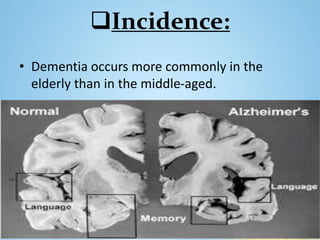
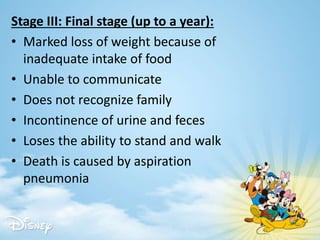
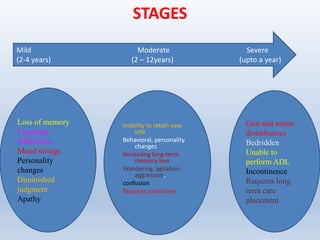
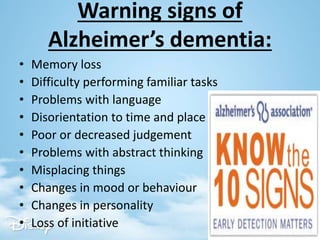
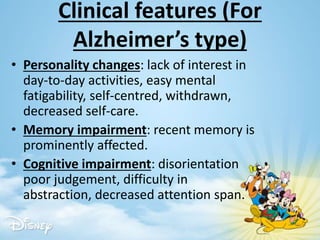
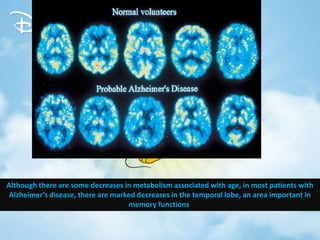
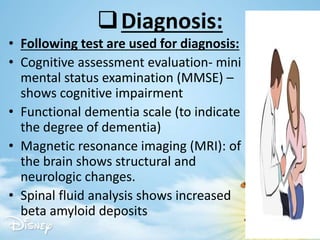
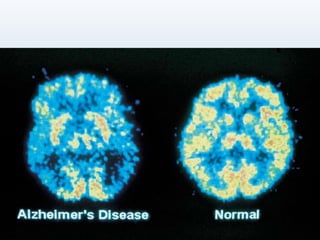
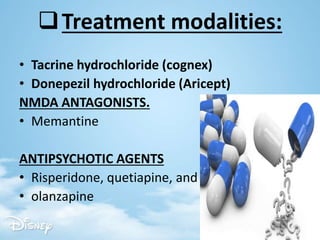
The document provides a comprehensive overview of dementia, including its definition, classification, historical context, and various causes. It outlines types and stages of dementia, warning signs, clinical features, diagnostic methods, and treatment options, as well as nursing management strategies for patient care. The emphasis is on the importance of awareness and education regarding dementia, particularly in the geriatric population.