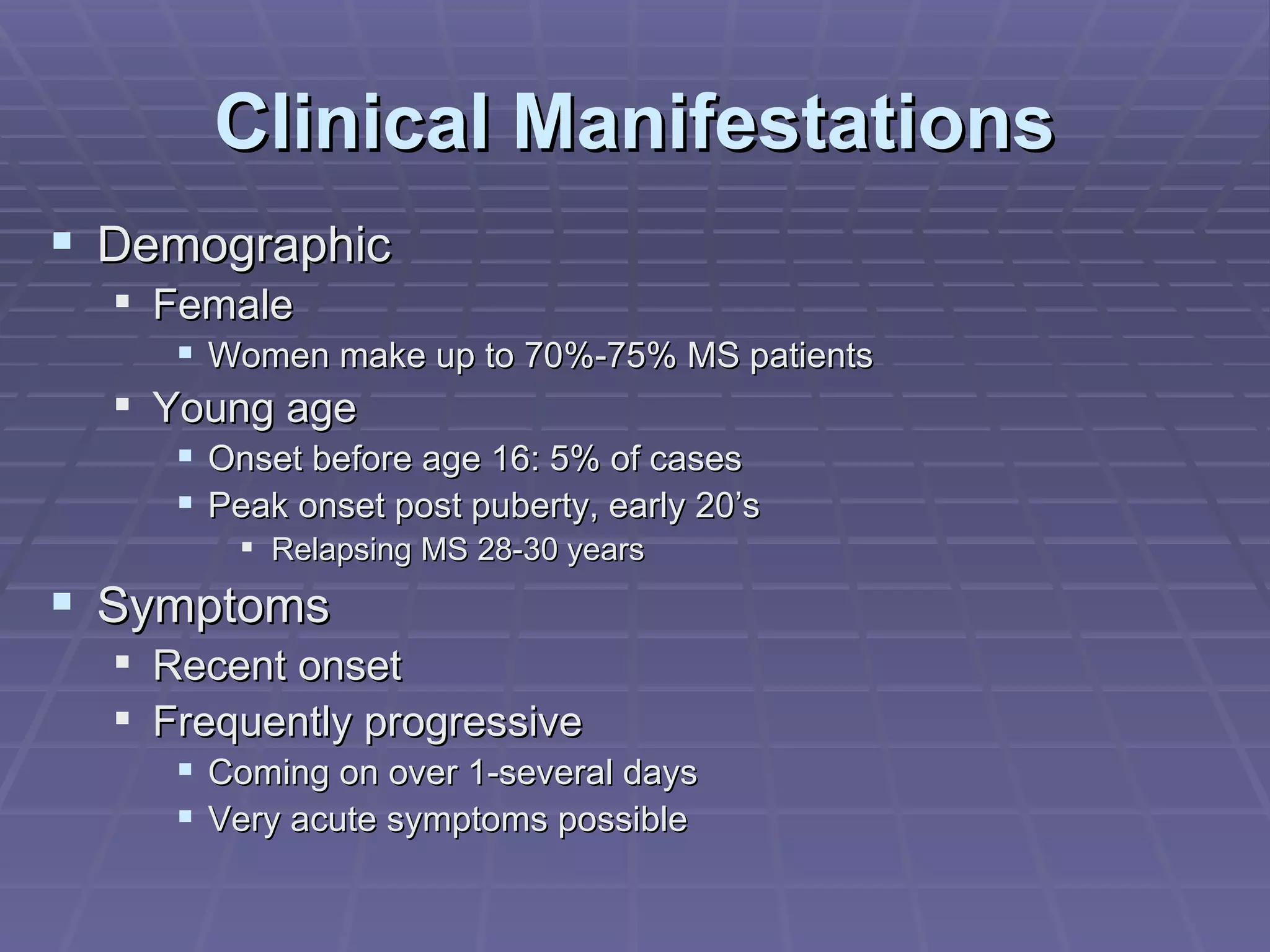
1. Multiple Sclerosis (MS) is a disease of the central nervous system that results in demyelination and damage to the protective covering of nerve fibers. It commonly causes visual issues, weakness, sensory problems, and other neurological symptoms.
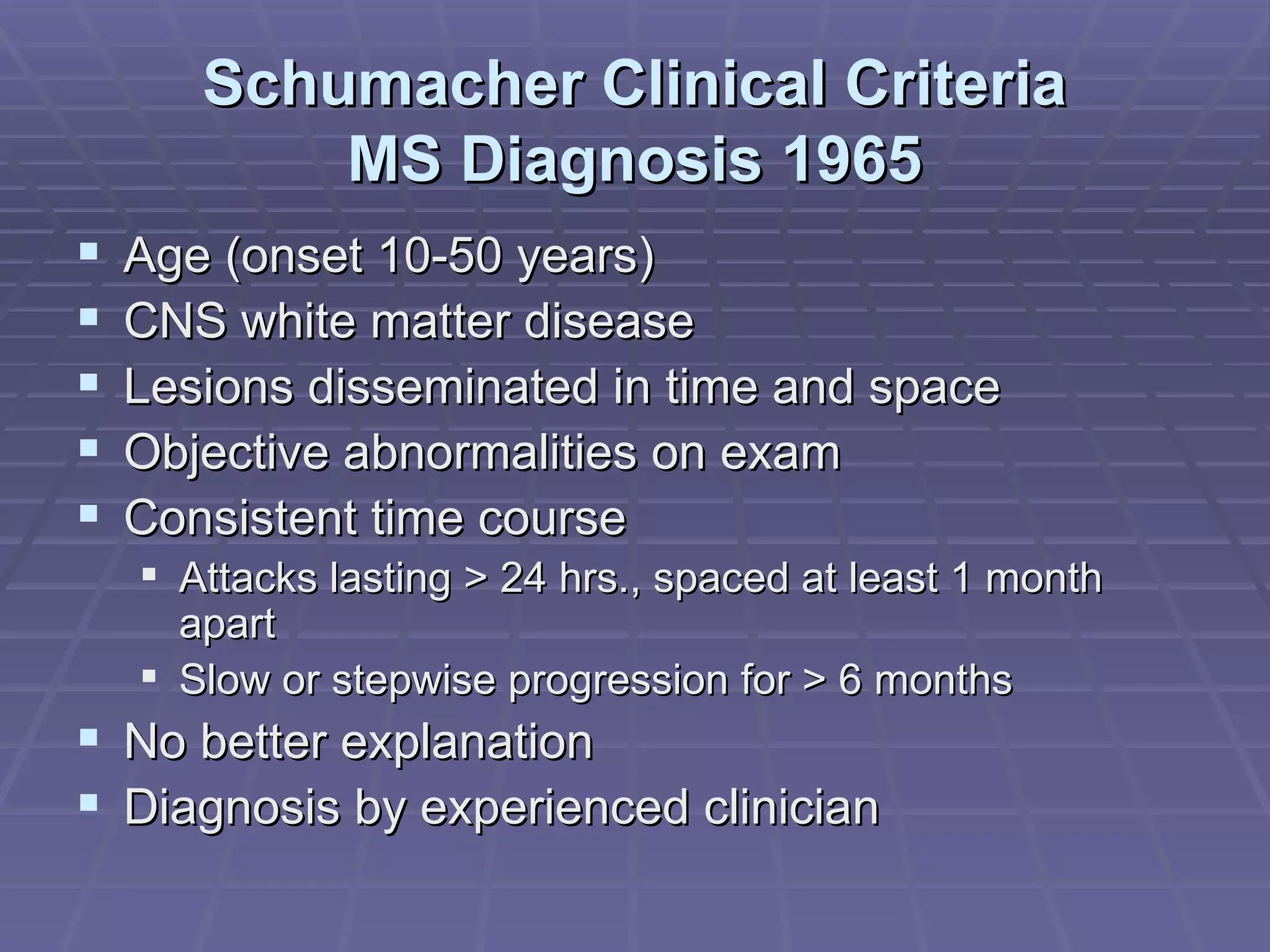
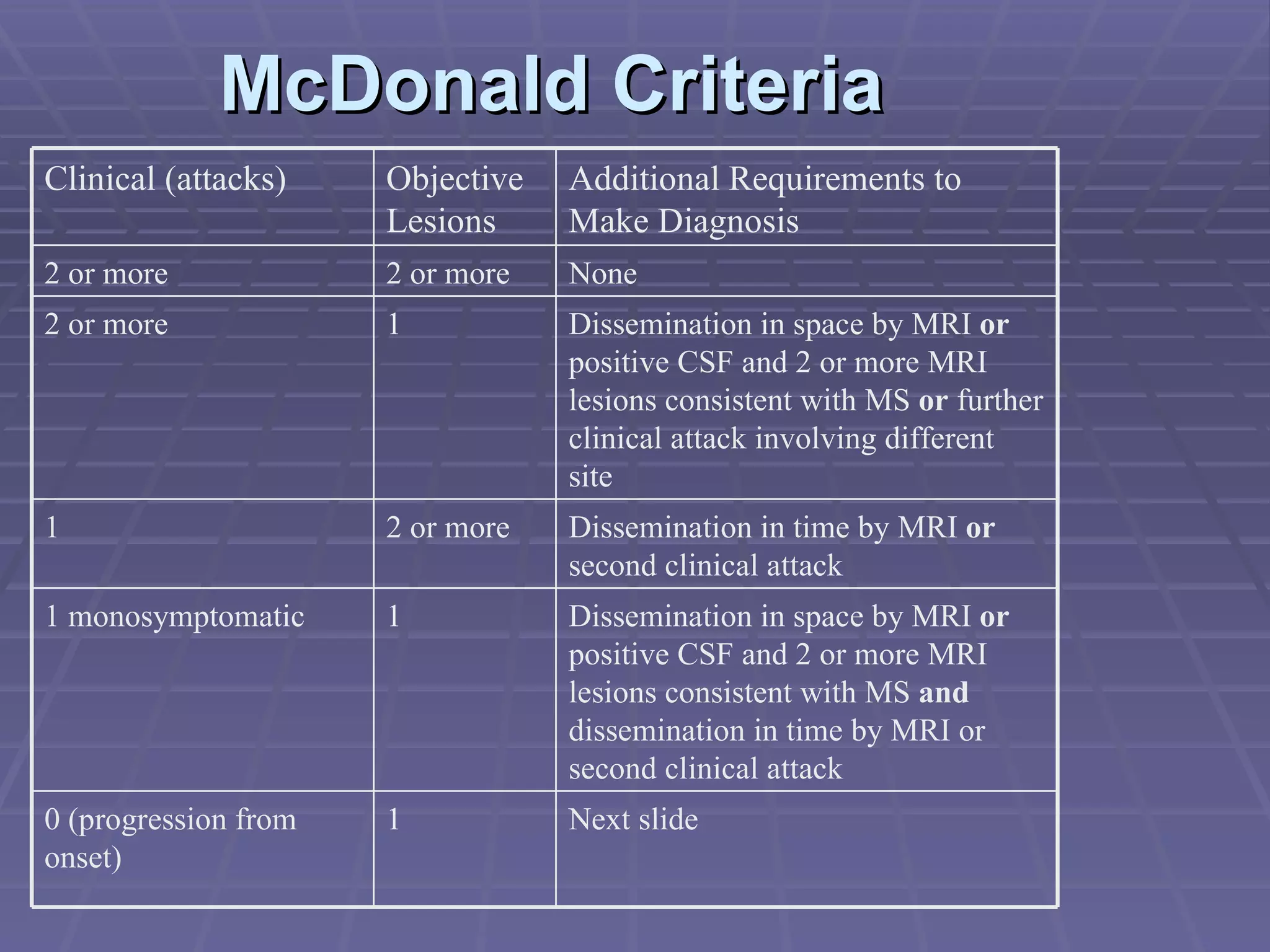
2. The diagnosis of MS involves demonstrating dissemination of lesions in both time and space, either clinically or radiologically. The McDonald criteria from 2001 provides guidelines for diagnosing MS based on clinical attacks, MRI findings, and cerebrospinal fluid analysis.
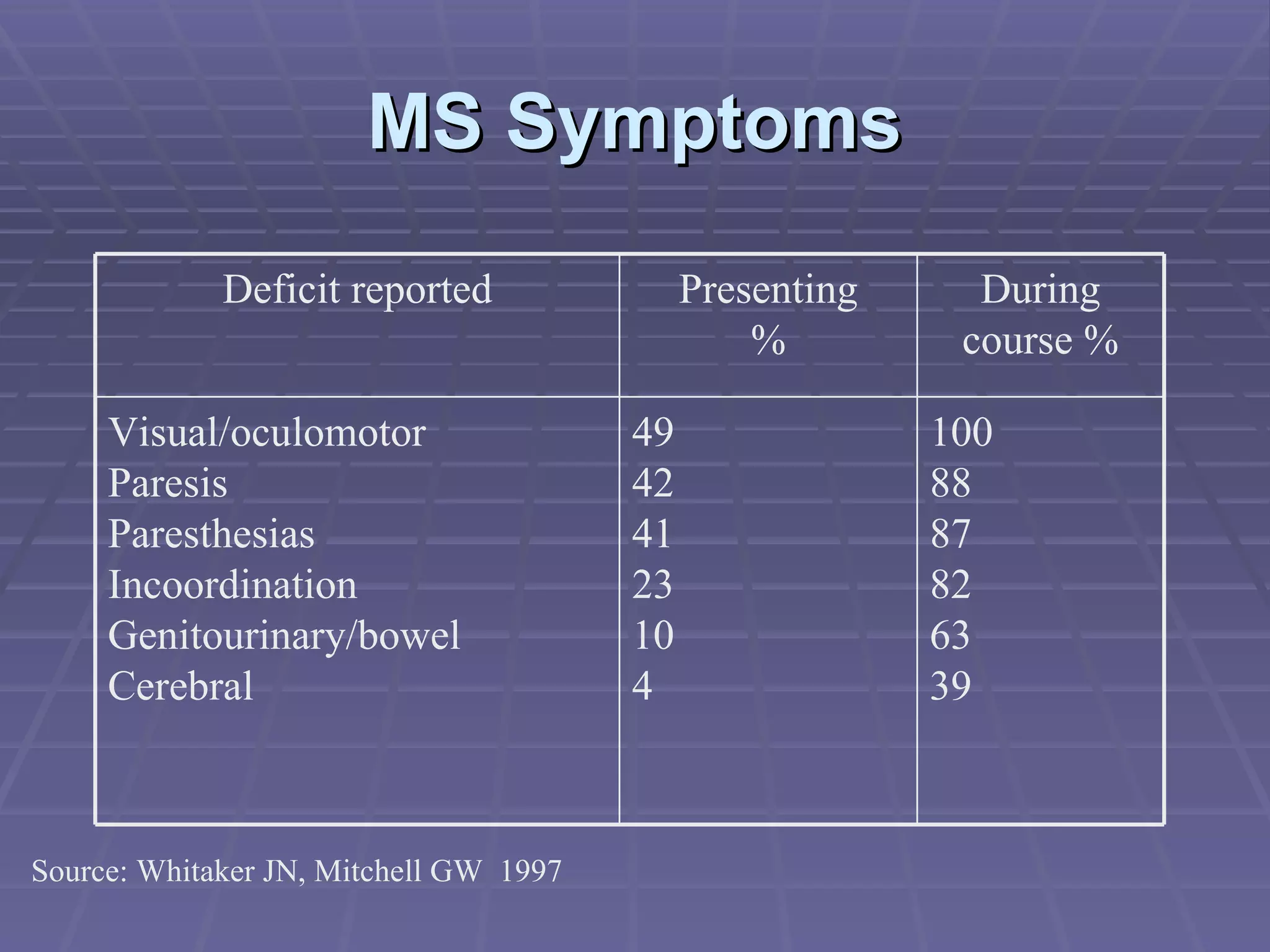
3. Common symptoms of MS include visual problems, motor weakness, sensory issues like numbness and tingling, and bladder/bowel dysfunction. Symptoms vary depending on location of lesions in the brain and spinal