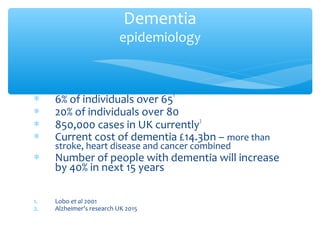
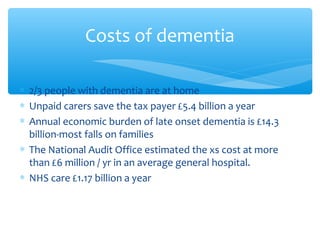
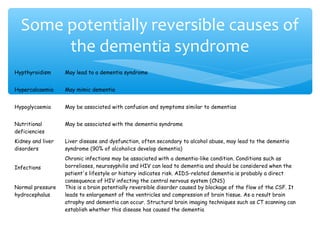
This document provides an overview of dementia and its treatment. It discusses the scope of dementia as a health problem, describing key statistics on prevalence and costs. It defines dementia and covers early diagnosis, treatment options, and behavioral symptoms. The presentation outlines the main types of dementia, including Alzheimer's disease, vascular dementia, and Lewy body dementia. It discusses diagnosis, risk factors, pathogenesis, and management of behavioral symptoms with antipsychotics. The future of dementia care is also mentioned.