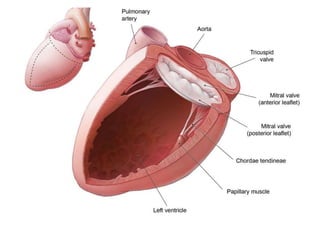
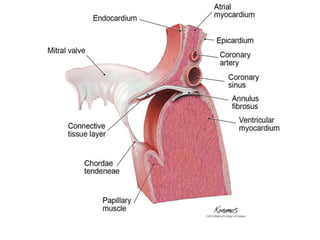
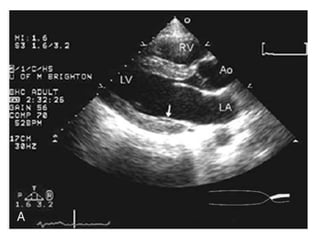
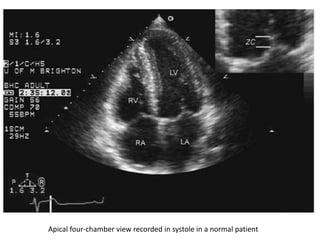
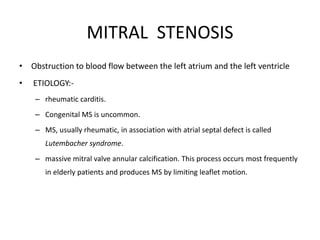
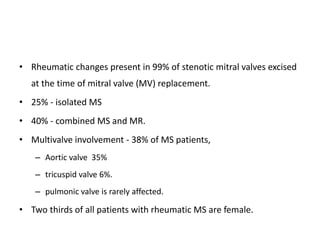
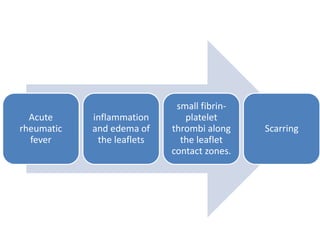
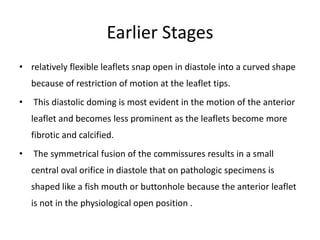
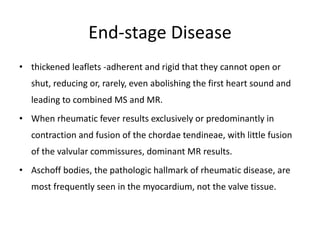
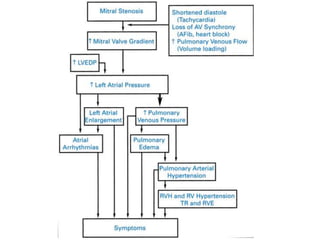
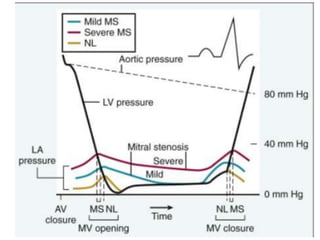
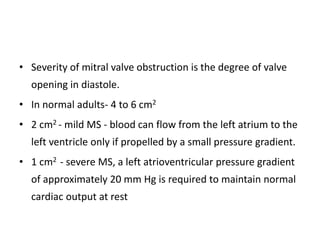
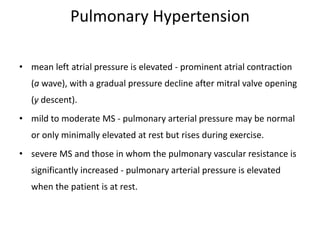
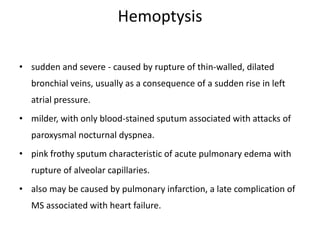
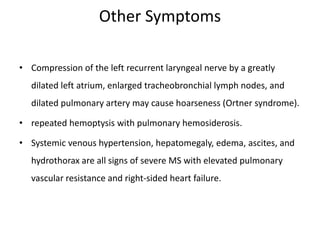
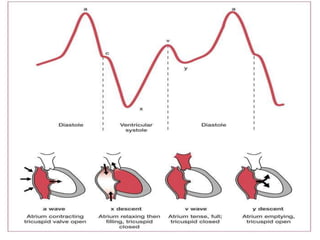
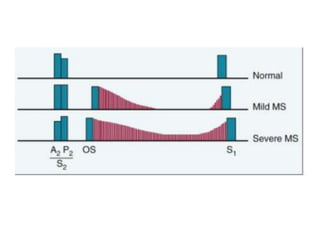
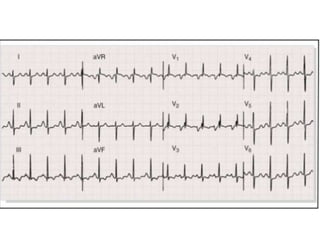
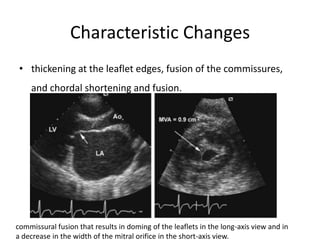
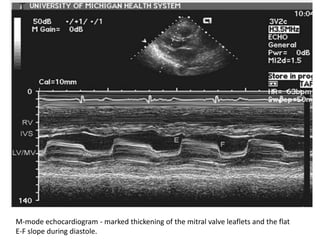
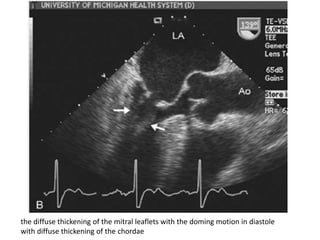
The mitral valve lies between the left atrium and left ventricle. Mitral stenosis is usually caused by rheumatic fever which causes scarring of the mitral valve leaflets and commissures. In early mitral stenosis, the leaflets can open but have restricted motion. Over time, the leaflets become thickened and rigid, reducing valve opening. This causes symptoms like dyspnea and pulmonary hypertension. On examination, findings may include an irregular pulse from atrial fibrillation, elevated jugular venous pressure, accentuated S1, and a diastolic murmur. Severe mitral stenosis can lead to right heart failure and complications like hemoptysis.