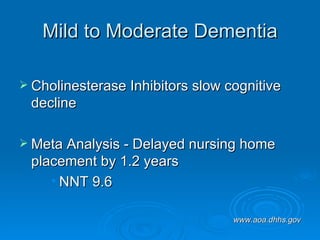
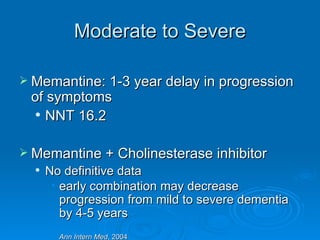
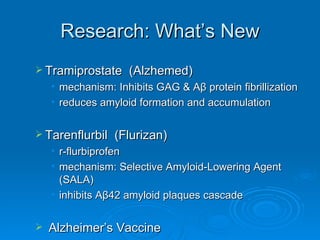
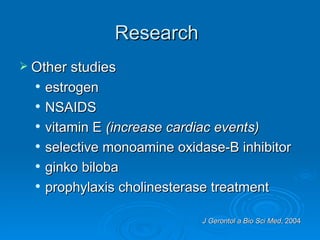
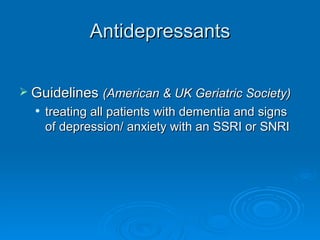
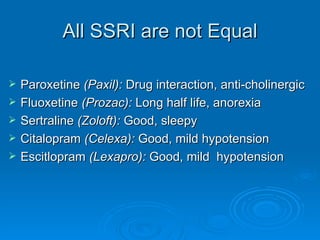
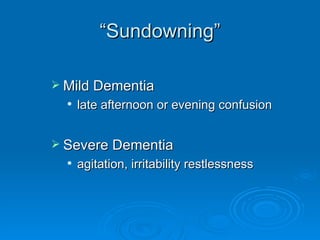
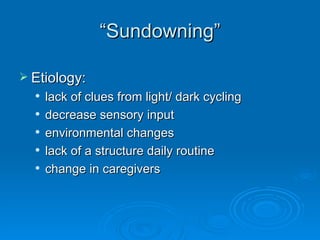
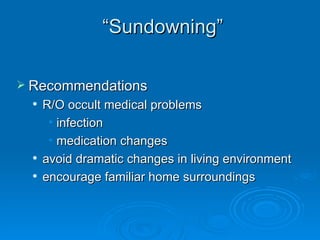
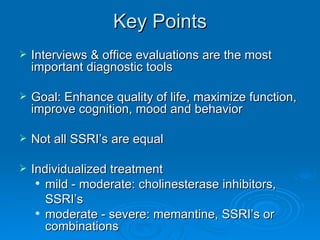
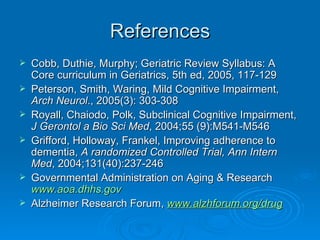
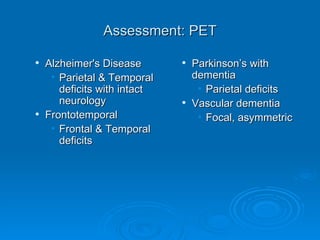
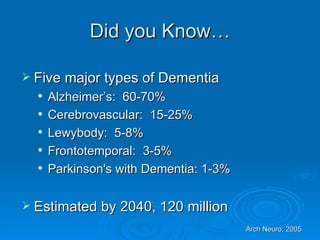
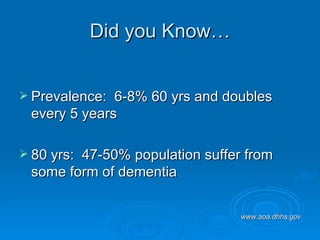
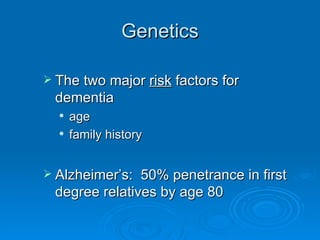
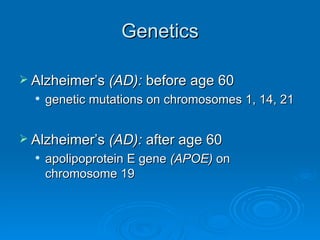
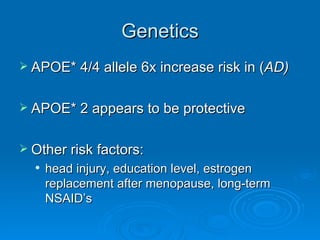
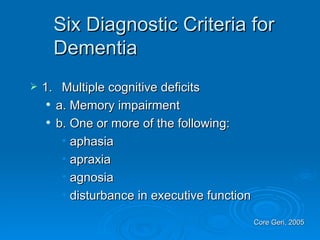
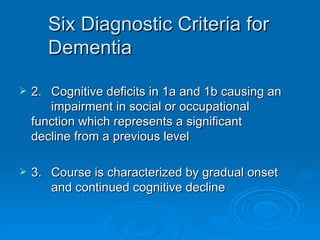
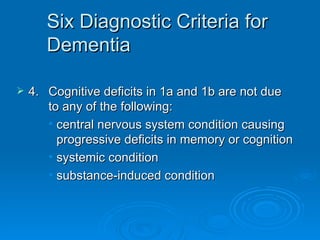
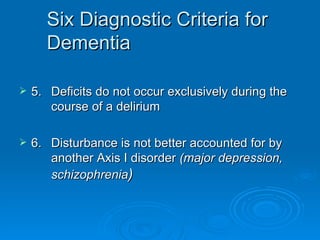
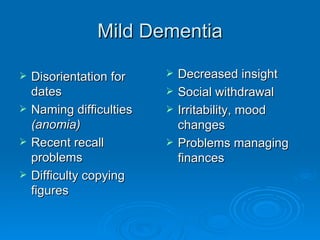
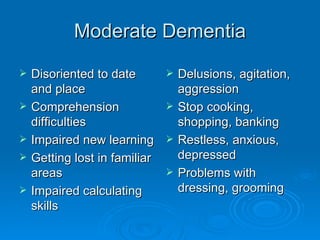
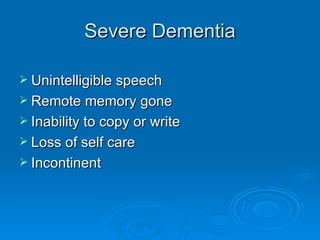
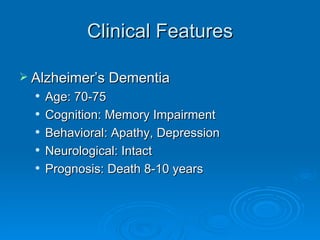
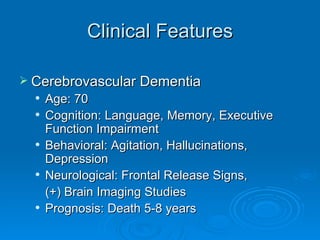
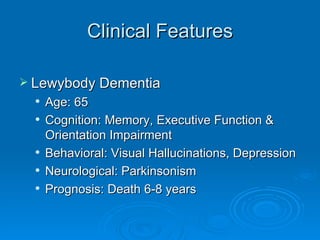
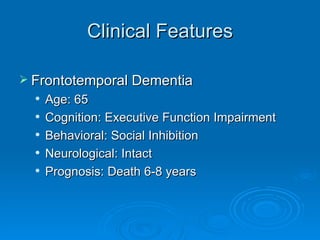
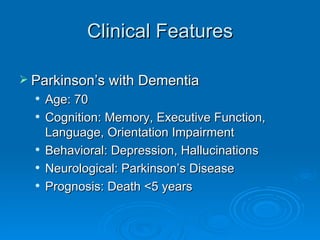
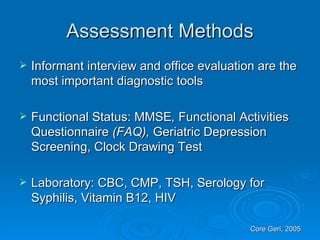
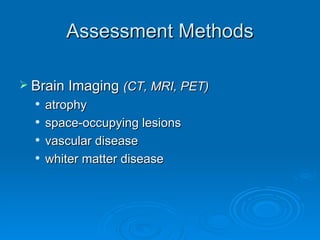
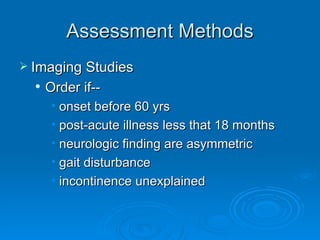
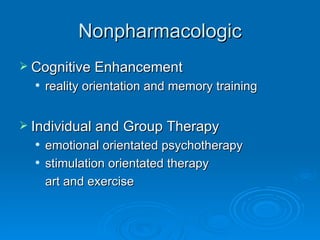
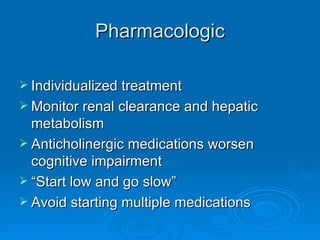
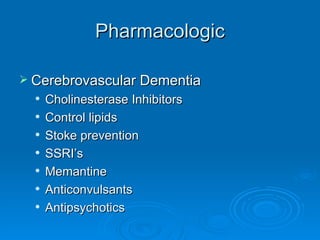
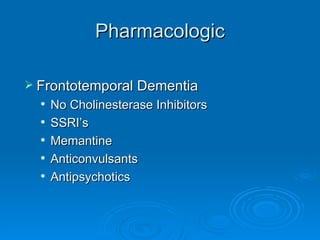
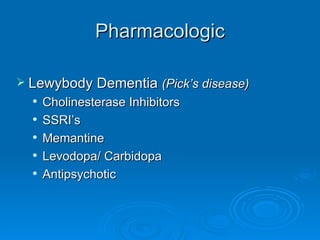
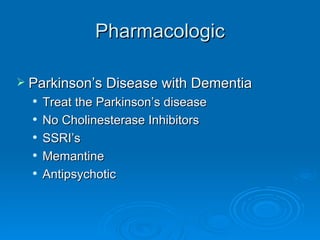
The document discusses dementia, including its various types, symptoms, diagnostic criteria, assessment methods, and treatment options. It defines dementia as the loss of cognitive and intellectual function without impairment of perception or consciousness. The five major types of dementia are Alzheimer's disease, cerebrovascular disease, Lewy body disease, frontotemporal dementia, and Parkinson's disease with dementia. Assessment involves interviews, examinations, and tests to evaluate cognition, function, and rule out other conditions. Treatment focuses on enhancing quality of life and includes both non-pharmacological and pharmacological approaches.




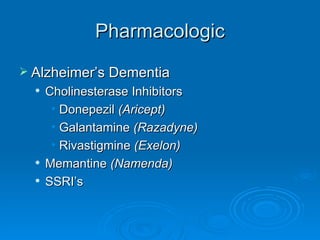
![NMDA [glutamate] antagonist Memantine (Namenda) Precautions : Dizziness, headache, alkalinized urine (ATN, UTI) seizures, GI upset Interactions : Other NMDA antagonists (amantadine, dextromethorphan), decreased by renally-excreted drugs (HCTZ)](https://image.slidesharecdn.com/dementia2-1233828203041668-3/85/Dementia-2-44-320.jpg)