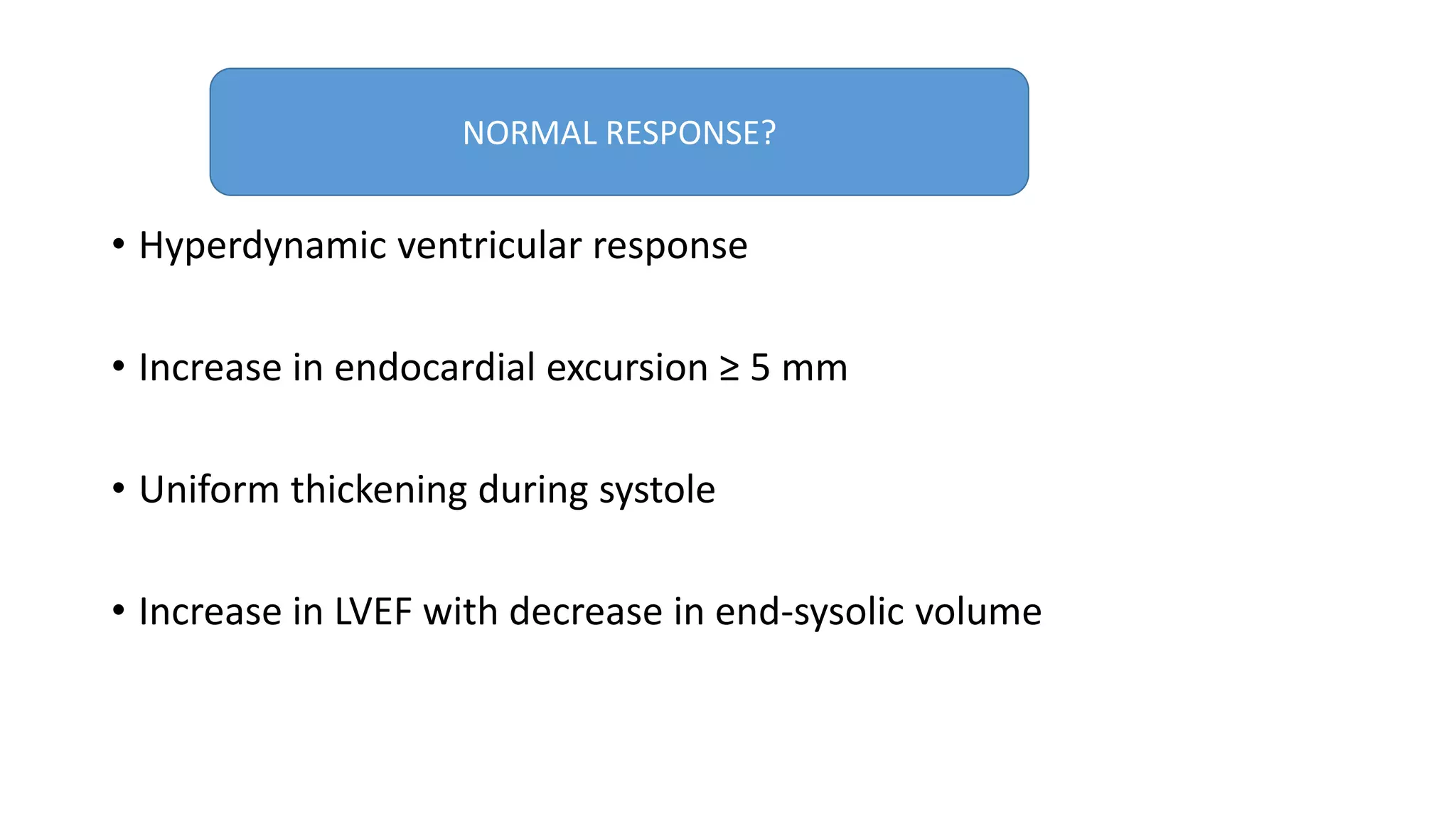
This document summarizes dobutamine stress echocardiography (DSE). Key points include:
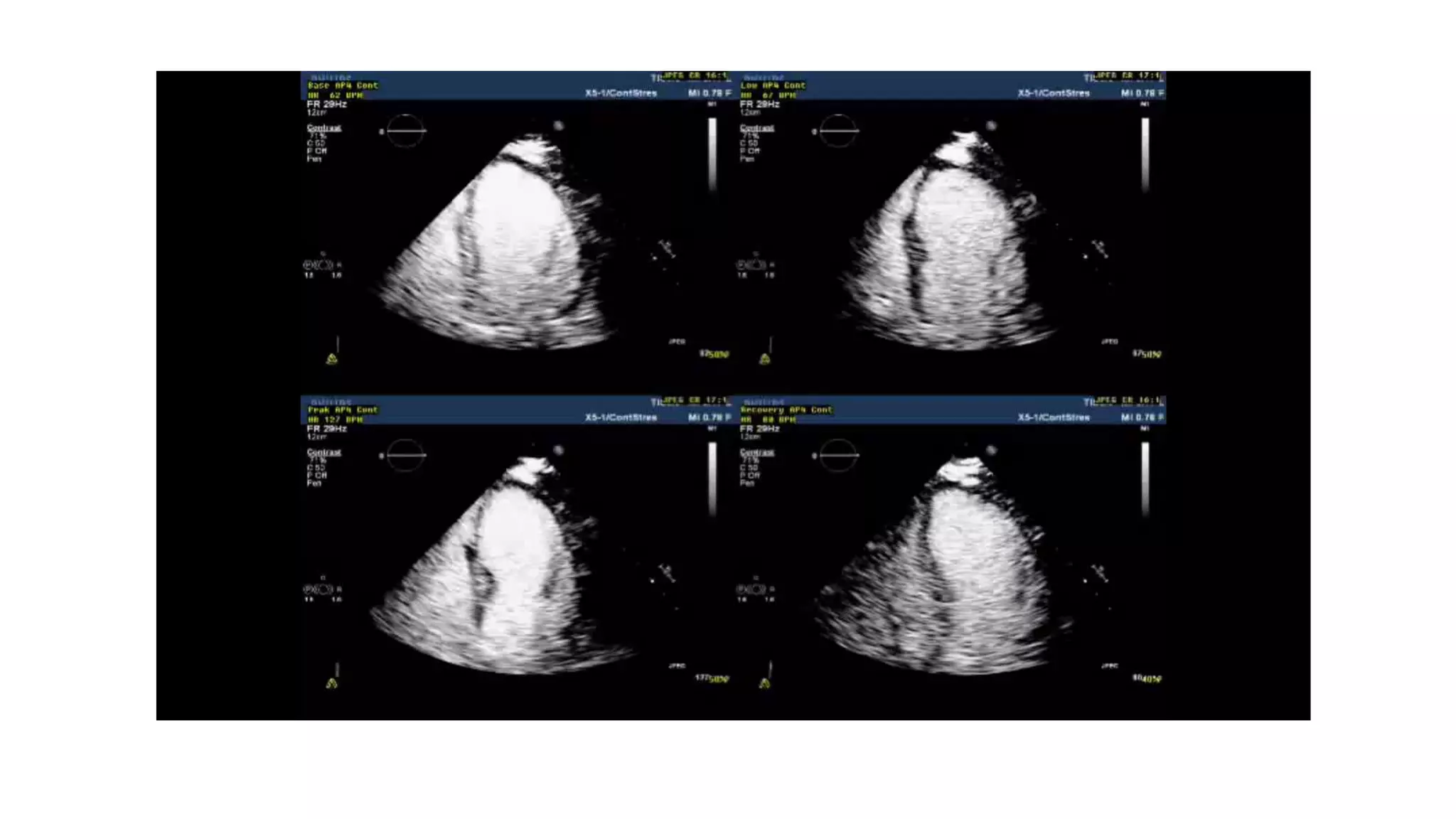
- DSE uses the drug dobutamine to simulate exercise and increase heart rate, contractility, and myocardial oxygen demand to detect ischemia.
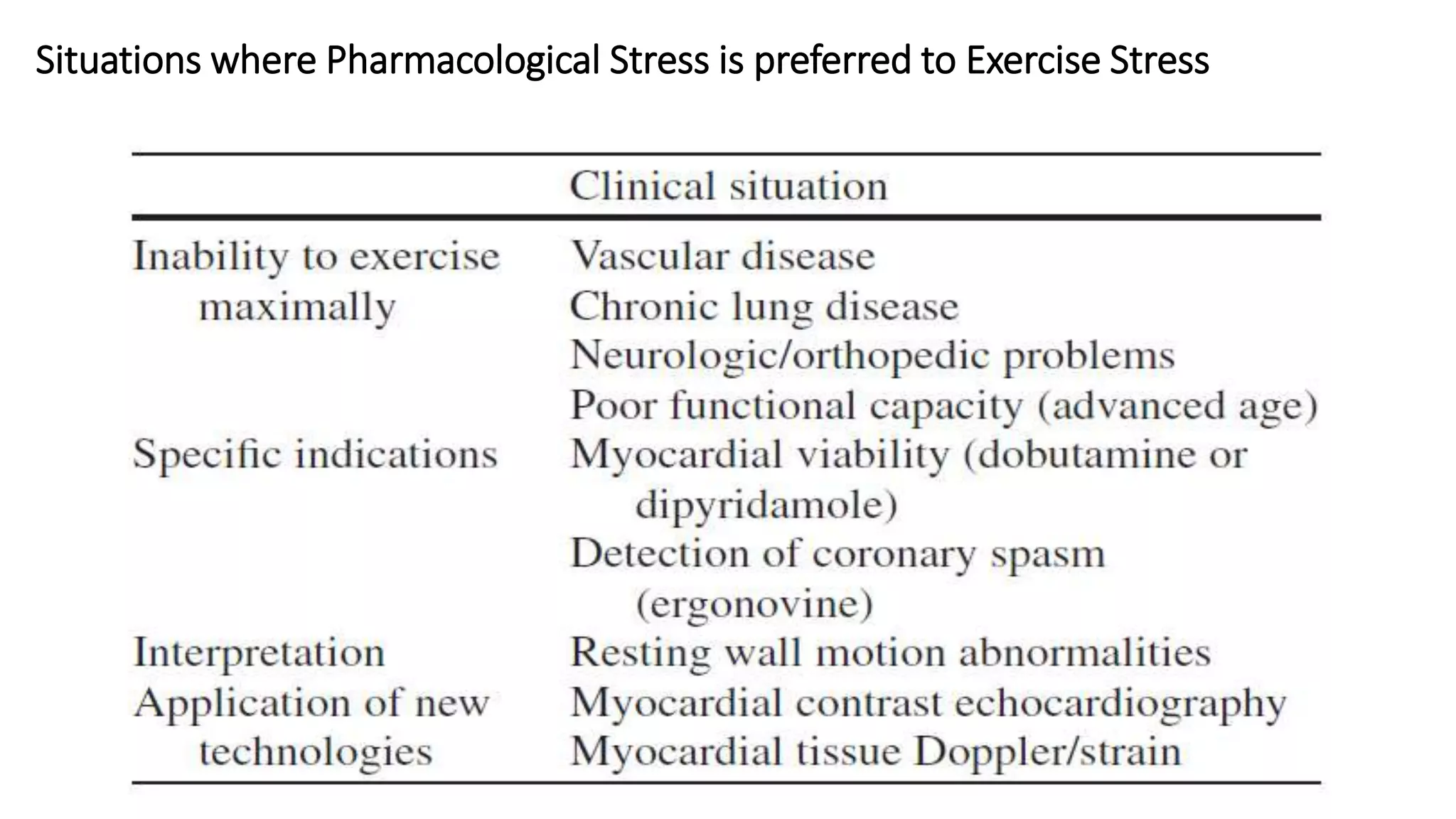
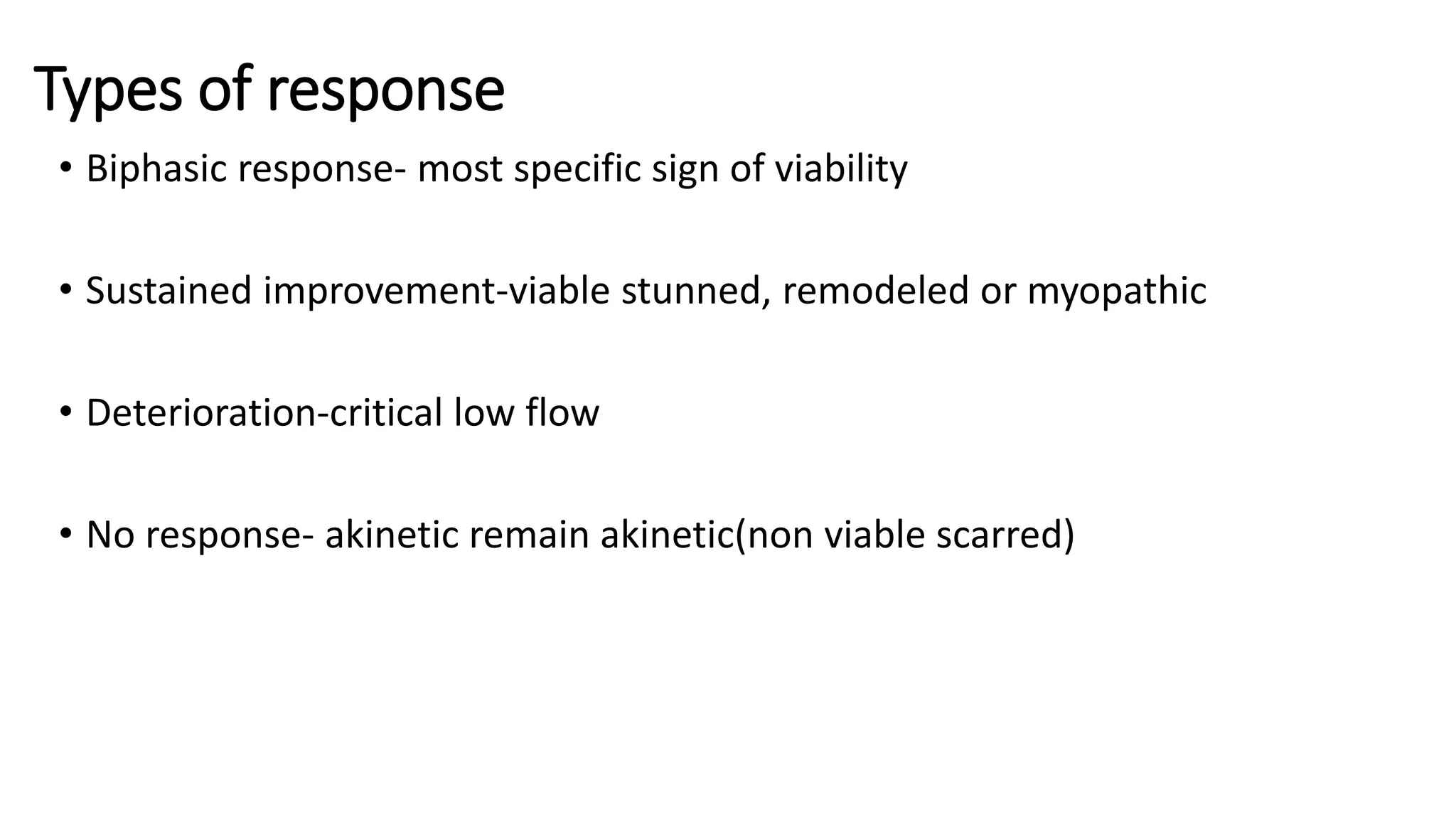
- It is useful for evaluating ischemia, viability, and valvular dysfunction in patients unable to exercise.
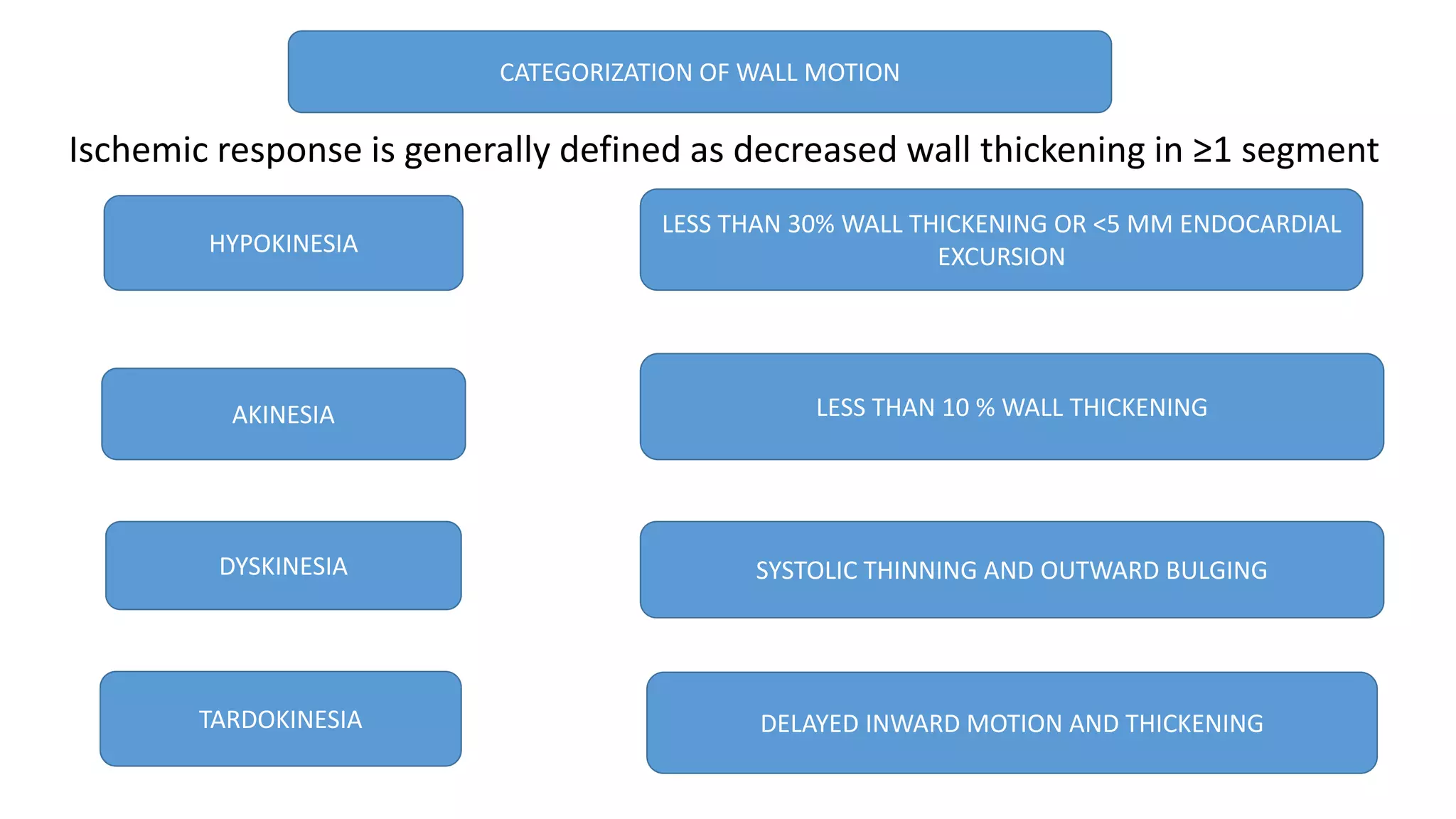
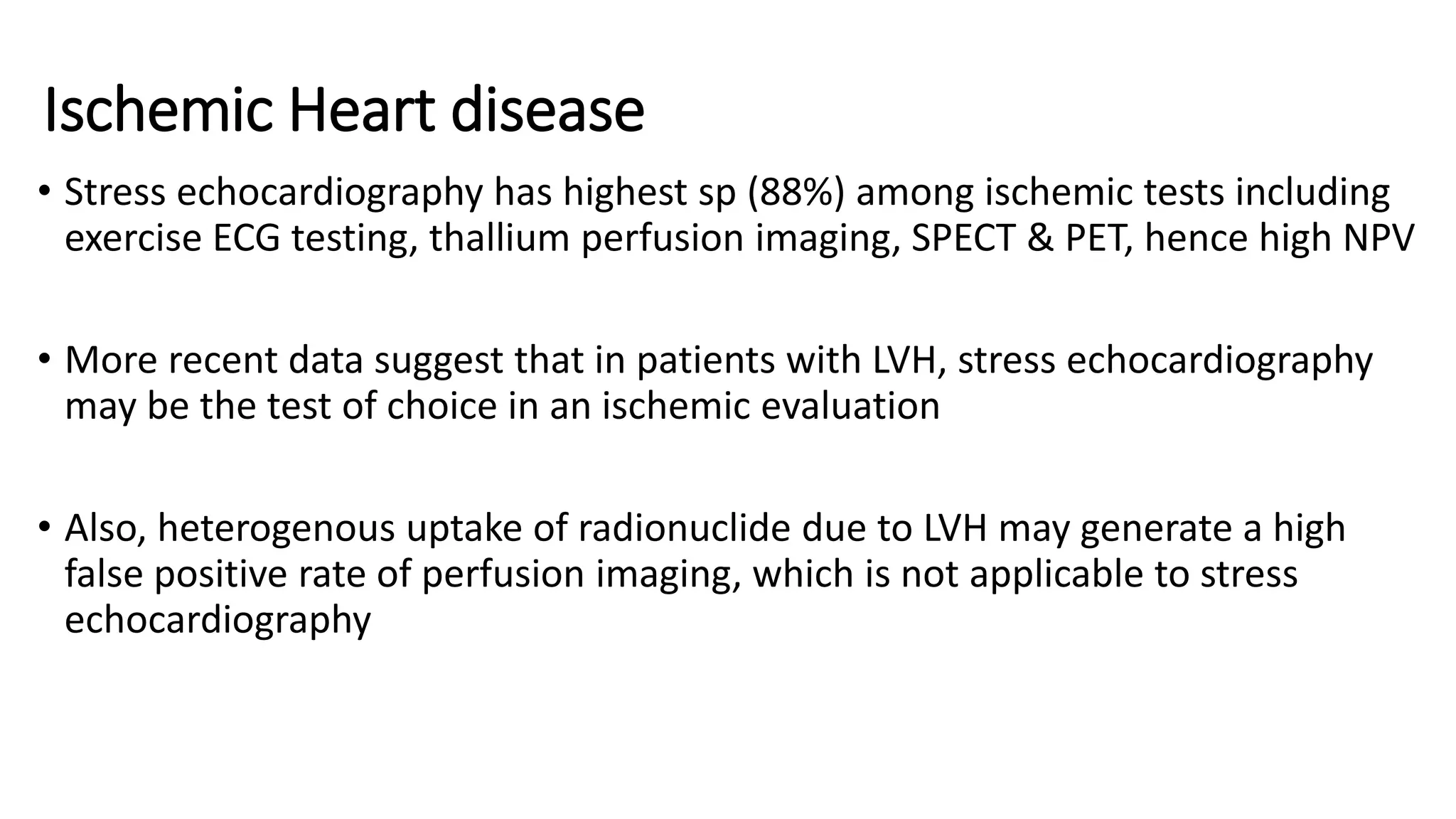
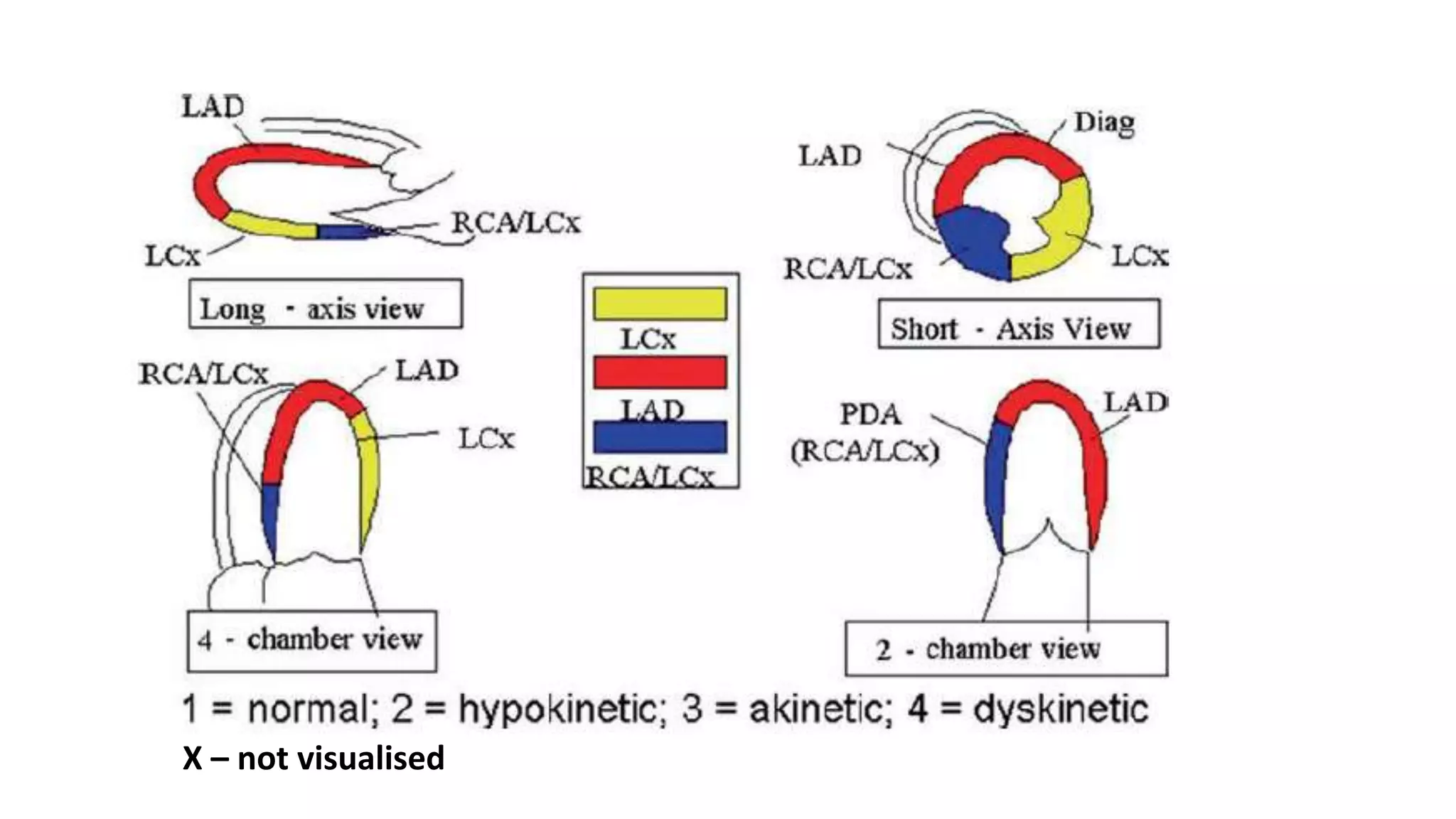
- The document reviews the DSE protocol, interpretation of wall motion abnormalities, indications, side effects, and applications for assessing ischemic heart disease, viability, valvular stenosis like mitral and aortic stenosis, and pulmonary hypertension.