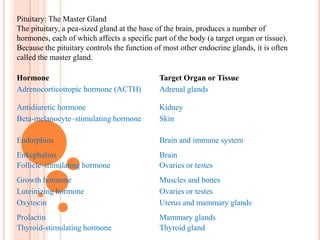
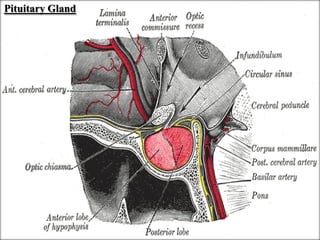
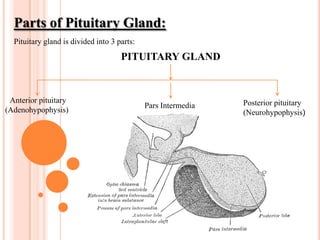
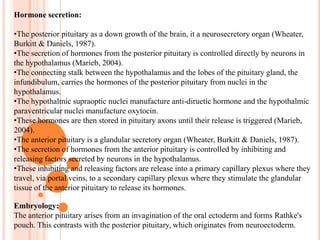
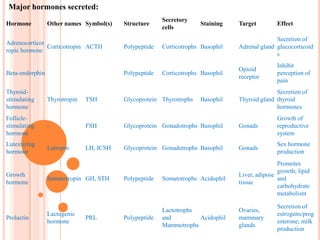
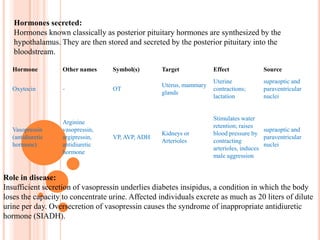
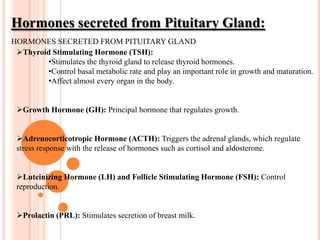
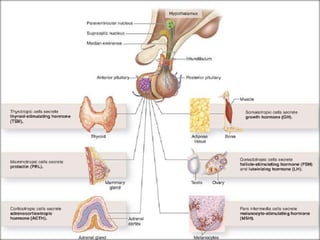
The pituitary gland is a small gland located at the base of the brain that regulates several important bodily functions. It is divided into anterior and posterior lobes. The anterior lobe secretes hormones that control other endocrine glands and regulate processes like growth, metabolism, and reproduction. These include growth hormone, thyroid stimulating hormone, and adrenocorticotropic hormone. The posterior lobe stores and releases oxytocin and vasopressin, which are produced in the hypothalamus and help regulate water balance and milk release. Disorders of the pituitary can impact hormone levels and cause wide-ranging symptoms.




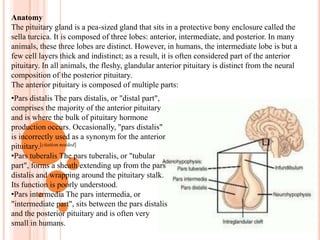
![Proper function of the anterior pituitary and of the organs it regulates can often be ascertained via blood tests that measure hormone levels.AnatomyThe pituitary gland is a pea-sized gland that sits in a protective bony enclosure called the sella turcica. It is composed of three lobes: anterior, intermediate, and posterior. In many animals, these three lobes are distinct. However, in humans, the intermediate lobe is but a few cell layers thick and indistinct; as a result, it is often considered part of the anterior pituitary. In all animals, the fleshy, glandular anterior pituitary is distinct from the neural composition of the posterior pituitary.The anterior pituitary is composed of multiple parts:Pars distalis The pars distalis, or "distal part", comprises the majority of the anterior pituitary and is where the bulk of pituitary hormone production occurs. Occasionally, "pars distalis" is incorrectly used as a synonym for the anterior pituitary.[citation needed]](https://image.slidesharecdn.com/presentation1-101204233519-phpapp02/85/Pituitary-Gland-28-320.jpg)




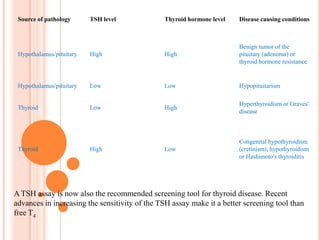
![The TSH receptorThe TSH receptor is found mainly on thyroid follicular cells.Stimulation of the receptor increases T3 and T4 production and secretion.Stimulating antibodies to this receptor mimic TSH and cause Graves' disease.Diagnostic:Further information: Reference ranges for blood tests.Thyroid hormonesTSH levels are tested in the blood of patients suspected of suffering from excess (hyperthyroidism), or deficiency (hypothyroidism) of thyroid hormone. In general, a standard reference range for TSH for adults is between 0.4 and 5.0 µIU/mL (equivalent to mIU/L), but values vary slightly among labs. The therapeutic target range TSH level for patients on treatment ranges between 0.3 to 3.0 μIU/L.The interpretation depends also on what the blood levels of thyroid hormones (T3 and T4) are.TSH levels for children normally start out much higher. In 2002, the National Academy of Clinical Biochemistry (NACB) in the United States recommended age-related reference limits starting from about 1.3 to 19 µIU/mL for normal-term infants at birth, dropping to 0.6–10 µIU/mL at 10 weeks old, 0.4–7.0 µIU/mL at 14 months and gradually dropping during childhood and puberty to adult levels, 0.4–4.0 µIU/mL.The NACB also stated that it expected the normal (95%) range for adults to be reduced to 0.4–2.5 µIU/mL, because research had shown that adults with an initially measured TSH level of over 2.0 µIU/mL had "an increased odds ratio of developing hypothyroidism over the [following] 20 years, especially if thyroid antibodies were elevated"](https://image.slidesharecdn.com/presentation1-101204233519-phpapp02/85/Pituitary-Gland-60-320.jpg)