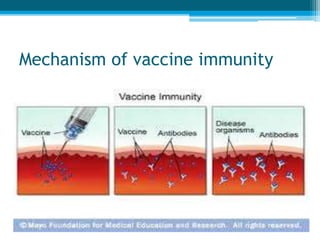
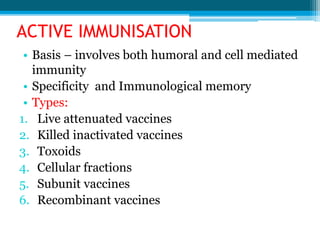
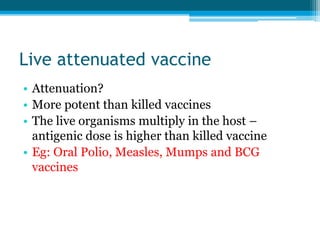
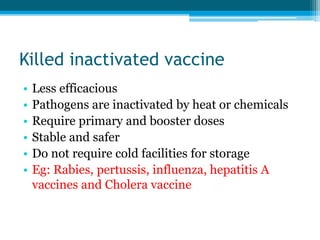
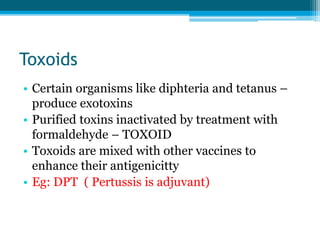
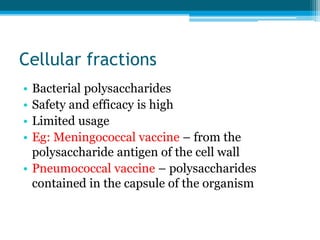
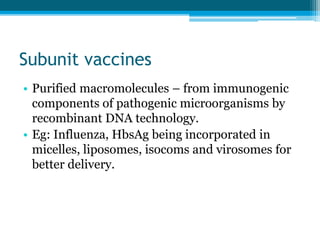
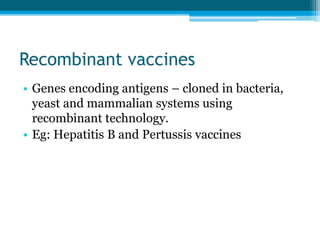
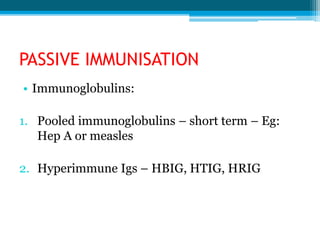
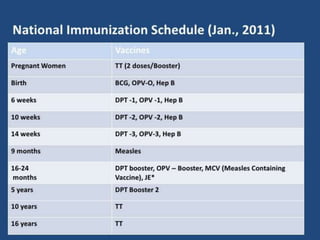
This document discusses immunoprophylaxis and vaccination. It defines prophylaxis and vaccine preventable diseases. There are two types of immunization: active and passive. Active immunization involves inducing immunity through vaccination and works through humoral and cellular immunity. Vaccines can be live attenuated, killed/inactivated, toxoids, cellular fractions, subunit vaccines, or recombinant vaccines. Passive immunization provides immediate short-term protection through administration of antibodies or immunoglobulins. The document also discusses vaccination schedules and recent vaccination missions.