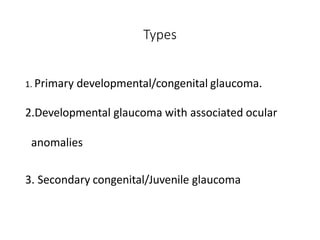
This document discusses congenital glaucoma, including its definition, pathogenesis, clinical presentation, diagnosis, differential diagnosis, and treatment. Some key points:
- Congenital glaucoma is caused by abnormal development of the anterior chamber angle resulting in impaired aqueous outflow and raised intraocular pressure in early childhood.
- Clinical signs include enlarged globe, corneal edema, tears in Descemet's membrane, and high intraocular pressure.
- Diagnosis involves measuring IOP, corneal diameter, examining the optic disc and performing gonioscopy to evaluate the anterior chamber angle.
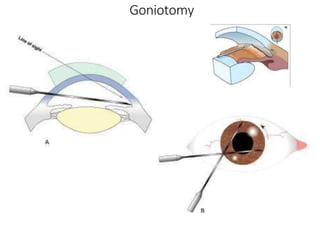
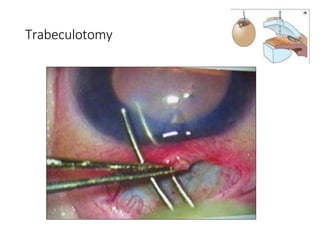
- The primary treatment is surgical to relieve pressure, through procedures like goniotomy or trabeculotomy. Medical treatment is temporary.





![Signs:
• Enlargement of the globe (buphthalmos) is a result of elevated
intraocular pressure.
• Bluish discoloration patches over sclera
[due to thinning of sclera underlying uveal tissue becomes visible]
Clinical Presentation](https://image.slidesharecdn.com/congeitalglaucoma-230826123142-b33c03a3/85/congeital_glaucoma-pptx-9-320.jpg)