This document provides information on smoking cessation and motivational interviewing techniques to help patients quit smoking. It discusses:
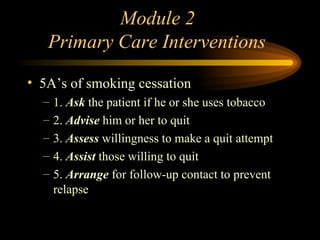
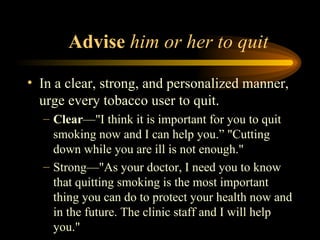
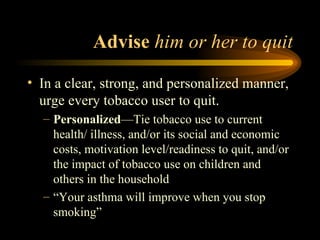
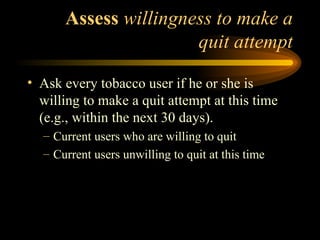
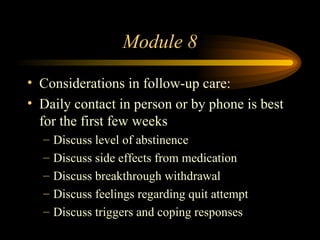
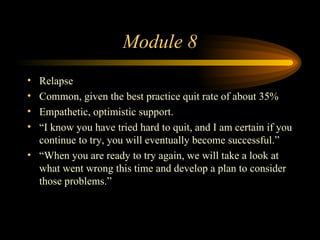
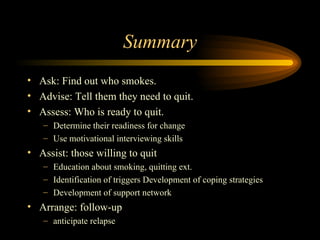
- The 5 A's approach to smoking cessation in primary care (Ask, Advise, Assess, Assist, Arrange).
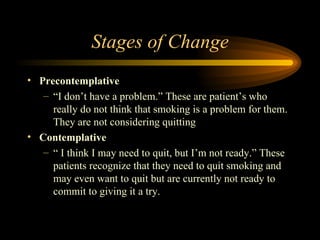
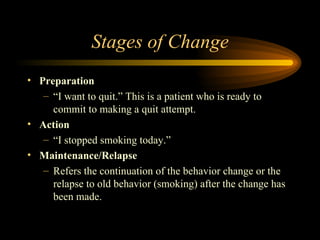
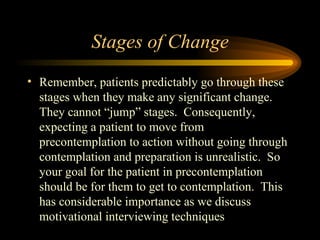
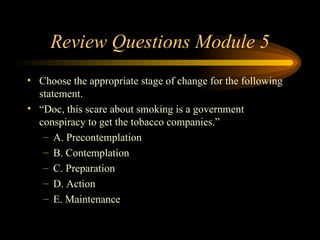
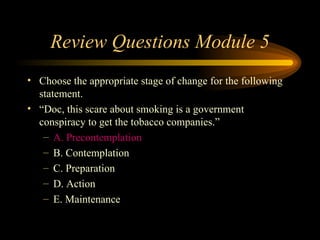
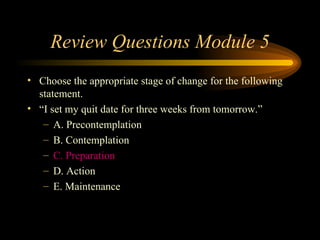
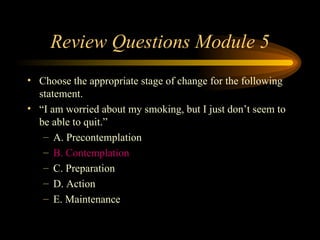
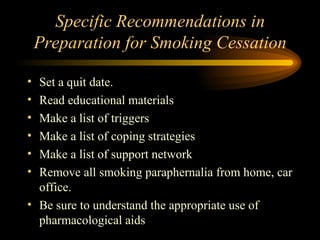
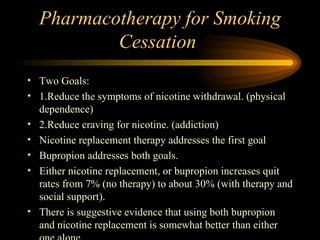
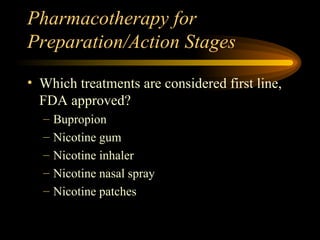
- Stages of change model for behavior change, including precontemplation, contemplation and preparation stages.
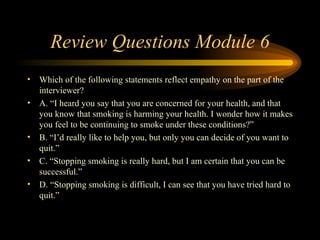
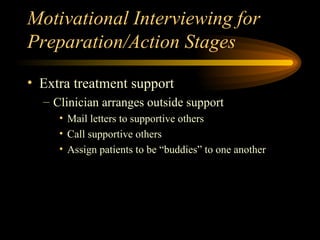
- Motivational interviewing techniques like expressing empathy, developing discrepancy, avoiding arguments and rolling with resistance to help move patients through the stages of change.
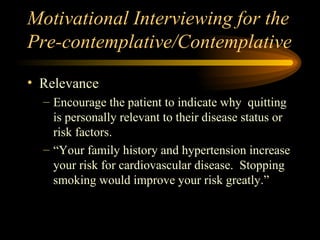
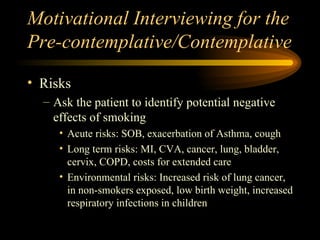
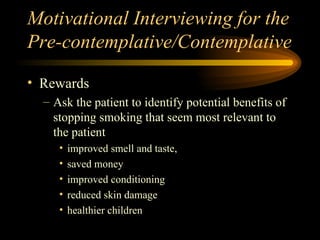
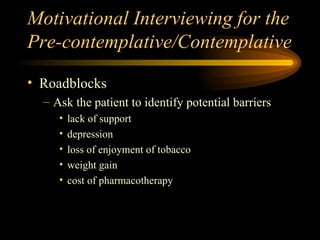
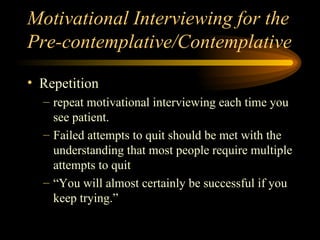
- Using the 5 R's of relevance, risks, rewards, roadblocks and repetition when motivational interviewing with precontemplative and contemplative patients.