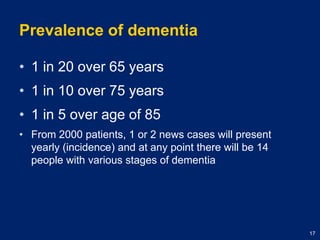
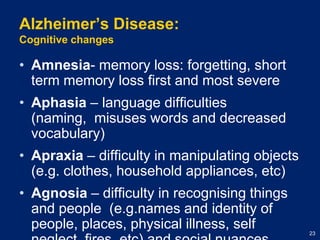
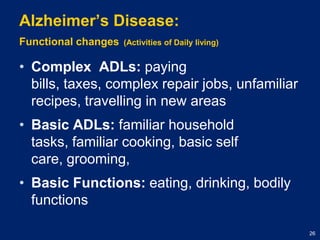
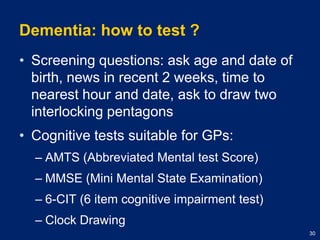
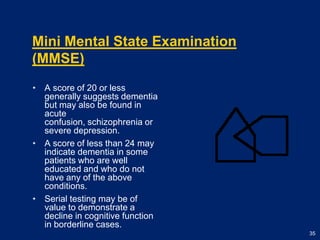
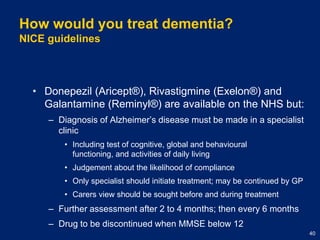
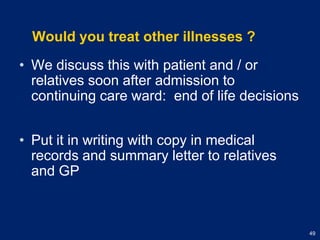
The document discusses dementia and primary care. It notes that the general practitioner (GP) is usually the first place people go if worried about dementia, so early detection by the GP is important. It provides information on diagnosing and treating dementia, including guidelines on prescribing medications. It also addresses dealing with behavioral issues like aggression, treating other illnesses, end of life decisions, and the ethics of caring for elderly demented patients in primary care.