The document discusses epilepsy and its management. Some key points:
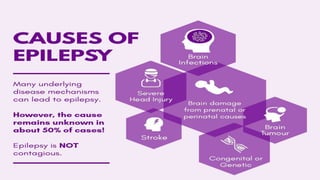
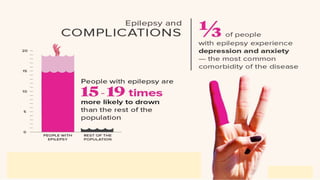
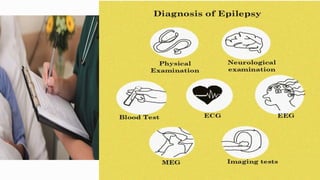
- Epilepsy is a chronic neurological disorder characterized by recurrent seizures. It affects around 50 million people worldwide.
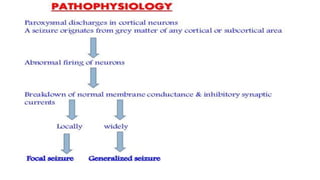
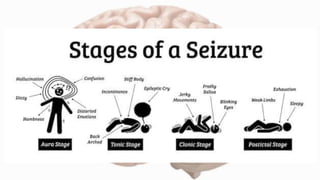
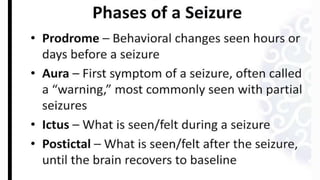
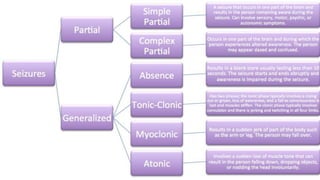
- Seizures occur due to excessive electrical discharges in the brain and present with symptoms like loss of consciousness and abnormal motor movements.
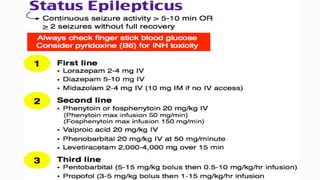
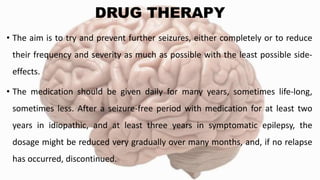
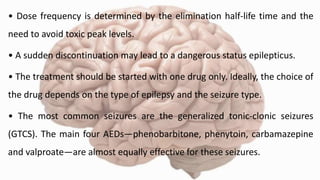
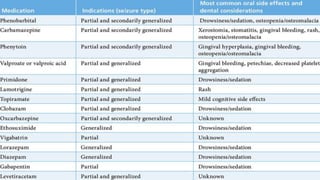
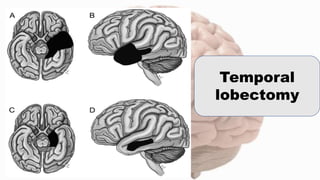
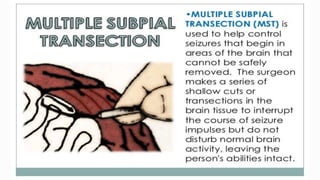
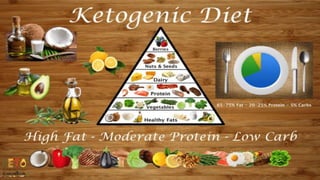
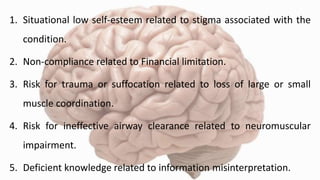
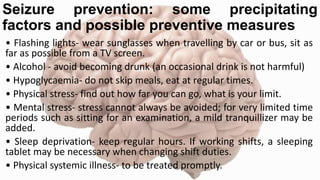
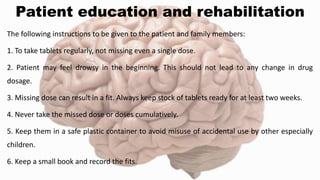
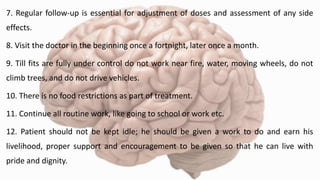
- Management involves anti-epileptic drug therapy to control seizures as well as addressing psychosocial issues like stigma and quality of life concerns. Surgery may be considered if drug therapy is ineffective. Nursing care includes education, monitoring for side effects, and supporting psychological well-being.









![REFERENCES
1. Janice L. Hinkle, Kerry H. Cheever. Brunner and Suddarth’s Textbook of Medical
Surgical Nursing. 2015. New Delhi. Wolters Kluwer.13th Edition. Volume 2. Pg. no.
2. Lewis. Medical Surgical Nursing Assessment and Management of clinical
problems.2015. New Delhi. Elsevier. 2nd Edition. Volume II. Pg. no. 1495-1497.
3. Joyce M. Black, Jane Hokanson Hawks. Medical Surgical Nursing Clinical
Management of Positive Outcomes.2015. New Delhi. Reed Elsevier India Private
Limited. Volume II. Pg. No. 1916-1918.
4. TP Prema, KF Graicy. Essentials of Neurological and Neurosurgical Nursing.
2013.New Delhi. Jaypee Brothers Medical Publishers. Pg. no. 145-155.
5.World Health Organization. Epilepsy. Key facts. Available from
https://www.who.int/news-room/fact-
sheets/detail/epilepsy#:~:text=Around%2050%20million%20people%20worldwide%2
0have%20epilepsy%2C%20making%20it%20one,if%20properly%20diagnosed%20and
%20treated. [cited 27 Nov 2020]](https://image.slidesharecdn.com/epilepsy-210128185105/85/Epilepsy-and-its-management-52-320.jpg)
![6.World Health Organization. Epilepsy: A manual for Medical and clinical officers
in Africa. Available from
https://www.who.int/mental_health/media/en/639.pdf?ua=1 [cited 27 Nov
2020]
7. Garg D. Specific considerations for epilepsy in India. Curr Med Issues [serial
online] 2020 [cited 2020 Nov 27];18:105-10. Available from:
https://www.cmijournal.org/text.asp?2020/18/2/105/282783
8. Medical News Today. [cited 11 jan 2020] Available from
https://www.medicalnewstoday.com/articles/8947.php#treatment
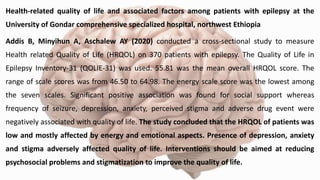
9. Addis B, Minyihun A, Aschalew AY. Health-related quality of life and associated
factors among patients with epilepsy at the University of Gondar comprehensive
specialized hospital, northwest Ethiopia. Qual Life Res. 2020 Oct 18. [cited 5 Nov
2020] doi: 10.1007/s11136-020-02666-4. Epub ahead of print. PMID: 33070287.
10. Ayanda KA, Sulyman D. Determinants of quality of life in adults living with
epilepsy. Ann Afr Med. 2020 Jul-Sep;19(3):164-169. [cited 5 Nov 2020] doi:
10.4103/aam.aam_20_18. PMID: 32820727.](https://image.slidesharecdn.com/epilepsy-210128185105/85/Epilepsy-and-its-management-53-320.jpg)

