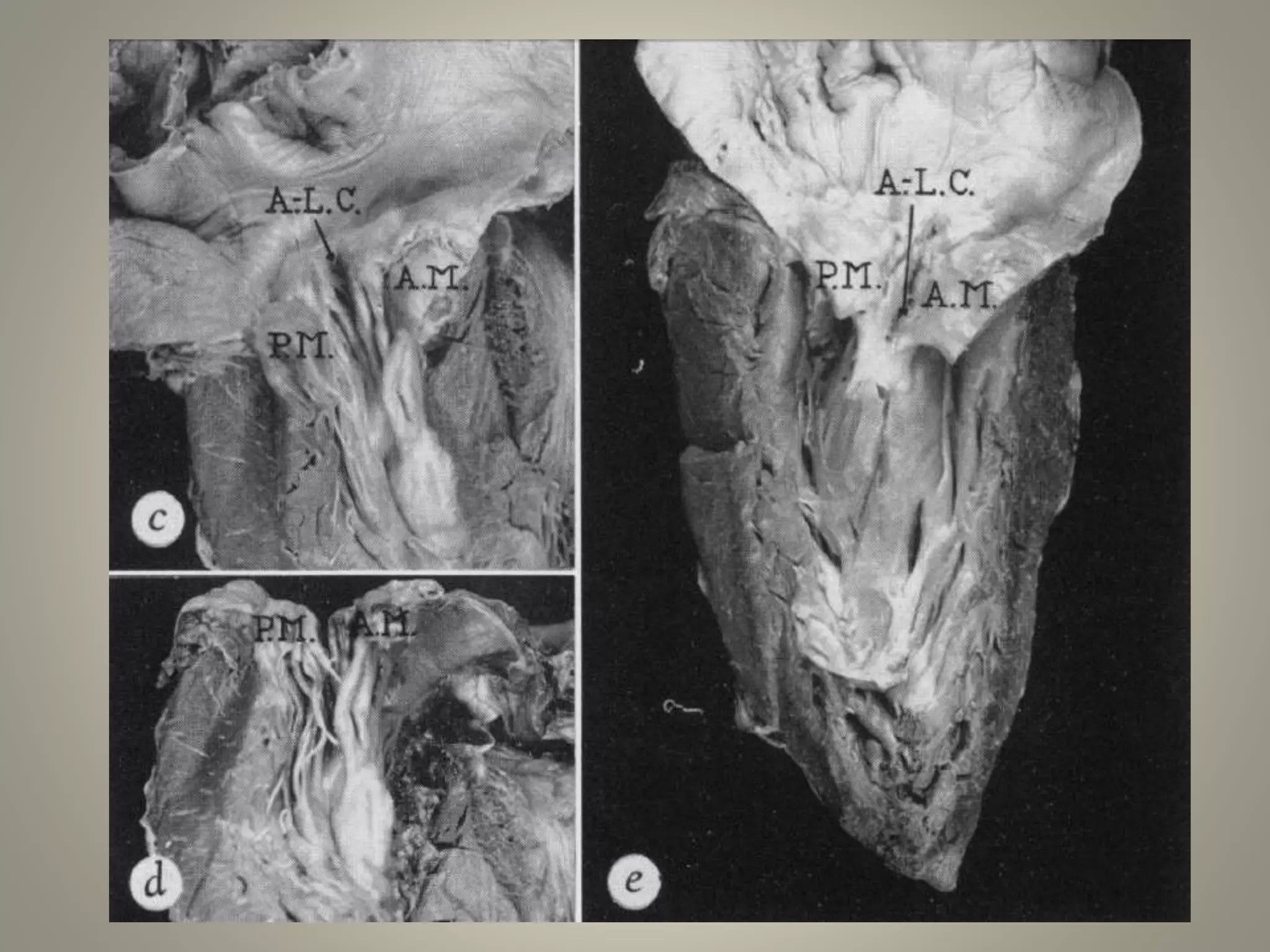
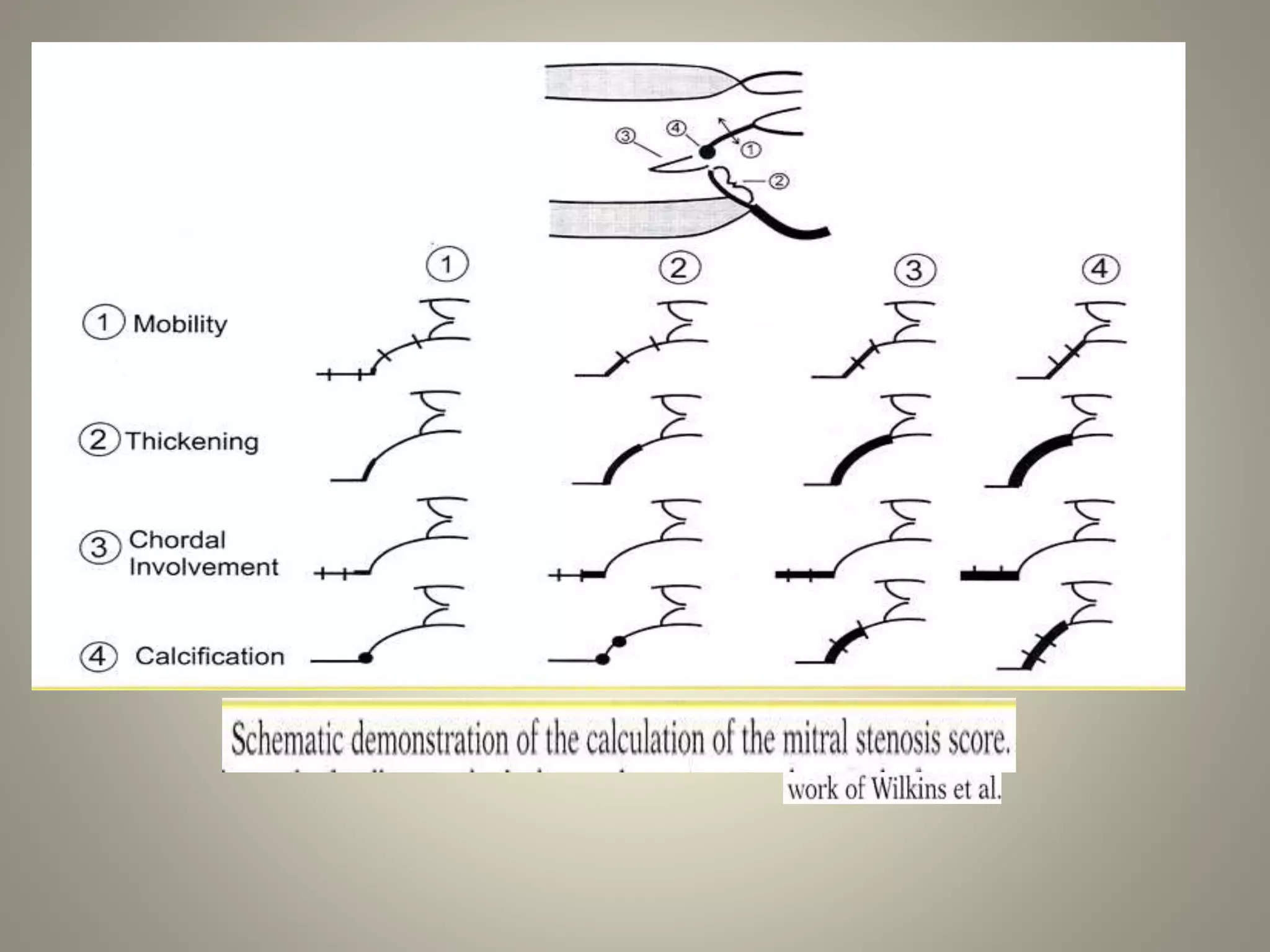
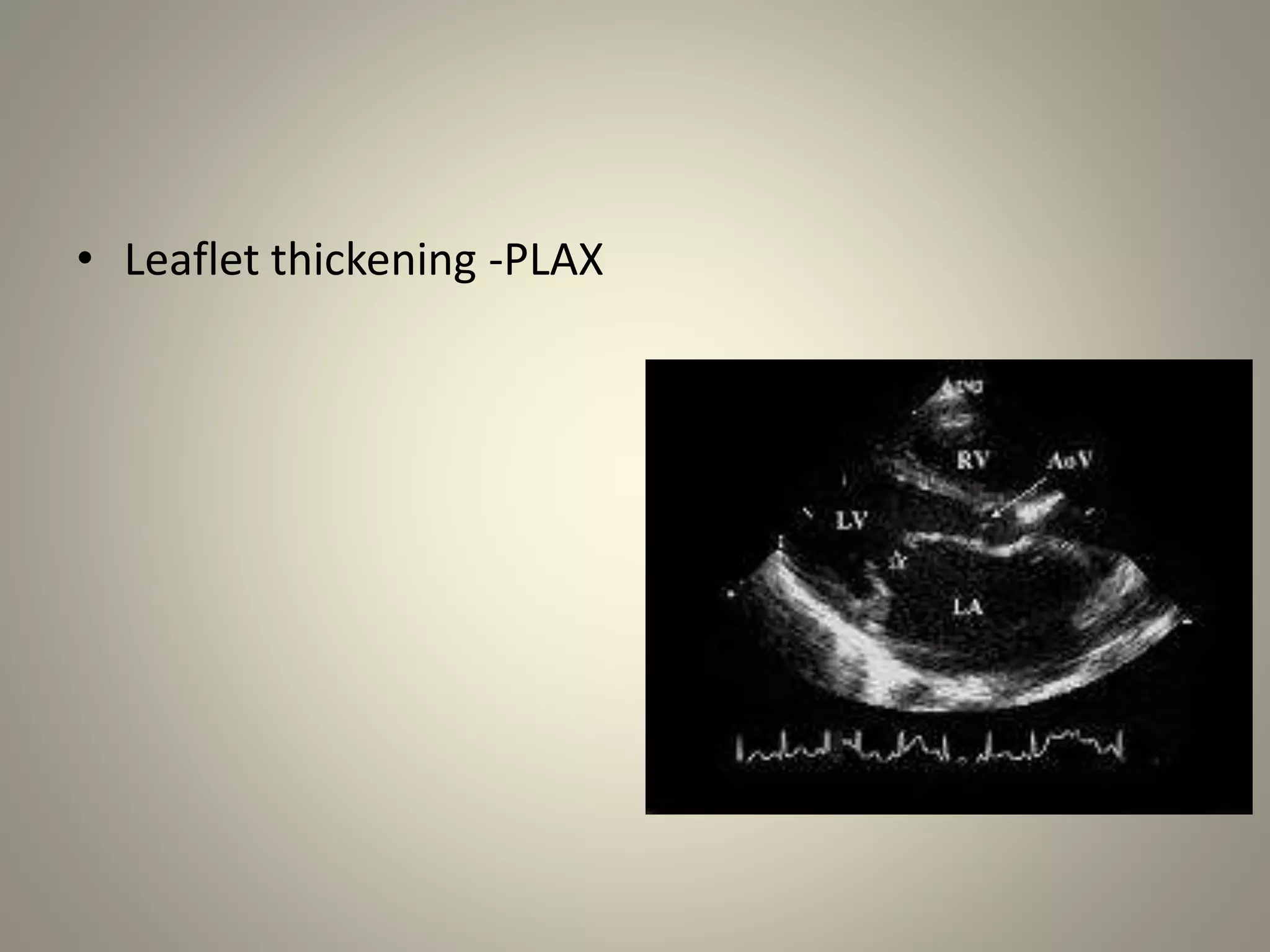
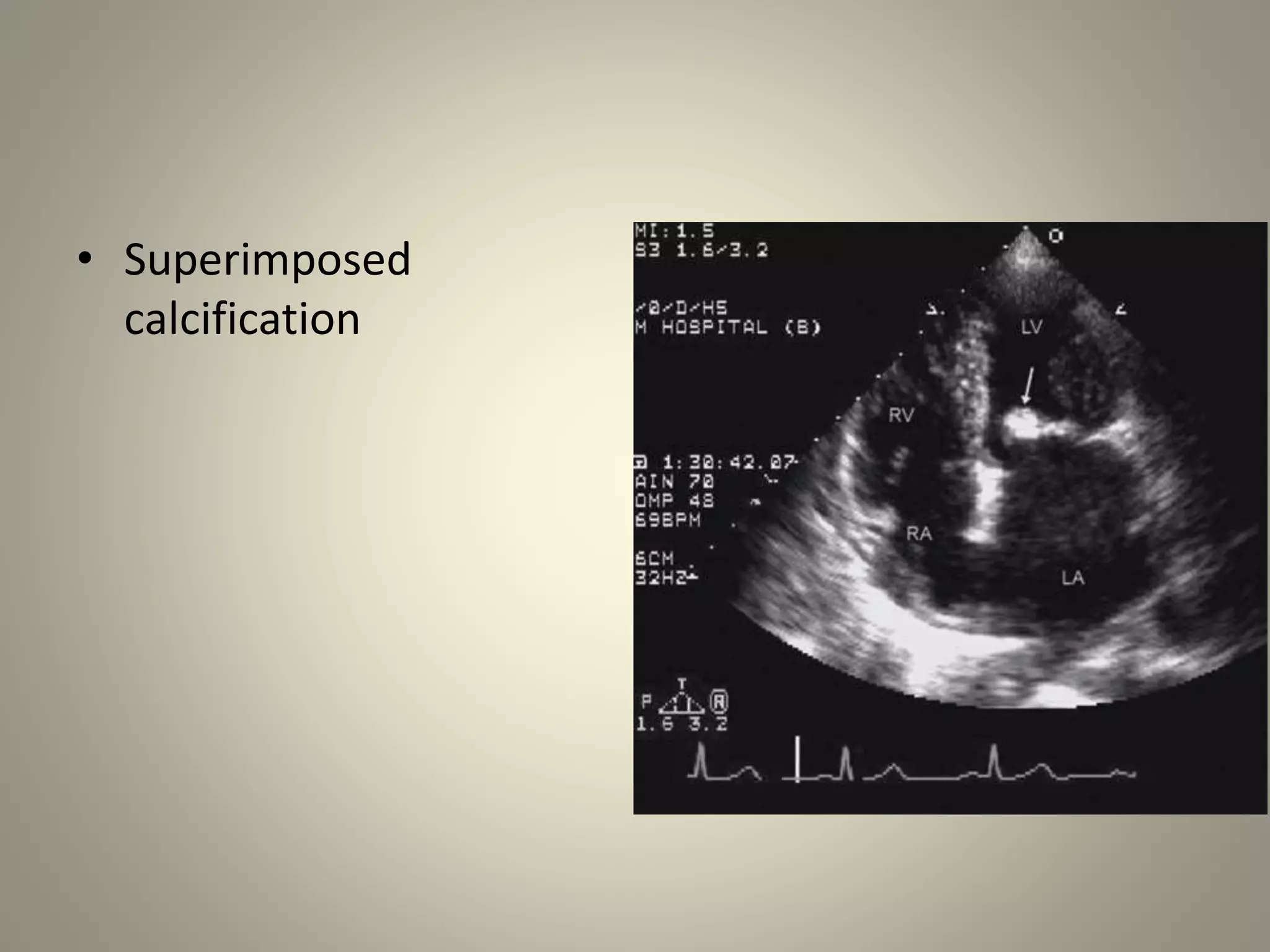
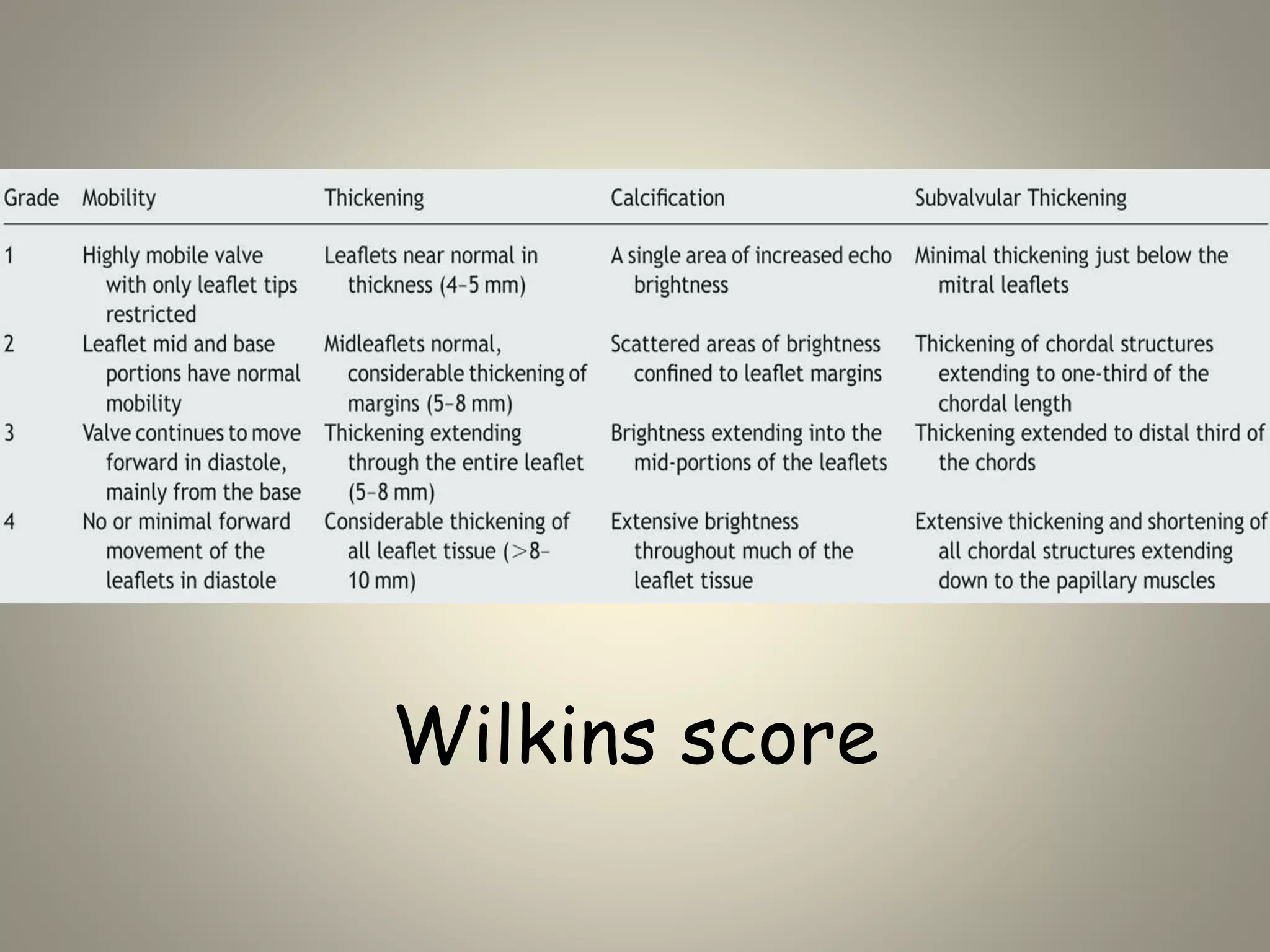
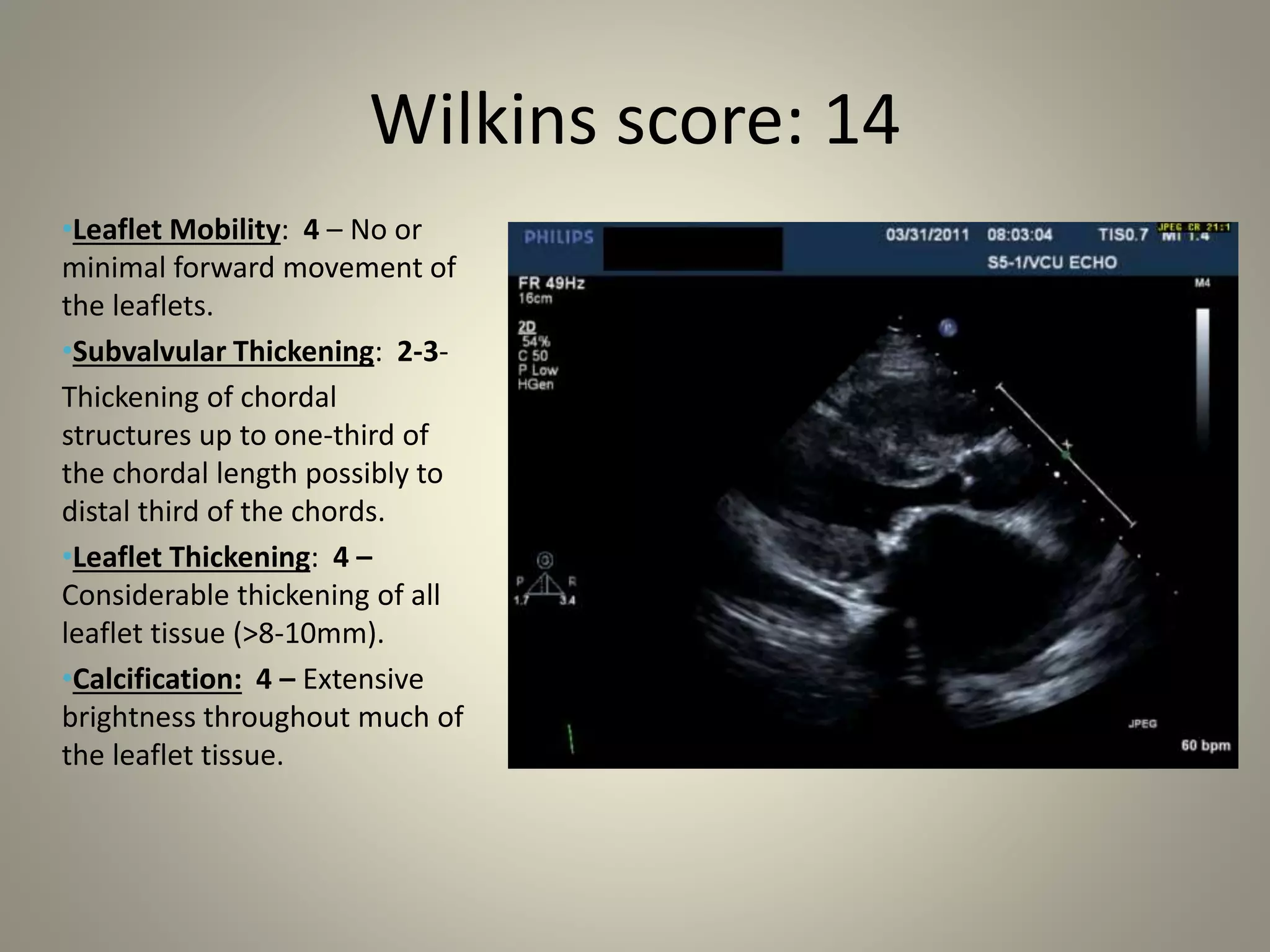
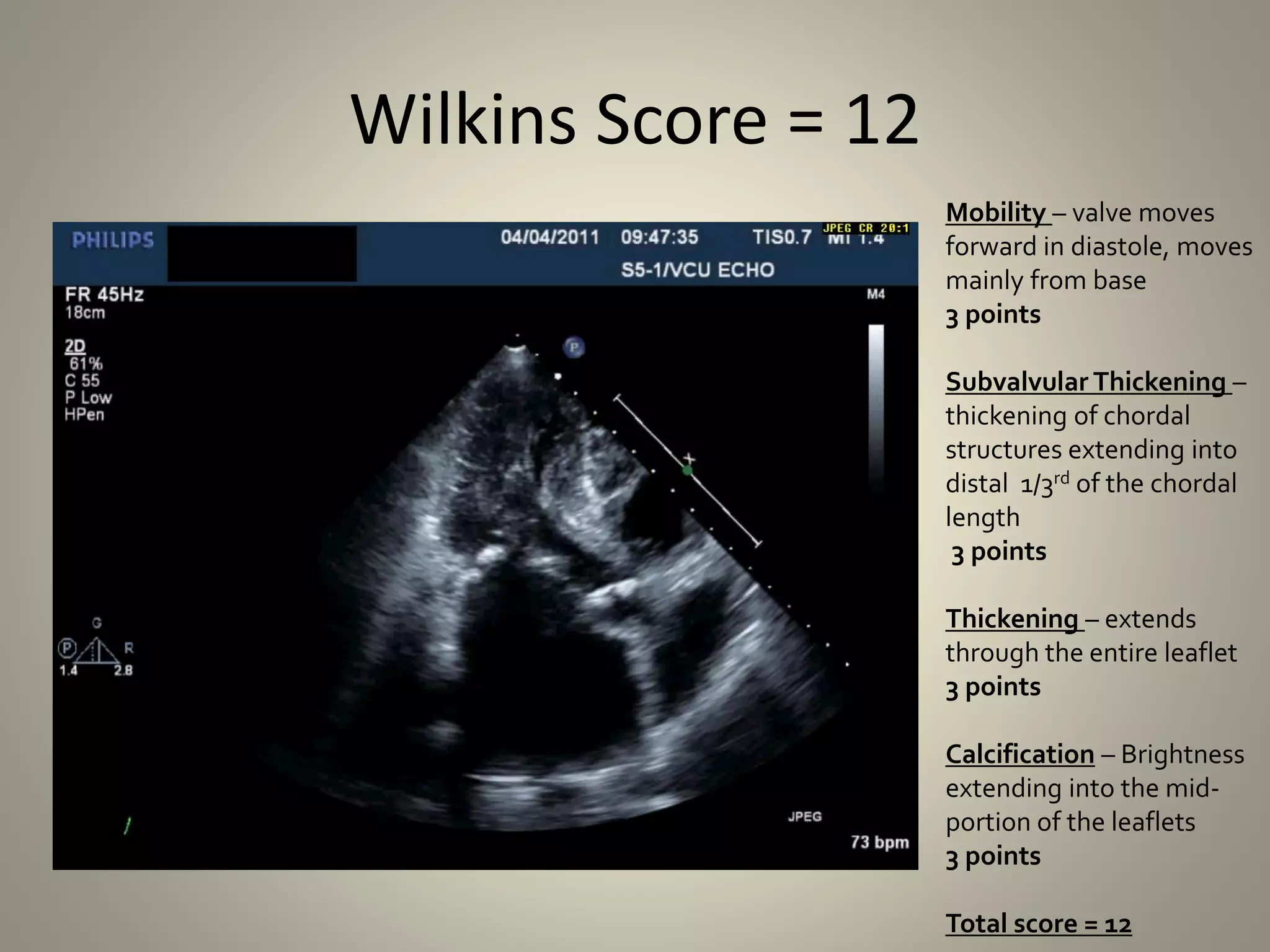
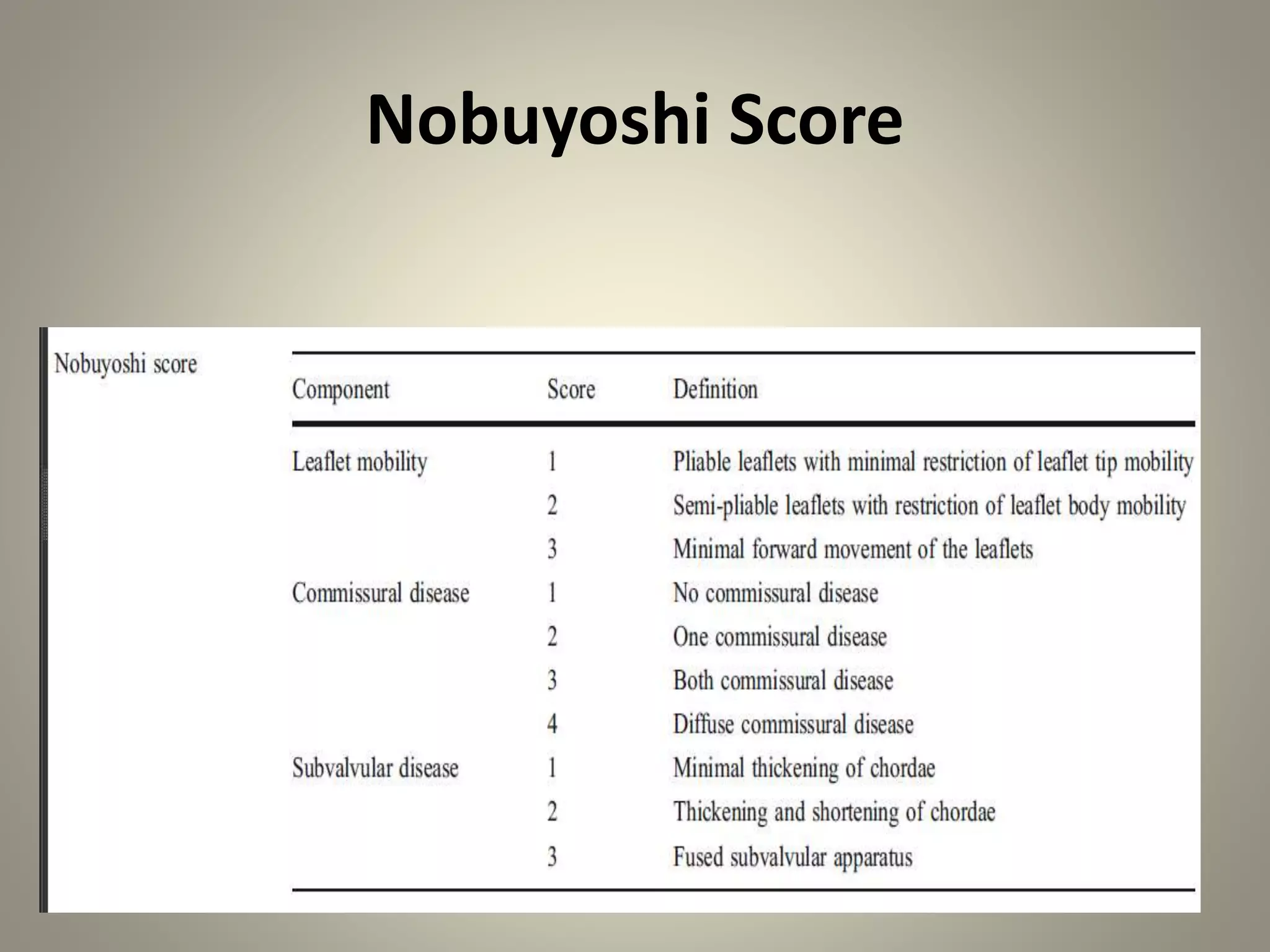
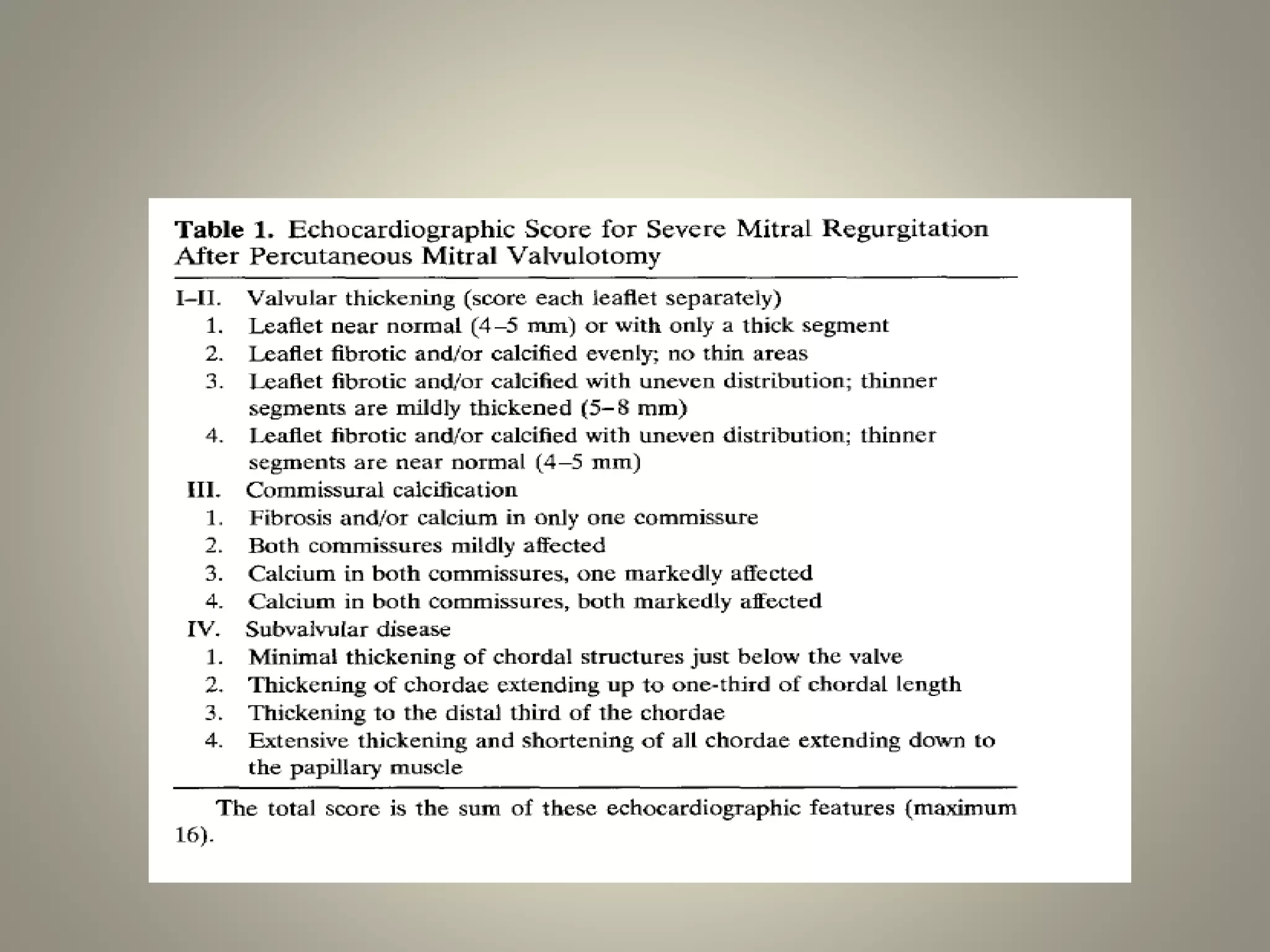
This document discusses various echocardiographic scoring systems used to assess mitral valve anatomy and predict outcomes of percutaneous balloon mitral valvuloplasty (PBMV). The Wilkins score and Commissural Calcification score are described in detail. The Wilkins score grades leaflet thickening, mobility, calcification and subvalvular involvement on a scale of 4-16. A score ≤8 indicates favorable anatomy for PBMV. The Commissural Calcification score quantifies calcification at each commissure. Other discussed scores include the Cormier score, RT-3DE score, Chen score, Reid score and Nobuyoshi score. Limitations of the scoring systems and ideas for an ideal future scoring