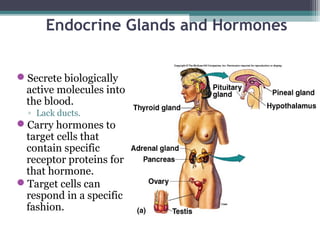
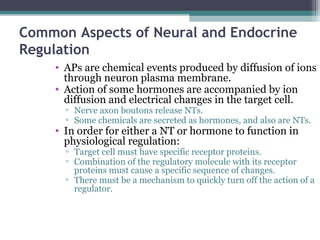
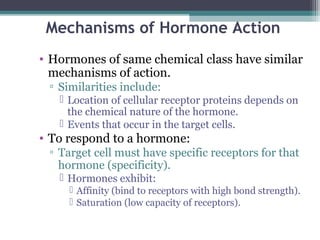
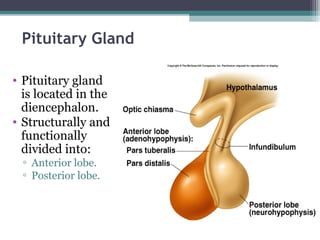
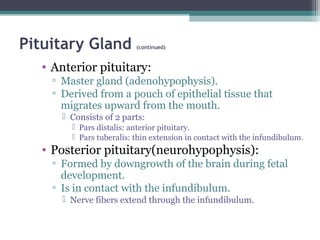
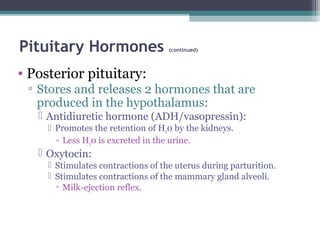
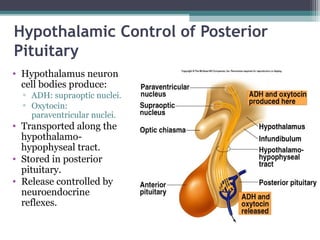
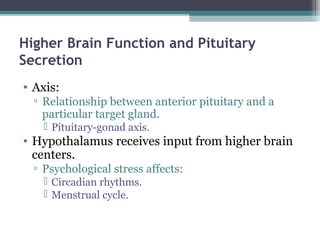
The document discusses endocrine glands and hormones. It explains that endocrine glands secrete hormones directly into the bloodstream, lacking ducts, and hormones are carried to target cells containing receptors. Hormones affect metabolism and regulate body processes like growth and reproduction. The mechanisms of hormone action depend on their chemical structure, with some binding to nuclear receptors to alter gene expression and others using second messengers to enact cellular responses. The pituitary gland is described as having anterior and posterior lobes that secrete trophic and regulatory hormones under control of the hypothalamus.
![Effects of [Hormone] on Tissue
Response
• [Hormone] in blood reflects the rate of
secretion.
• Half-life:
▫ Time required for the blood [hormone] to be reduced
to ½ reference level.
Minutes to days.
• Normal tissue responses are produced only
when [hormone] are present within
physiological range.
• Varying [hormone] within normal,
physiological range can affect the
responsiveness of target cells.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-12-320.jpg)
![Effects of [Hormone] on Tissue
Response (continued)
• Priming effect (upregulation):
▫ Increase number of receptors formed on target
cells in response to particular hormone.
▫ Greater response by the target cell.
• Desensitization (downregulation):
▫ Prolonged exposure to high [polypeptide
hormone].
Subsequent exposure to the same [hormone] produces less
response.
Decrease in number of receptors on target cells.
▫ Insulin in adipose cells.
▫ Pulsatile secretion may prevent downregulation.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-13-320.jpg)
![Pituitary Hormones
• Anterior
Pituitary:
▫ Trophic effects:
High blood
[hormone] causes
target organ to
hypertrophy.
Low blood
[hormone] causes
target organ to
atrophy.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-29-320.jpg)
![Actions of T3
• Stimulates protein synthesis.
• Promotes maturation of nervous system.
• Stimulates rate of cellular respiration by:
▫ Production of uncoupling proteins.
▫ Increase active transport by Na+
/K+
pumps.
▫ Lower cellular [ATP].
• Increases metabolic heat.
• Increases metabolic rate.
▫ Stimulates increased consumption of glucose, fatty
acids and other molecules.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-46-320.jpg)
![Diseases of the Thyroid (continued)
[Iodine-deficiency (endemic) goiter—continued]
▫ Adult myxedema:
Accumulation of mucoproteins and fluid in subcutaneous tissue.
▫ Symptoms:
Decreased metabolic rate.
Weight gain.
Decreased ability to adapt to cold.
Lethargy.
• Grave’s disease:
▫ Autoimmune disorder:
Exerts TSH-like effects on thyroid.
Not affected by negative feedback.
• Cretinism:
▫ Hypothyroid from end of 1st
trimester to 6 months postnatally.
Severe mental retardation.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-48-320.jpg)
![Parathyroid Glands
• Embedded in the lateral
lobes of the thyroid gland.
• Parathyroid hormone
(PTH):
▫ Only hormone secreted by
the parathyroid glands.
• Single most important
hormone in the control of
blood [Ca2+
].
• Stimulated by decreased
blood [Ca2+
].
• Promotes rise in blood [Ca2+
]
by acting on bones, kidney
and intestines.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-49-320.jpg)
![Pancreatic Islets (Islets of
Langerhans)
• Alpha cells secrete glucagon.
▫ Stimulus is decrease in blood
[glucose].
▫ Stimulates glycogenolysis
and lipolysis.
▫ Stimulates conversion of
fatty acids to ketones.
• Beta cells secrete insulin.
▫ Stimulus is increase in blood
[glucose].
▫ Promotes entry of glucose
into cells.
▫ Converts glucose to glycogen
and fat.
▫ Aids entry of amino acids
into cells.](https://image.slidesharecdn.com/chp11endocrineglands-151007044205-lva1-app6892/85/Endocrine-glands-50-320.jpg)