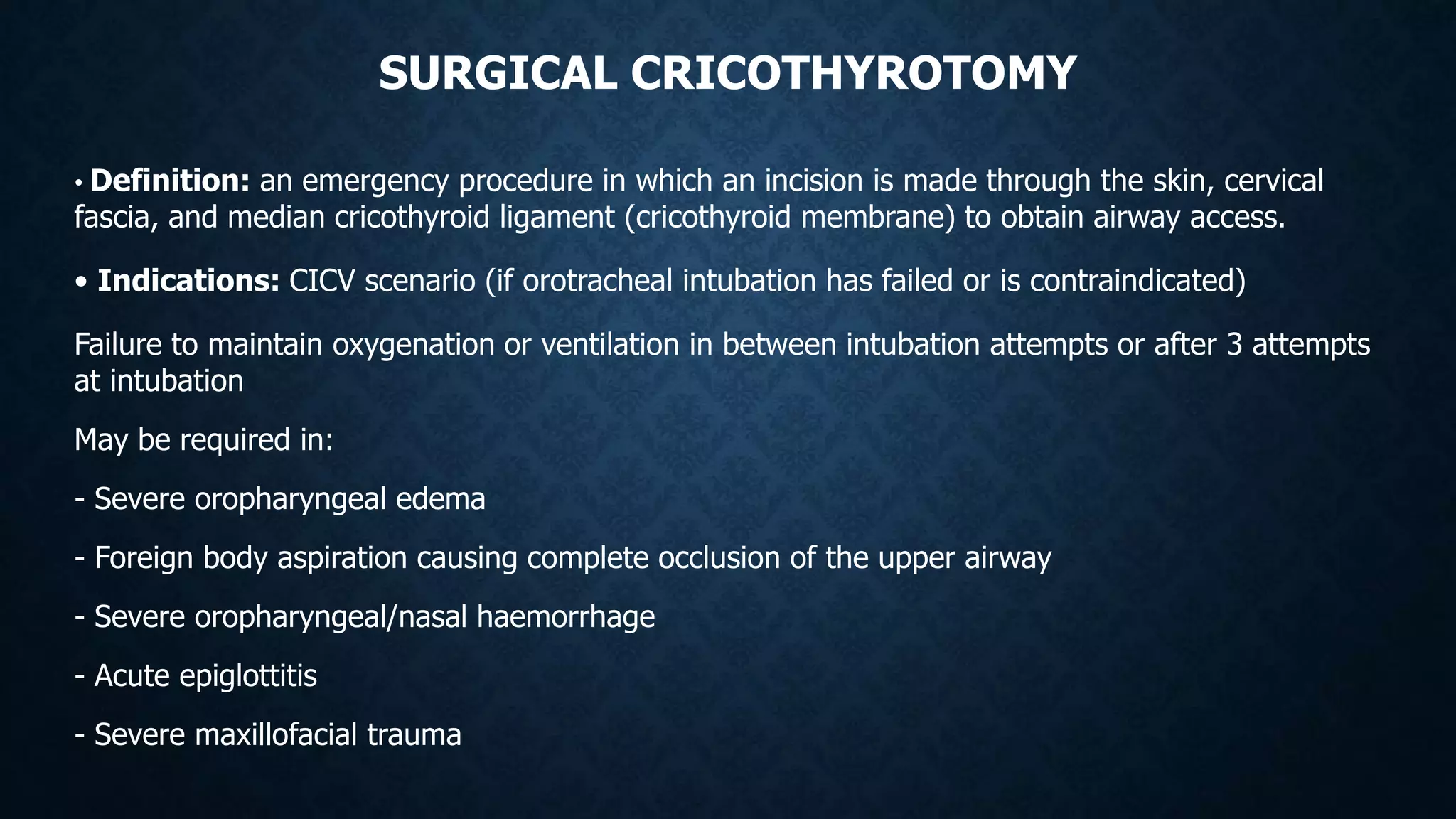
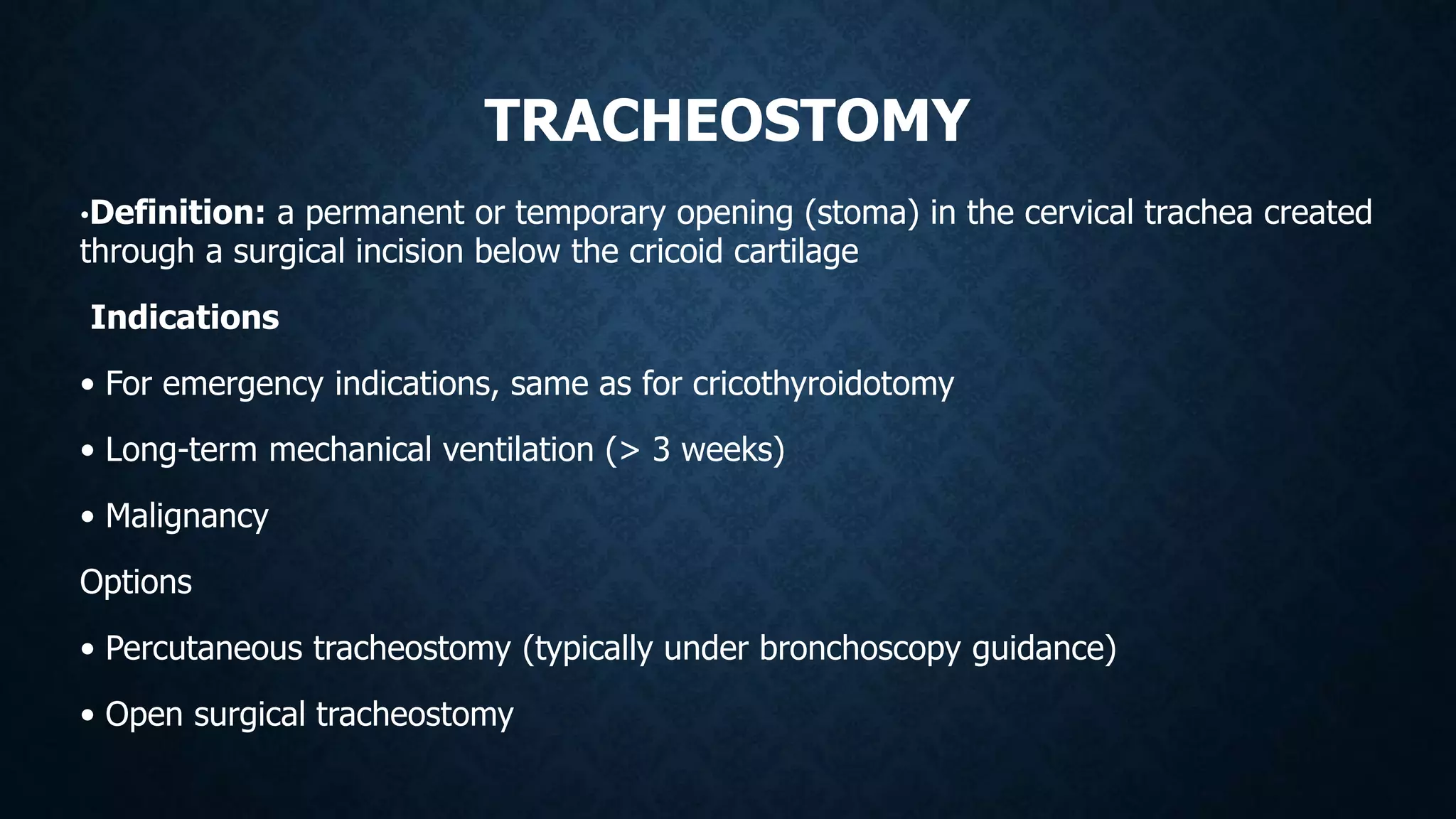
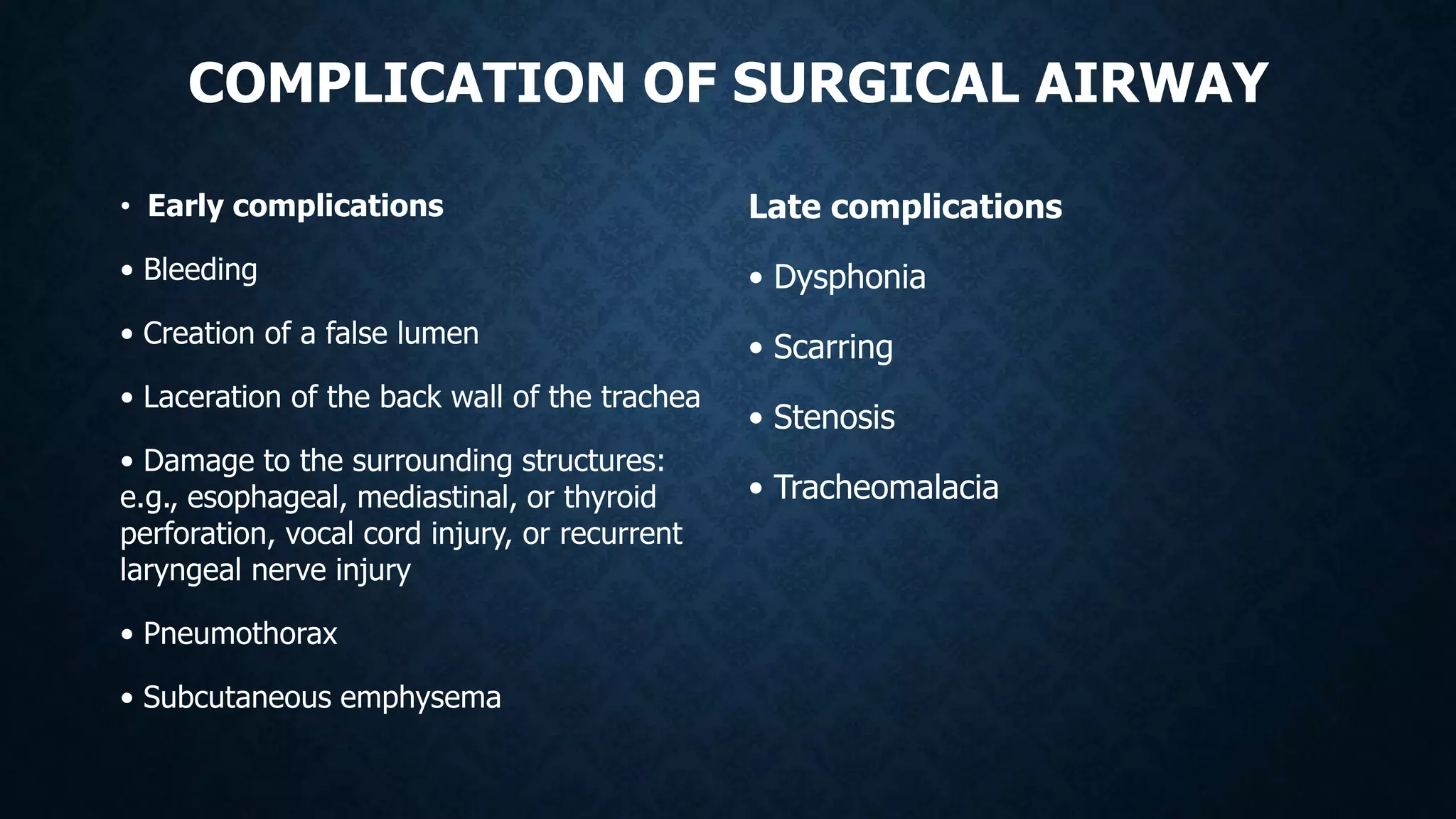
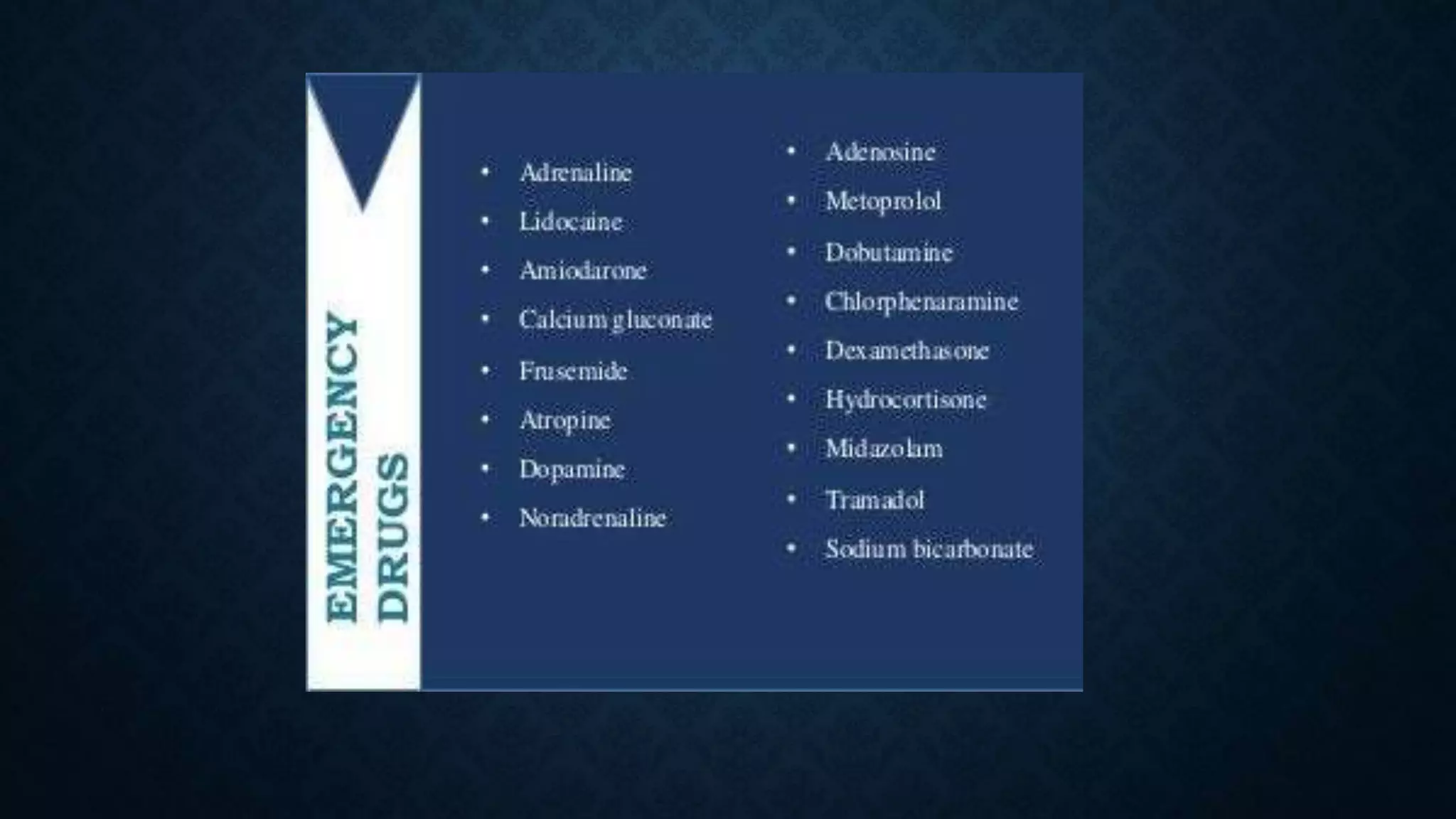
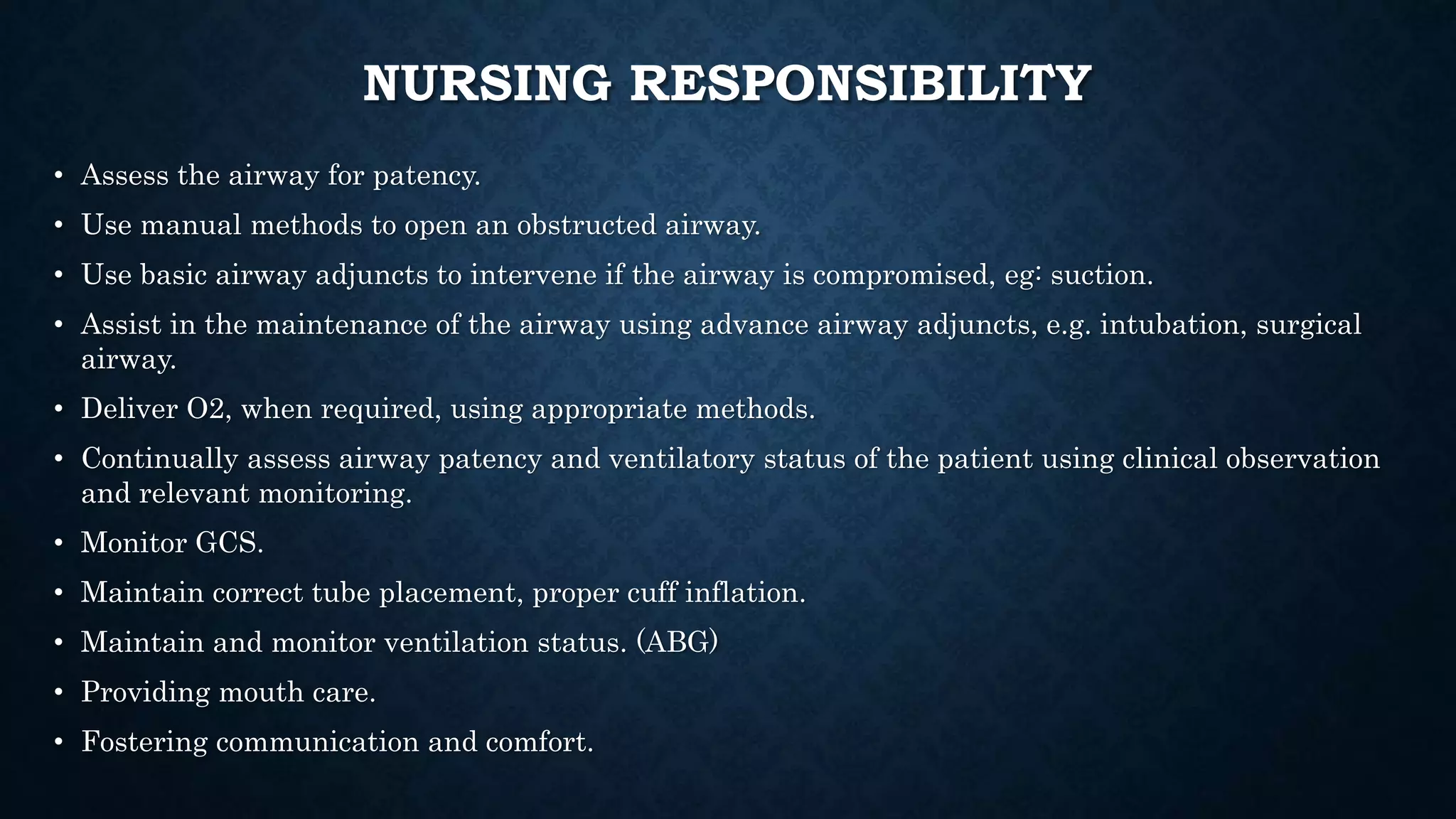
The document provides a comprehensive overview of airway management, emphasizing its critical role in maintaining effective ventilation and oxygenation in patients, particularly in emergency and critical care settings. It covers definitions, clinical features of airway obstruction, respiratory arrest, basic and advanced airway maneuvers, and various airway adjuncts, with a focus on their indications, procedures, and potential complications. The importance of proper assessment and management techniques, such as intubation and the use of devices like the laryngeal mask airway, is highlighted to ensure patient safety and effective treatment.