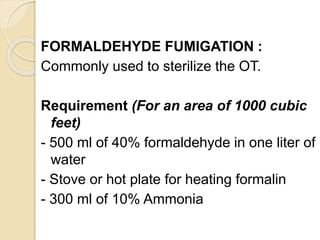
The document discusses disinfection, providing definitions and outlining factors that determine a disinfectant's potency. It describes ideal characteristics for disinfectants and lists common chemical agents used, including their mechanisms and uses. Different levels of disinfection are defined. Specific disinfectants like alcohols, aldehydes, dyes, halogens and phenols are explained in detail. Methods for disinfecting various surfaces and materials are provided.