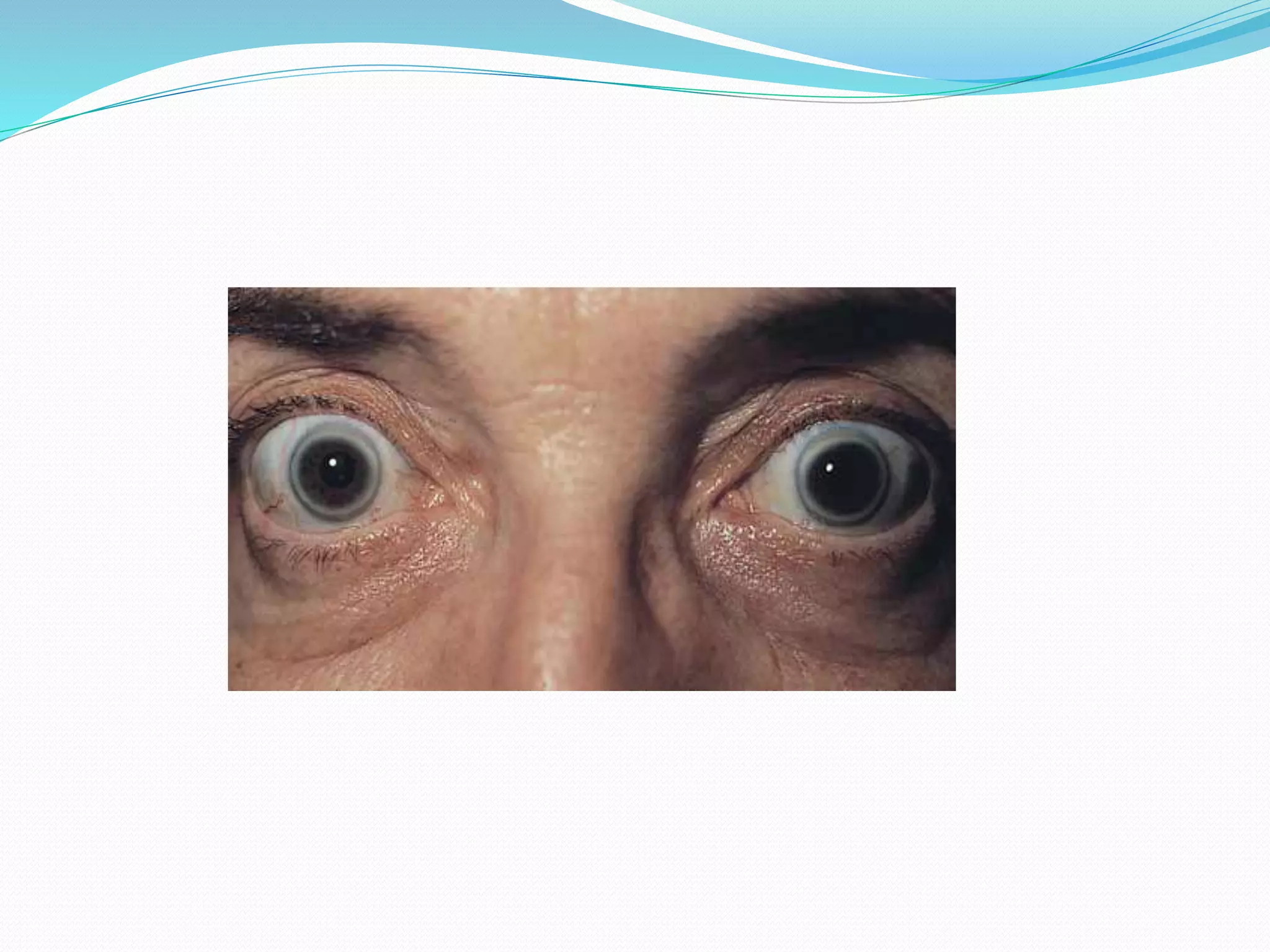
This document summarizes various degenerative conditions of the conjunctiva, cornea, and retina. It describes conditions such as pterygium, pinguecula, and concretions of the conjunctiva. For the cornea, it discusses recurrent erosion, arcus senilis, and lipid keratopathy. Regarding the retina, it outlines microcystoid degeneration, retinoschisis, and paving stone degeneration. The document provides details on the signs, symptoms, etiology, and treatment of these various ocular degenerative diseases.