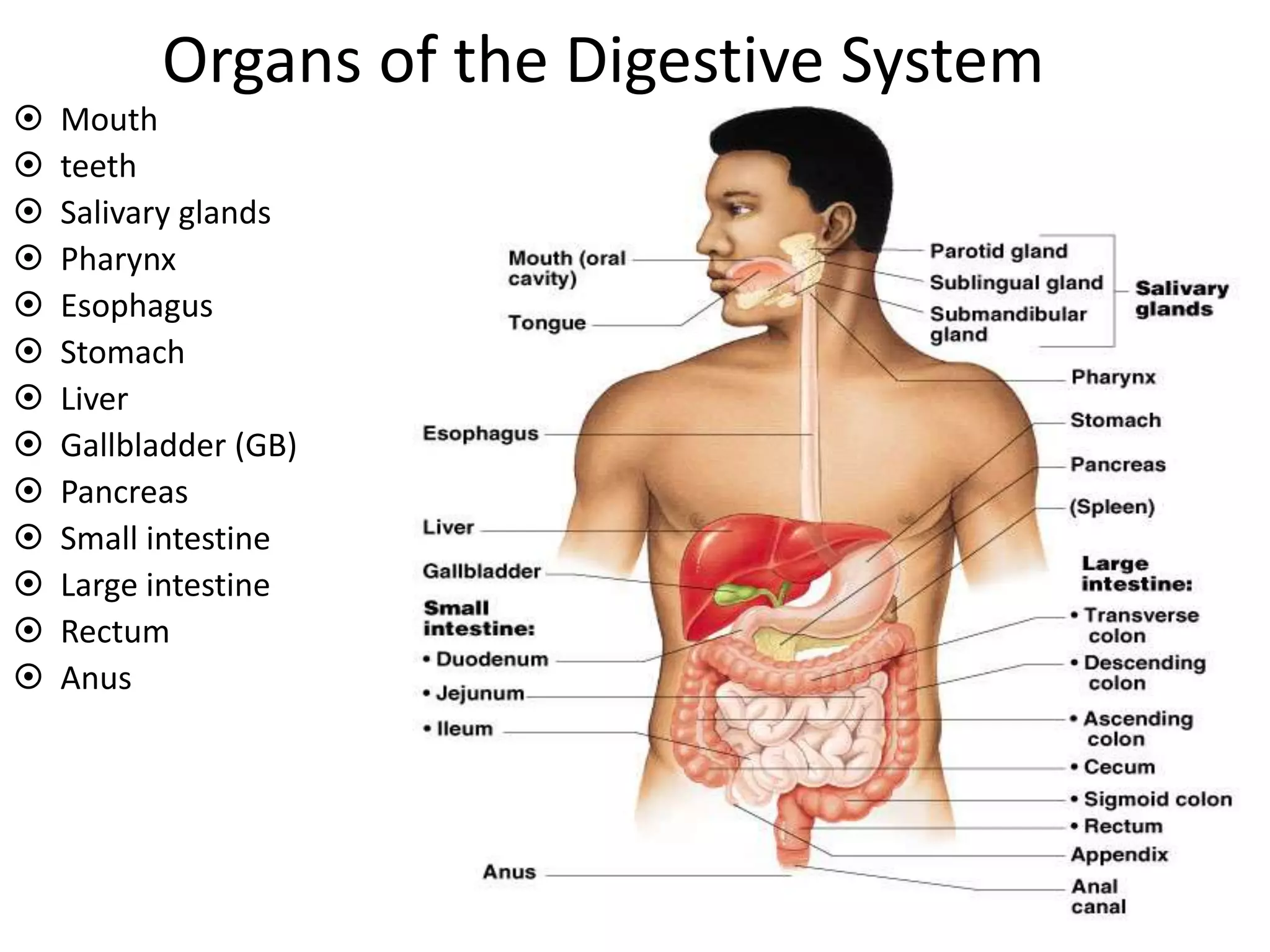
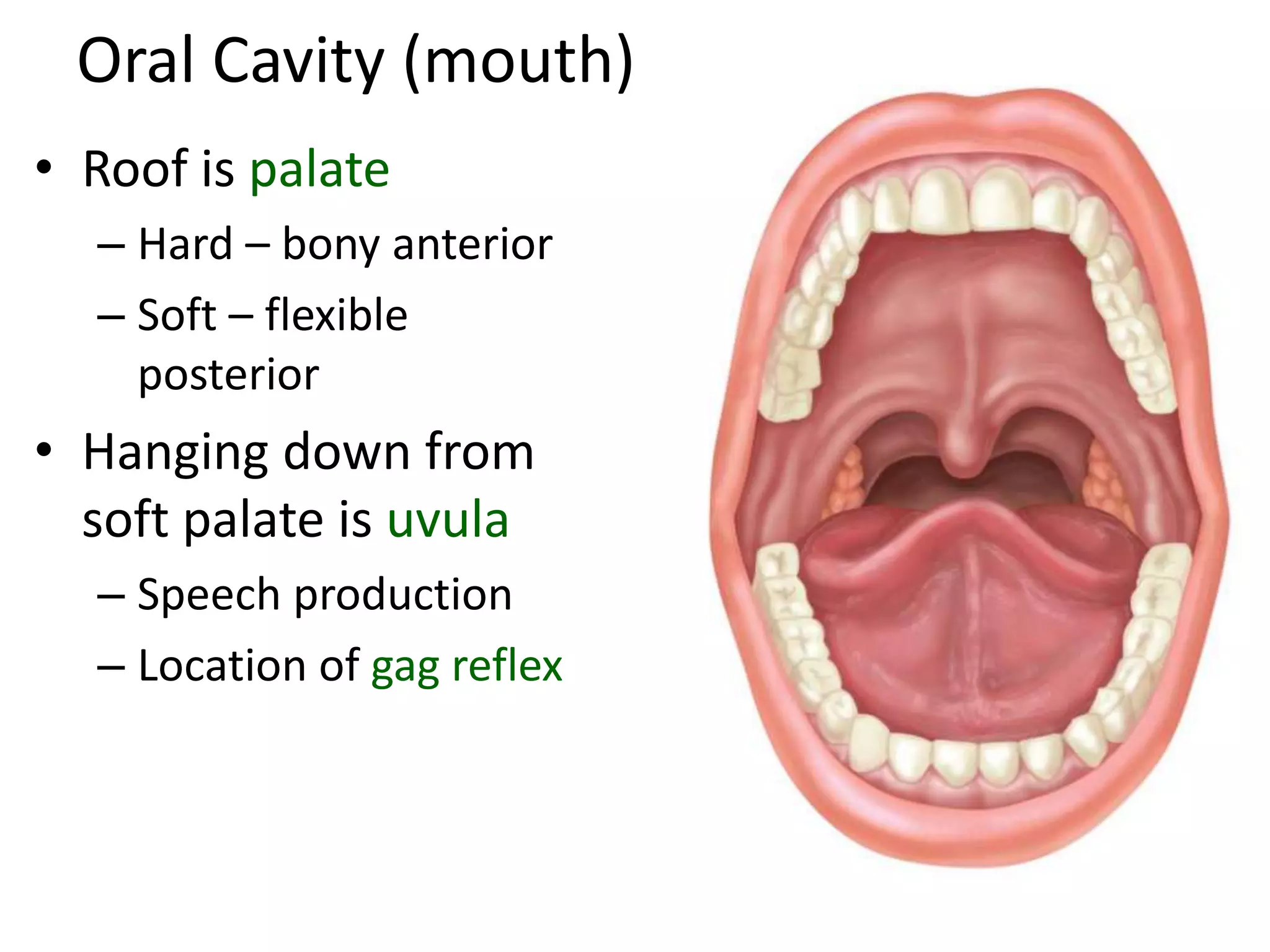
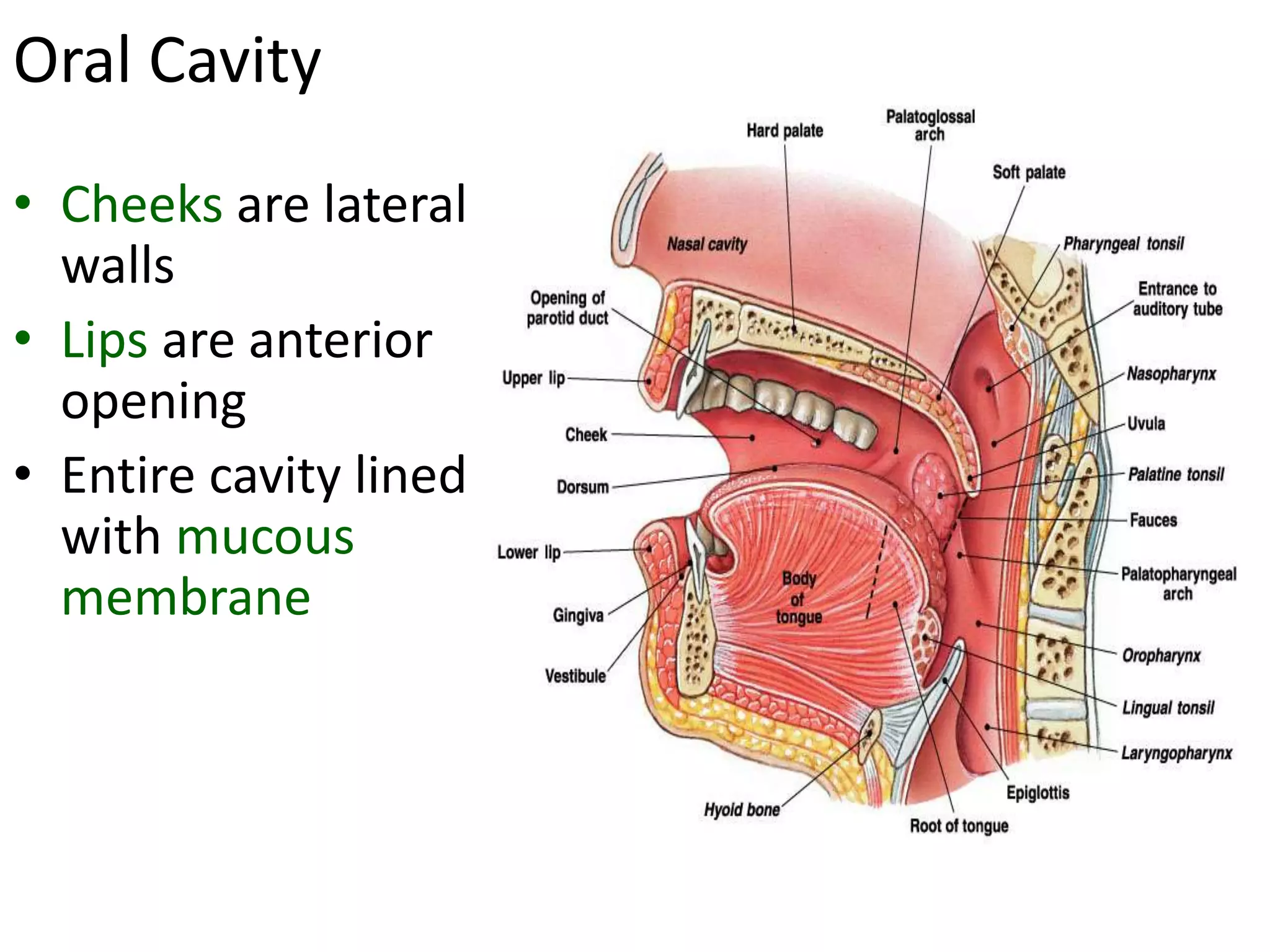
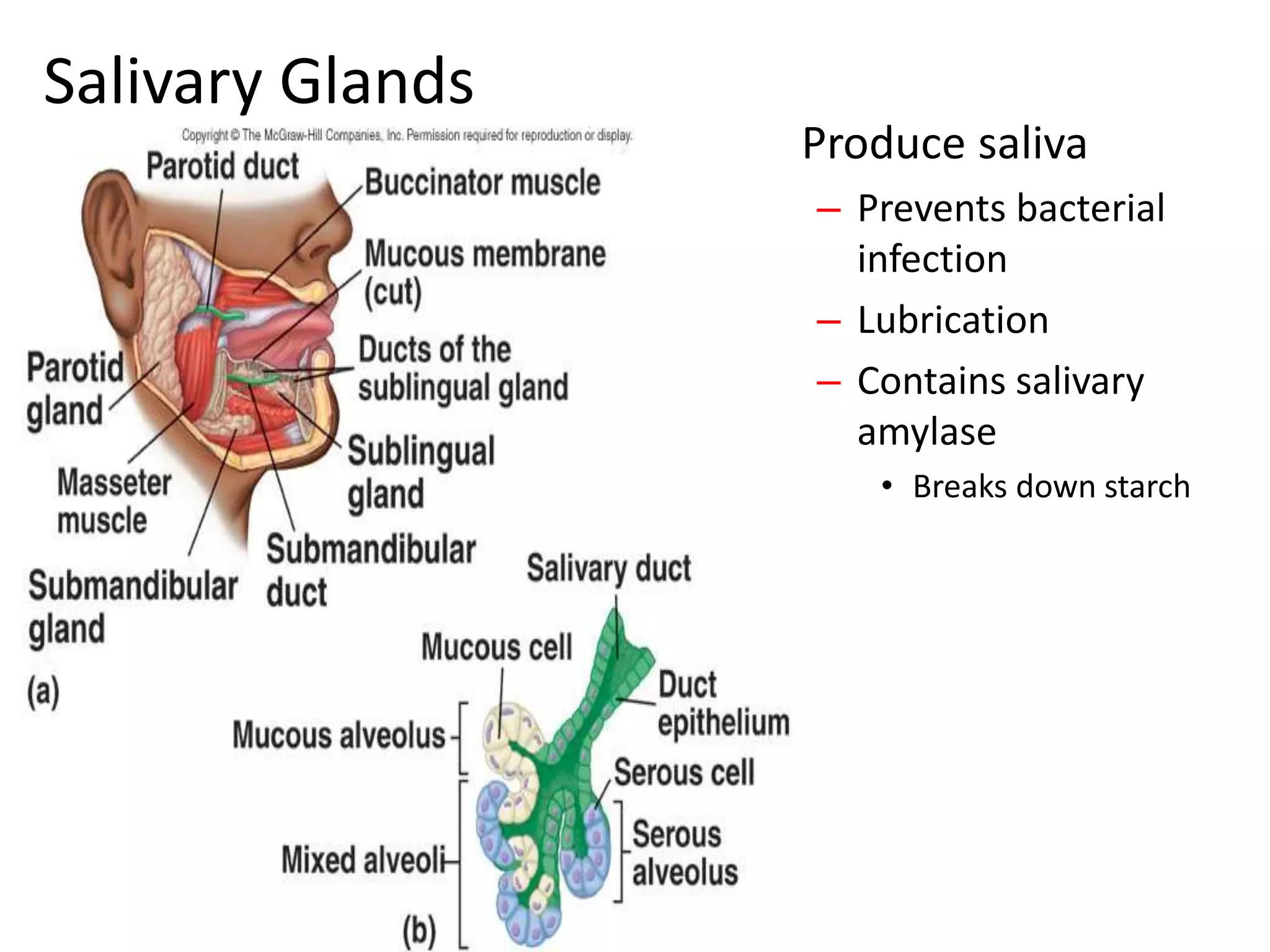
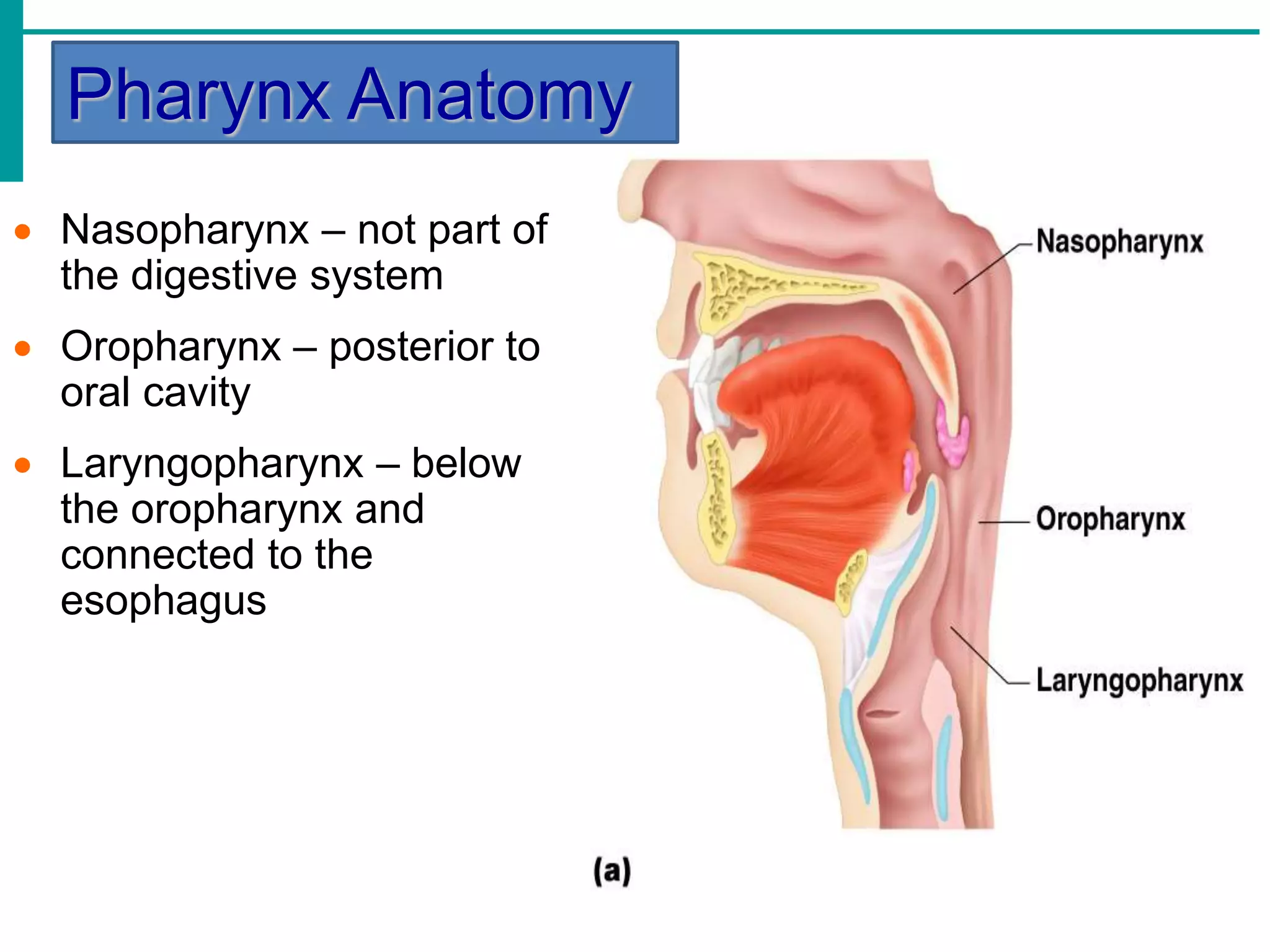
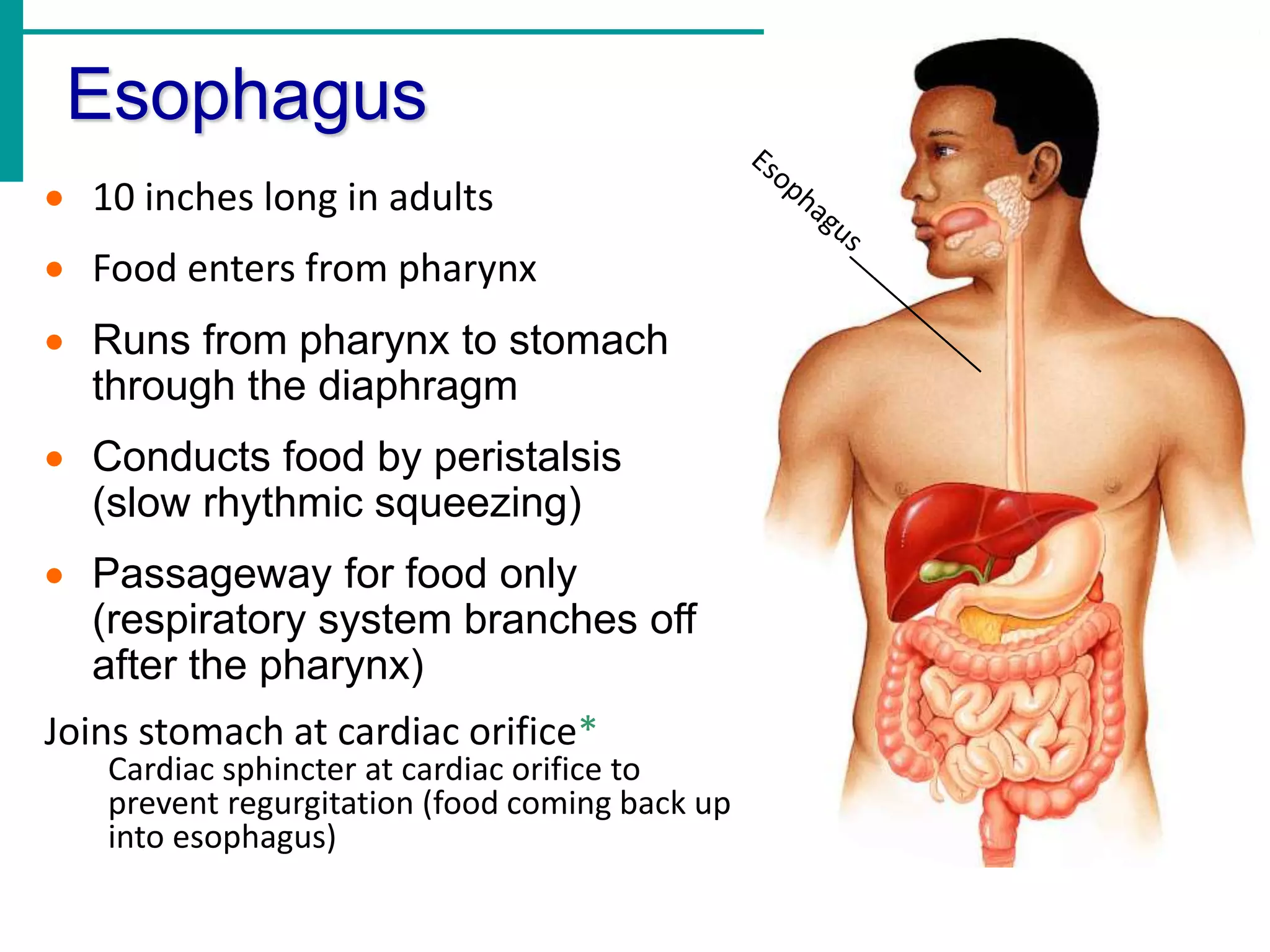
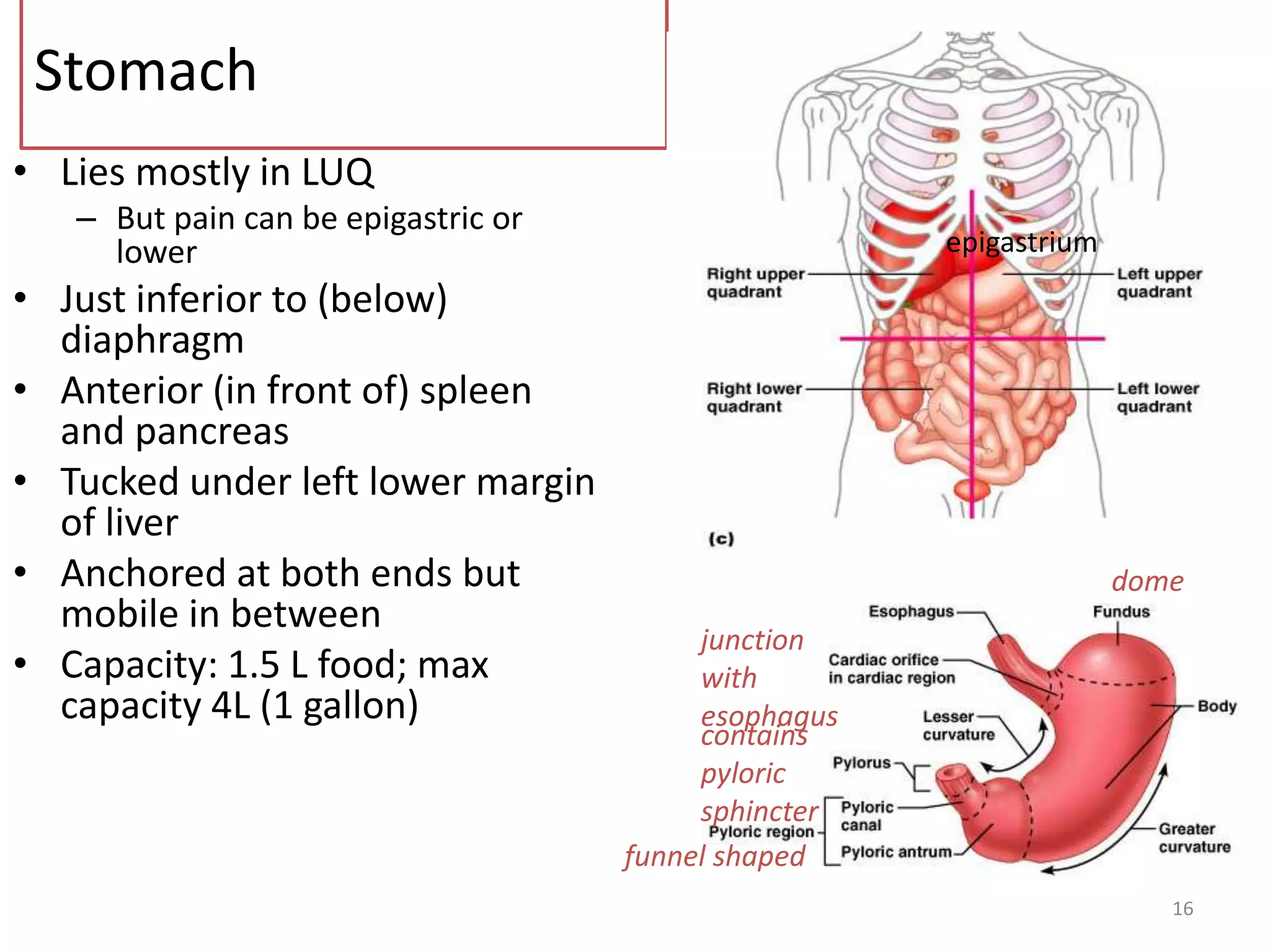
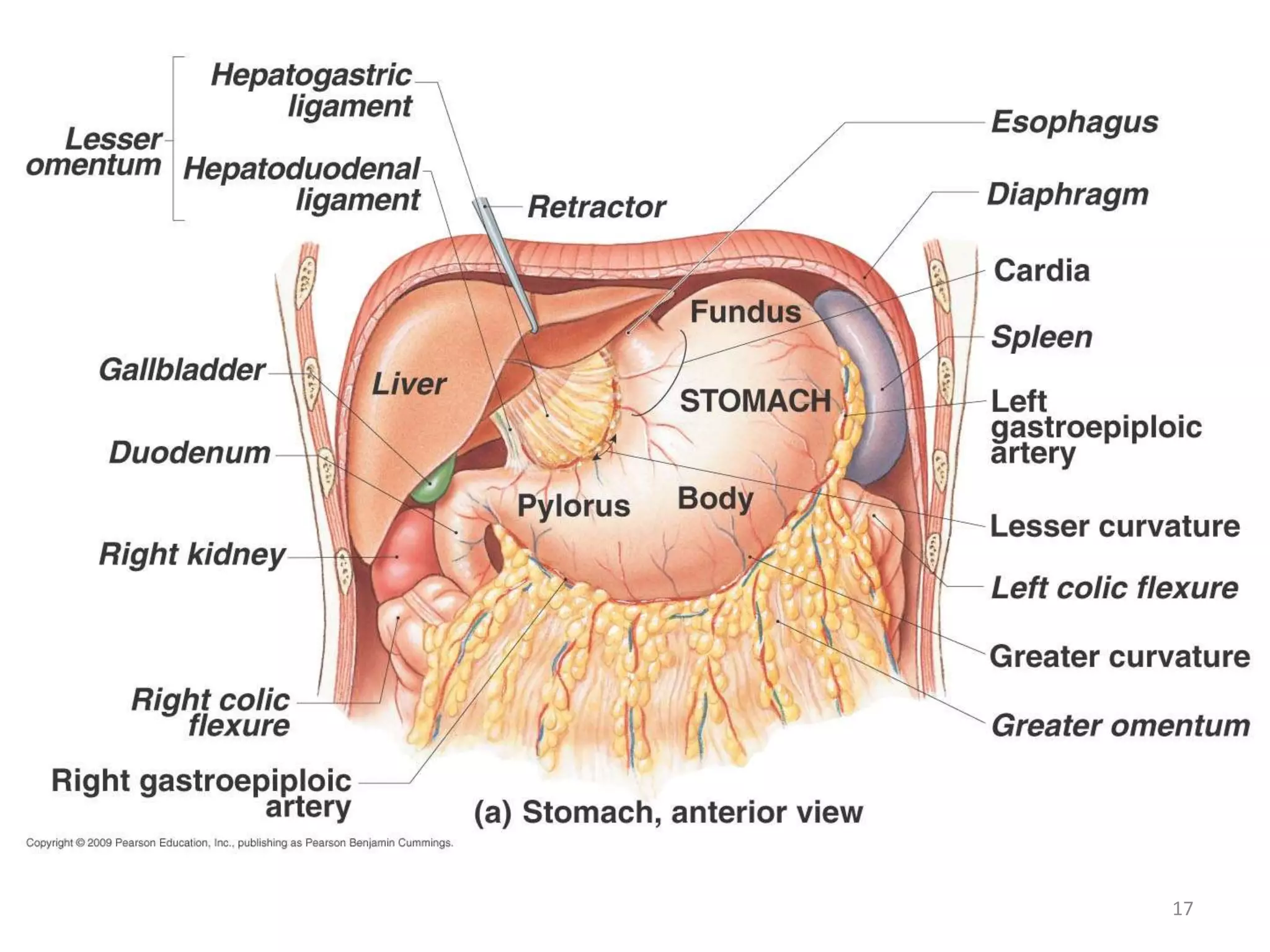
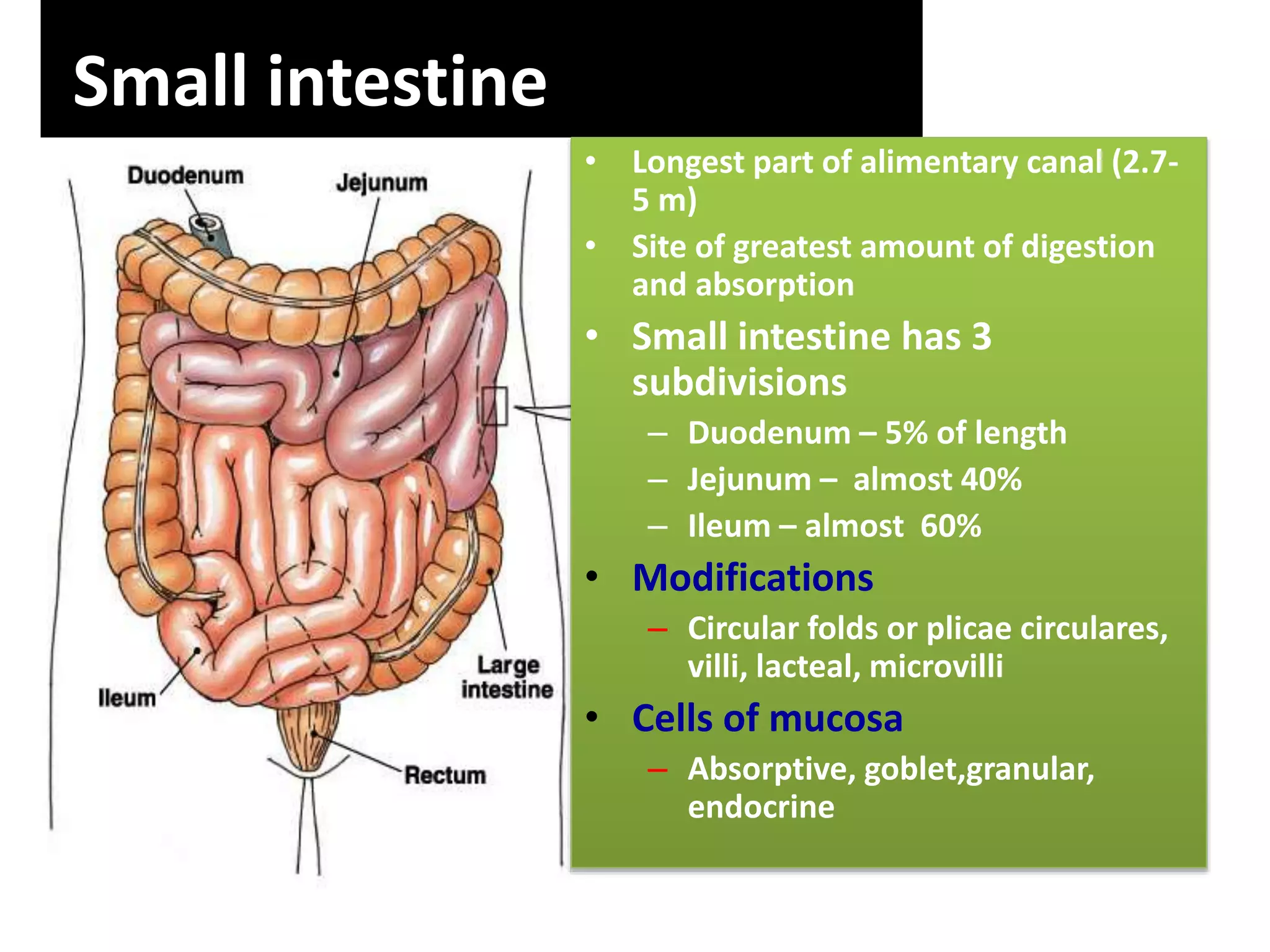
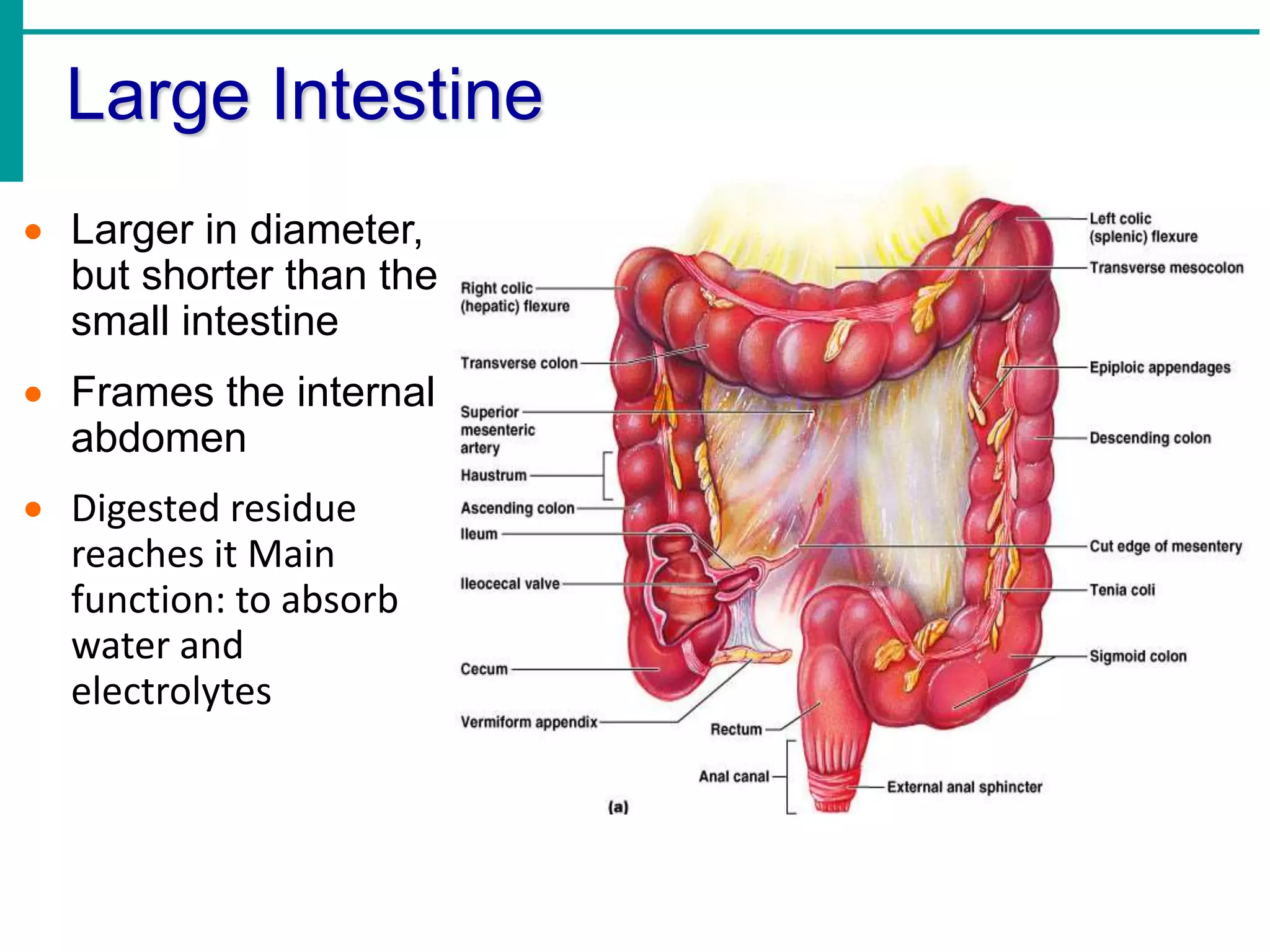
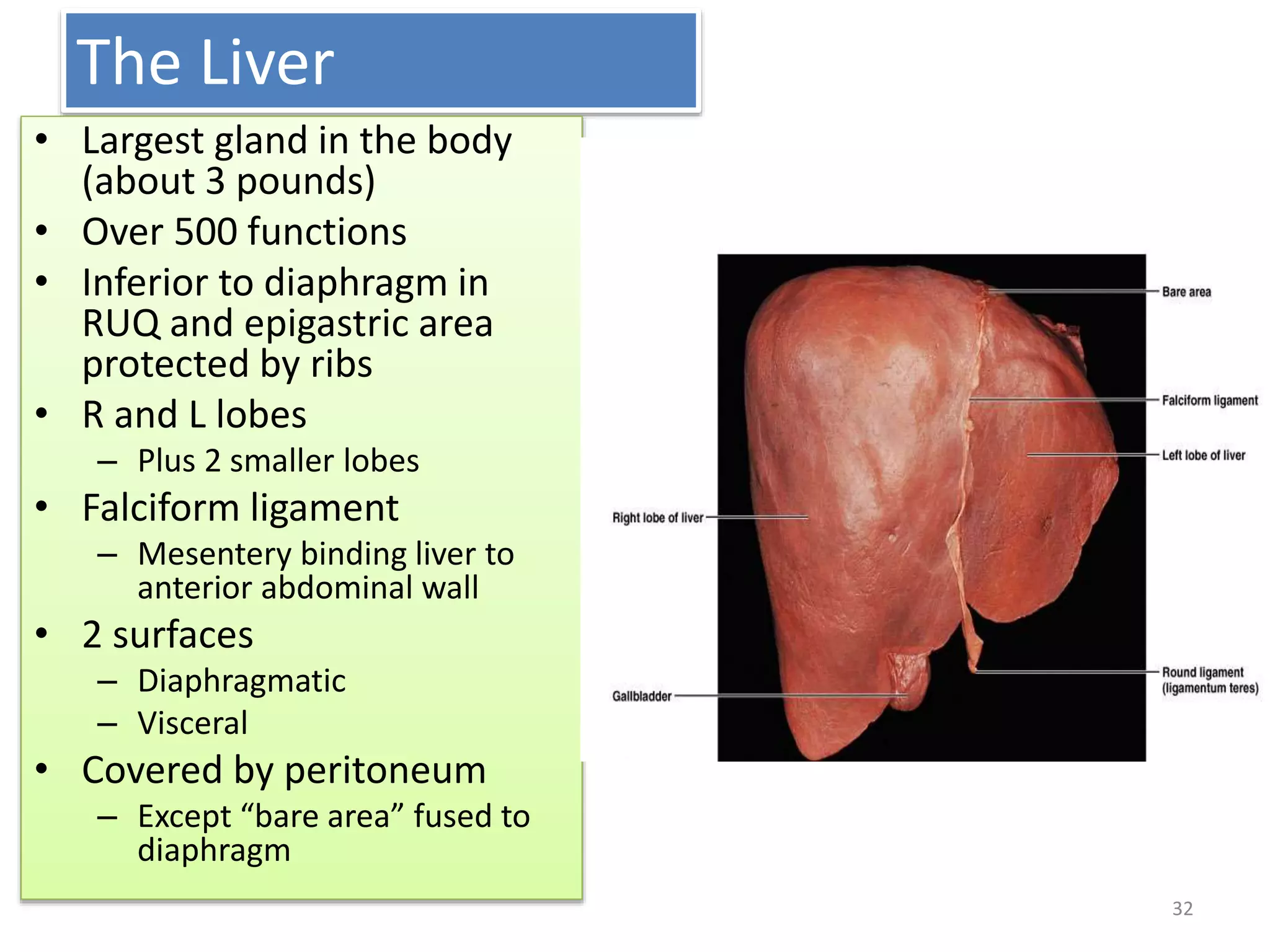
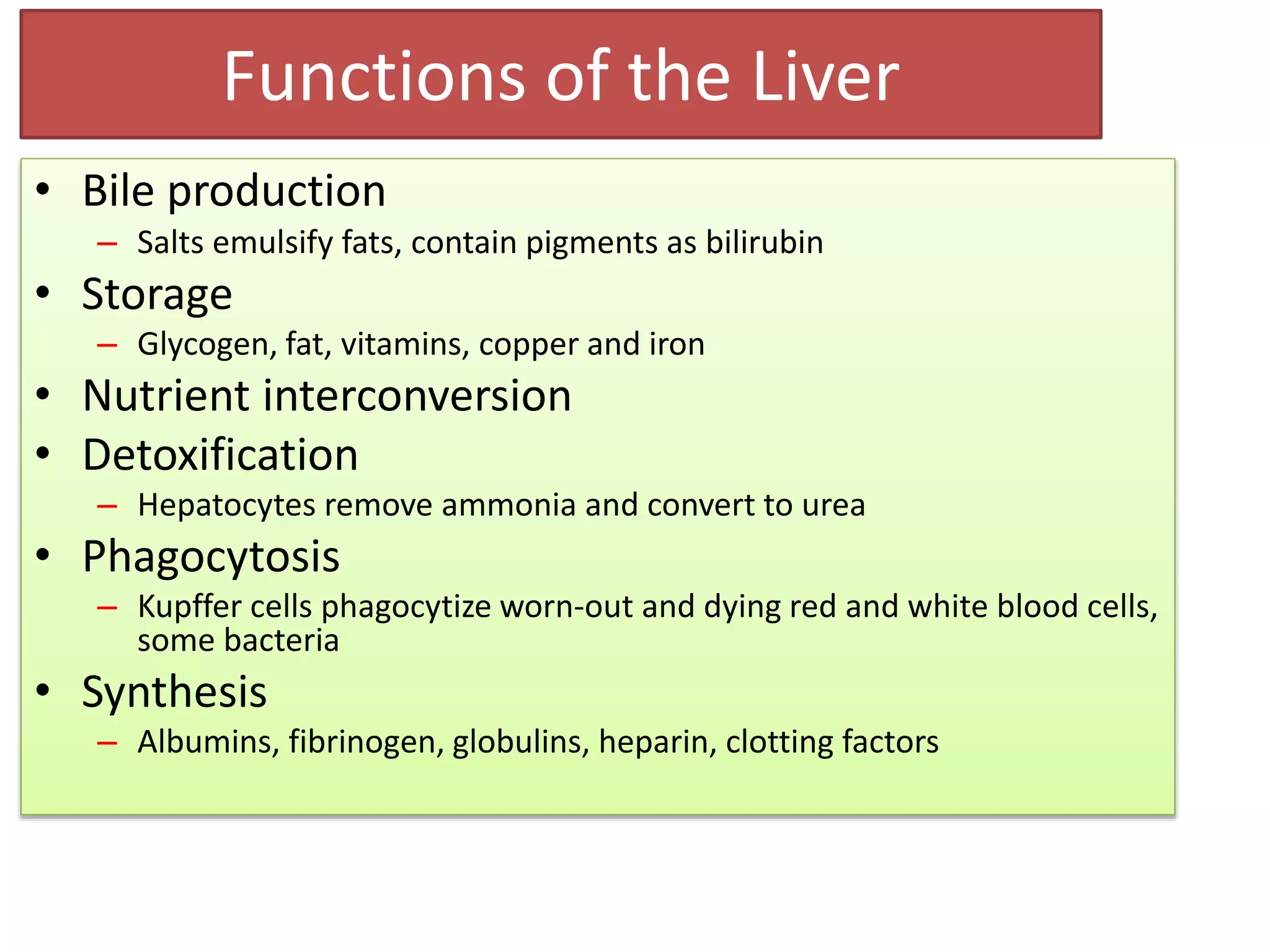
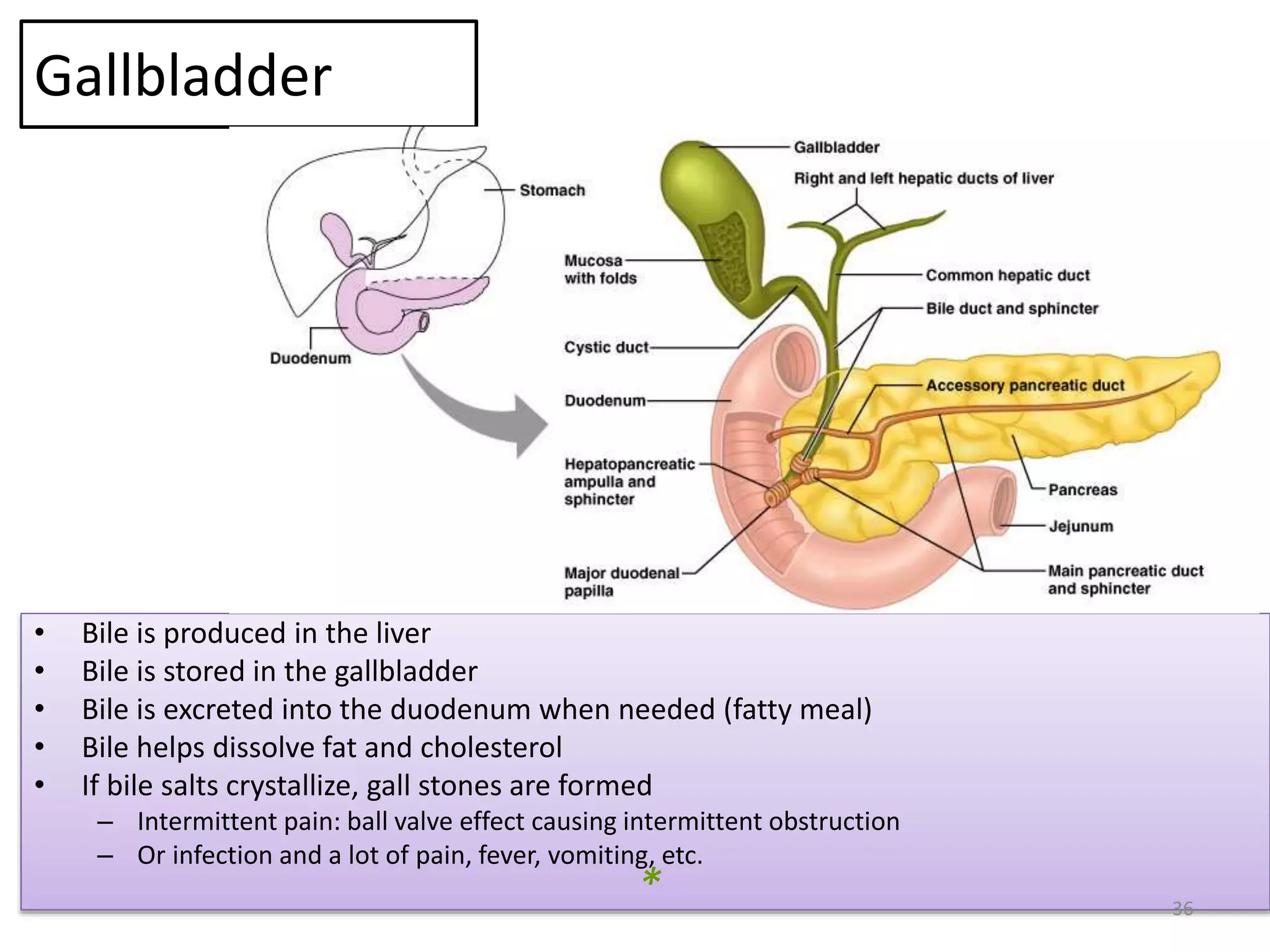
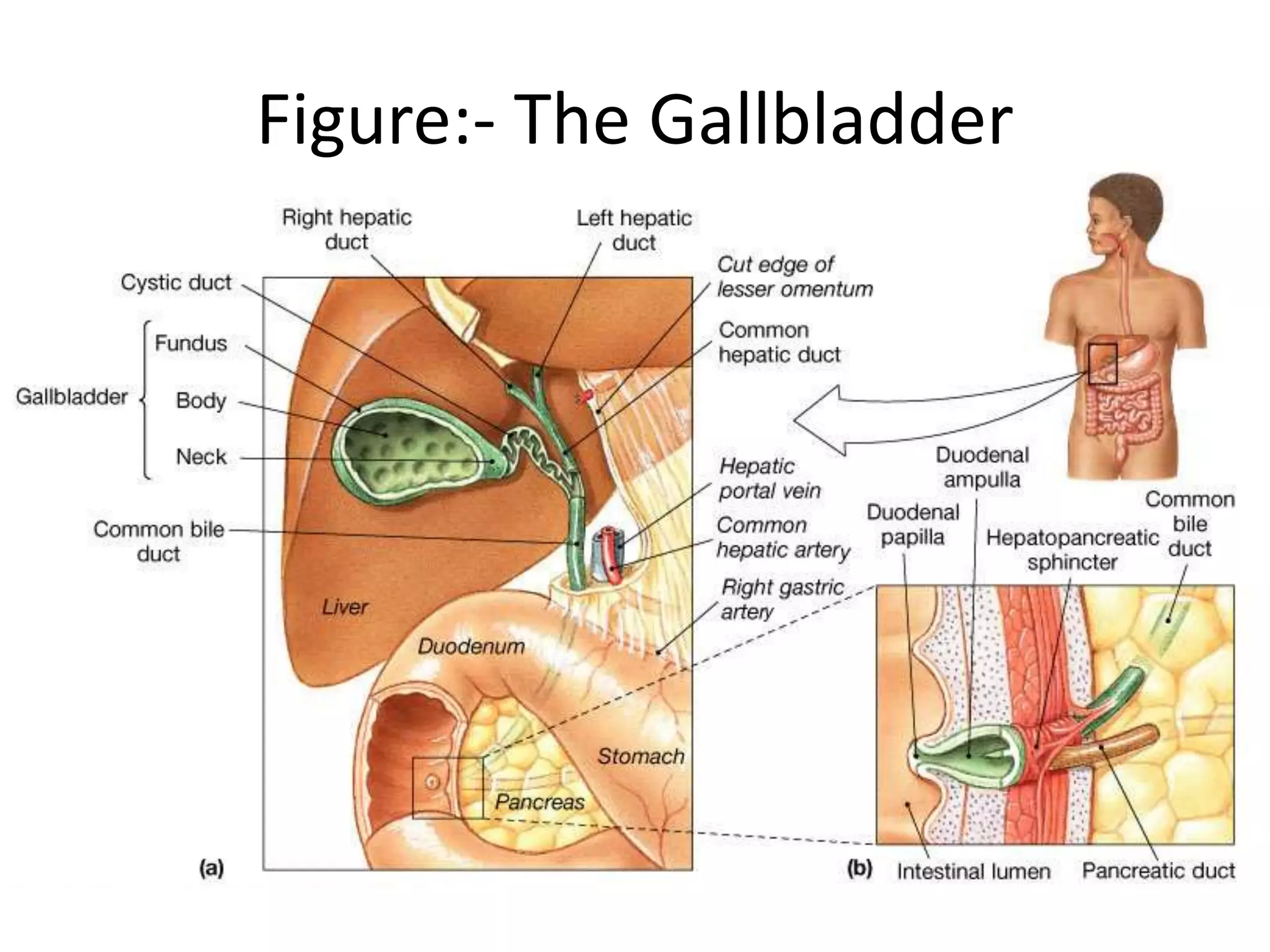
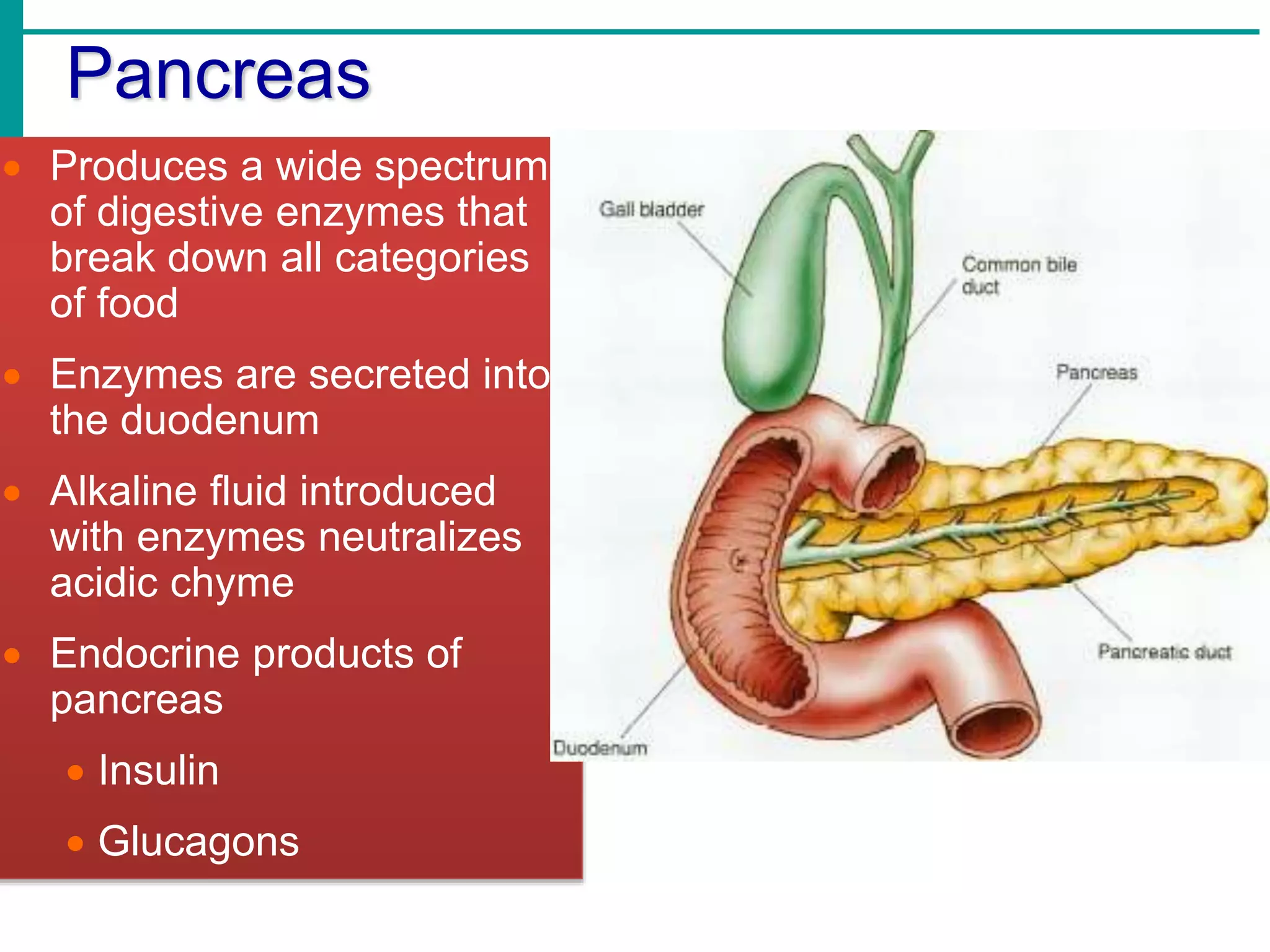
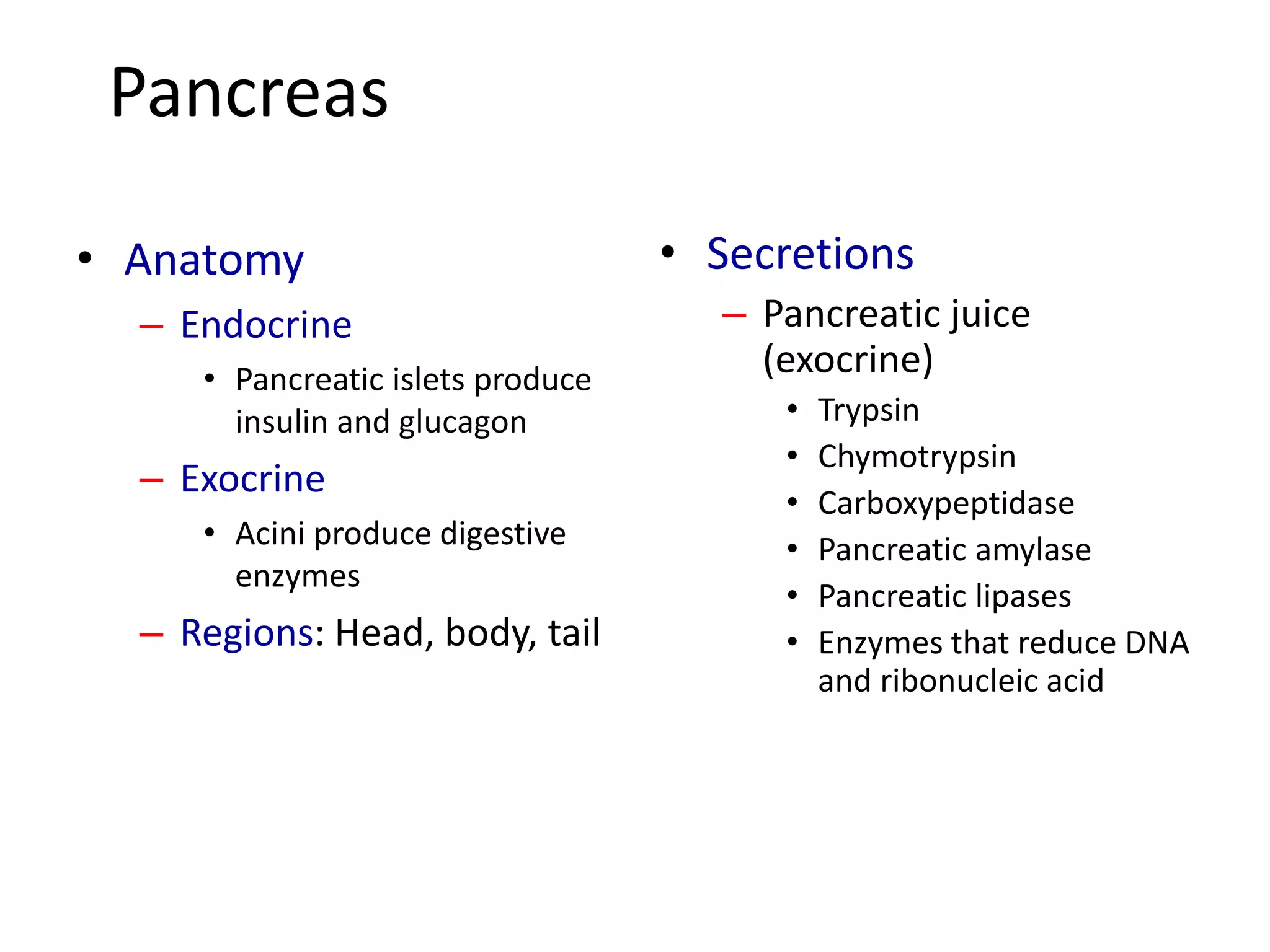
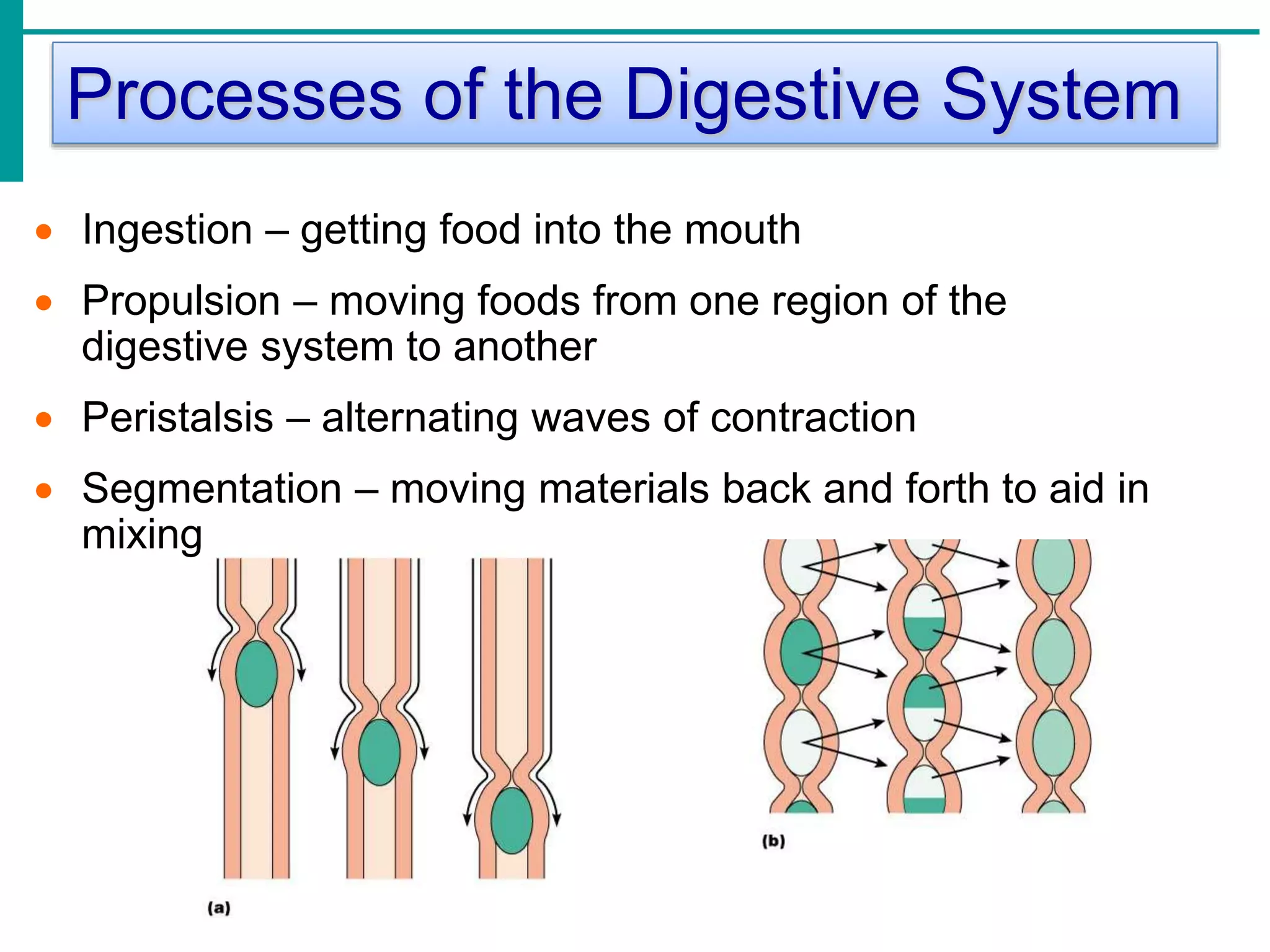
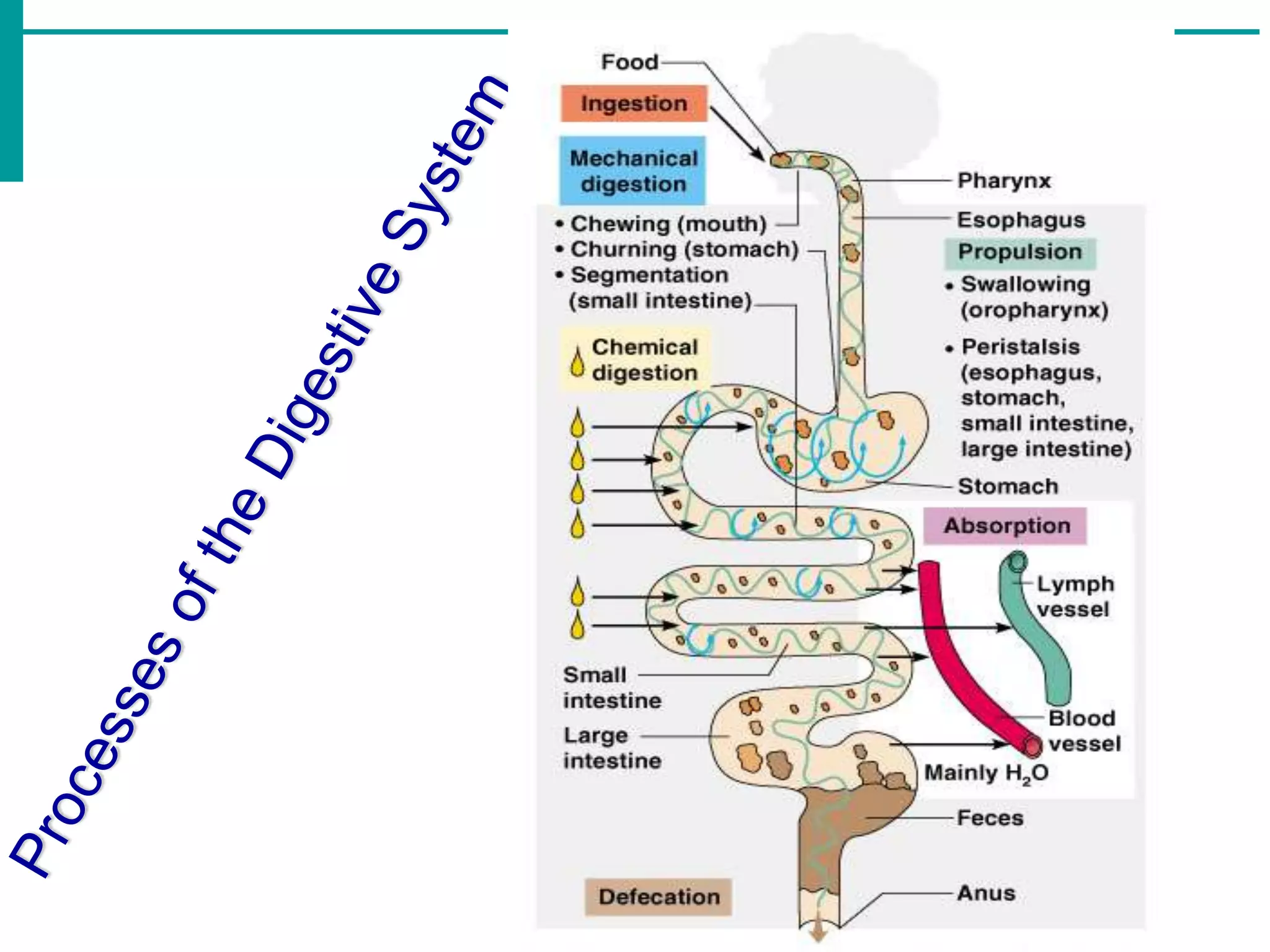
The document describes the anatomy and functions of the digestive system. It lists and describes the major organs of the digestive system including the mouth, esophagus, stomach, small intestine, large intestine, liver, gallbladder and pancreas. It explains the processes of digestion, including mechanical and chemical breakdown of food as well as absorption of nutrients and elimination of waste. It also provides an overview of some common disorders that can affect the digestive system.