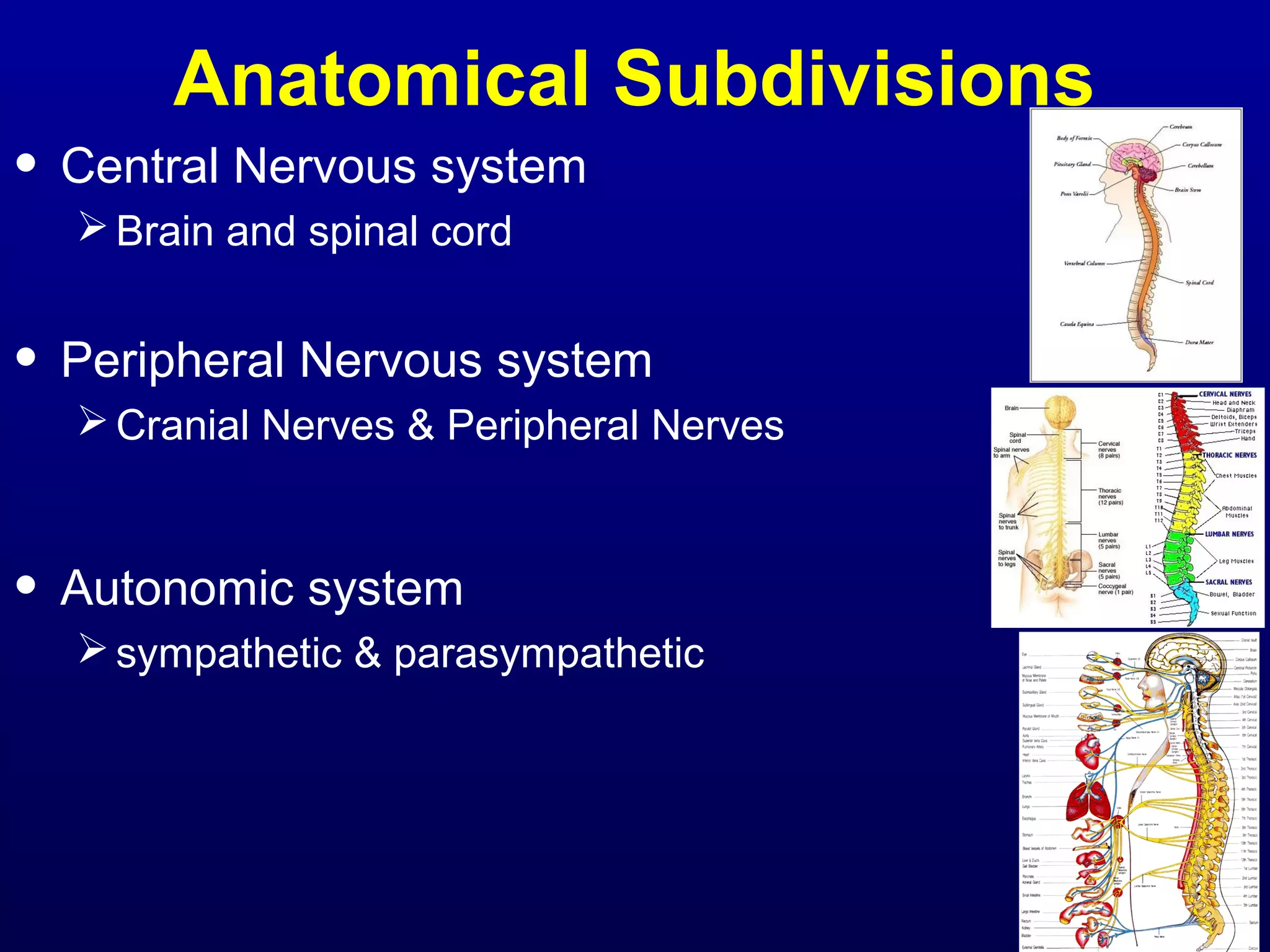
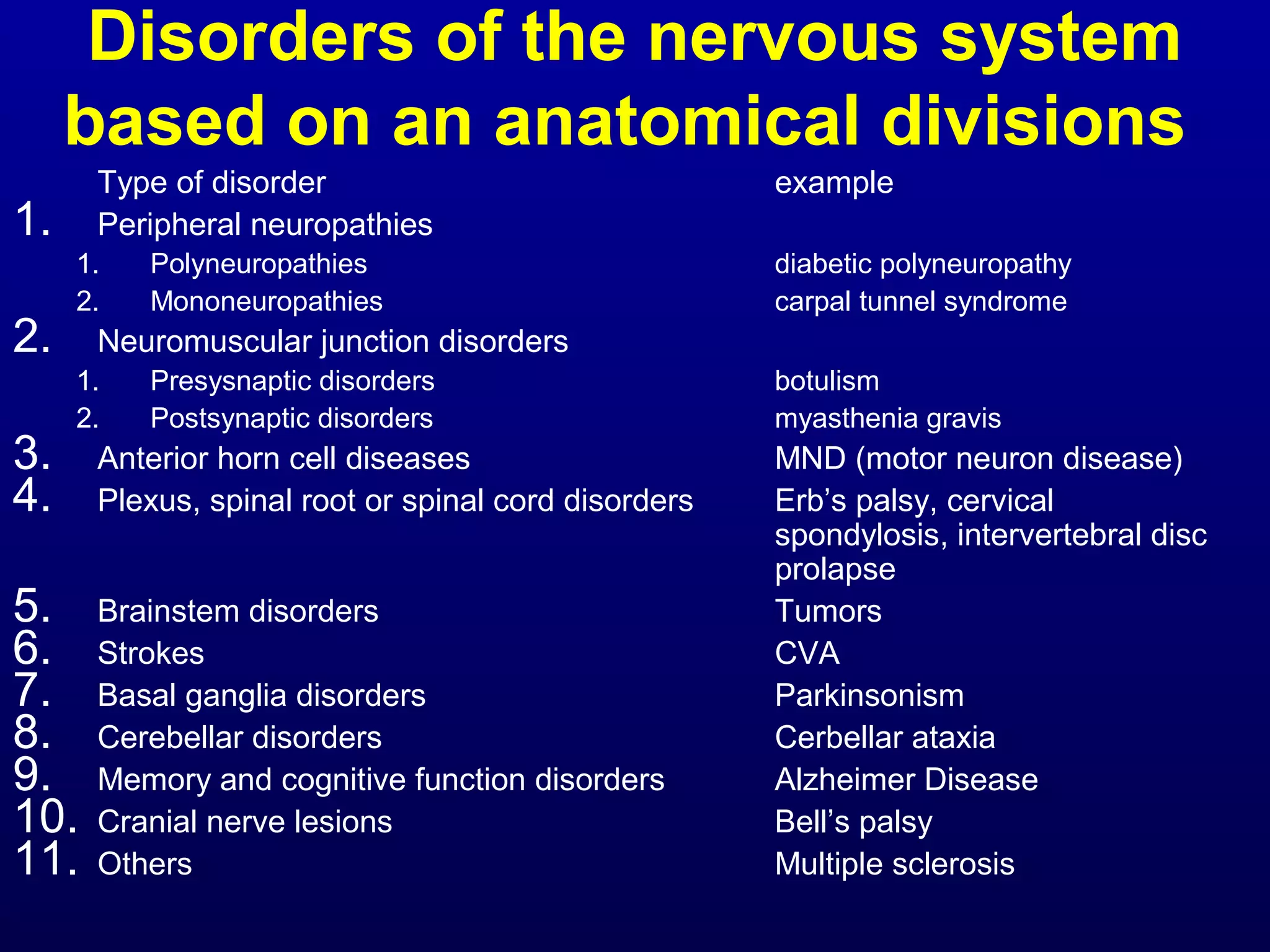
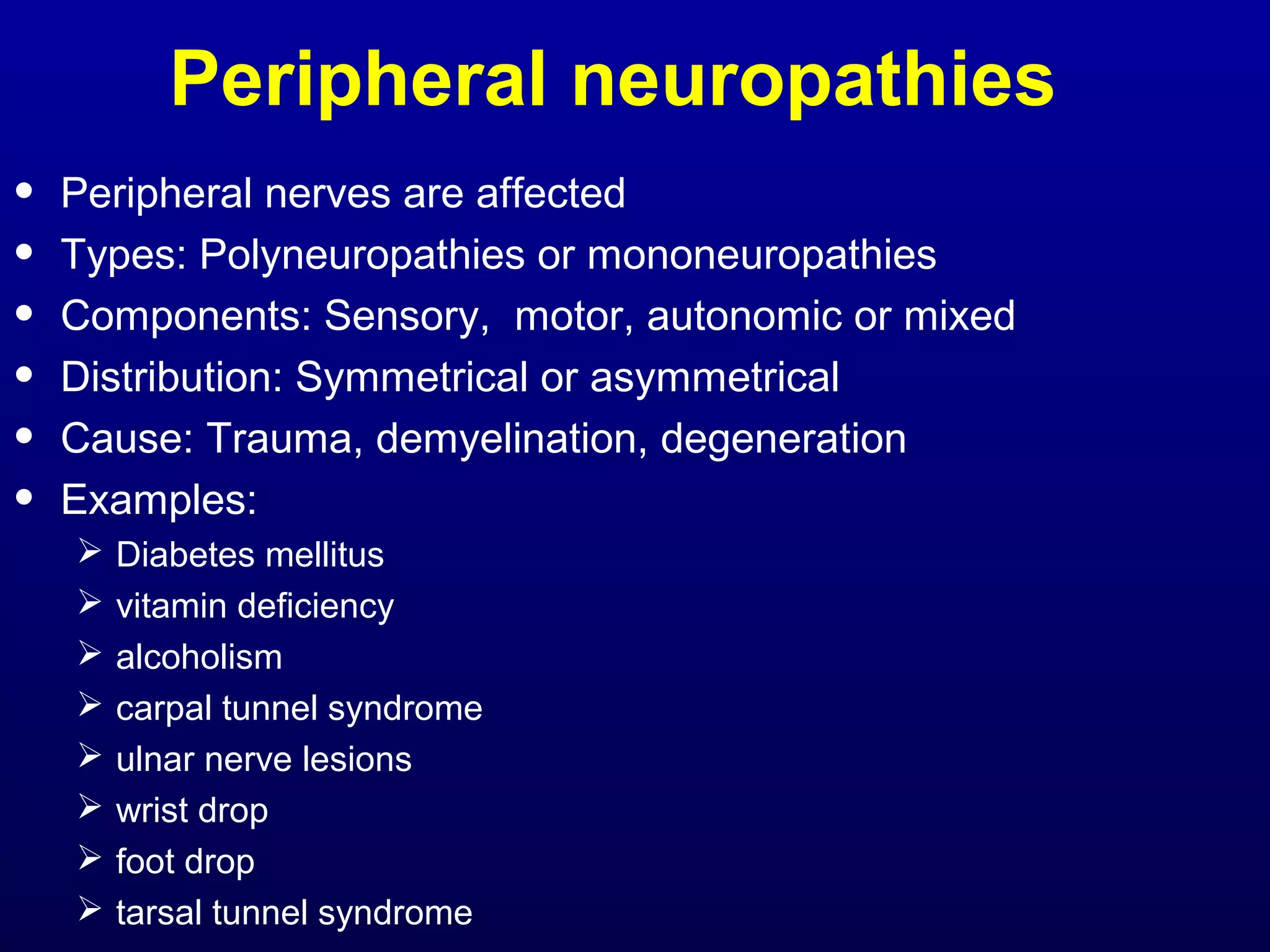
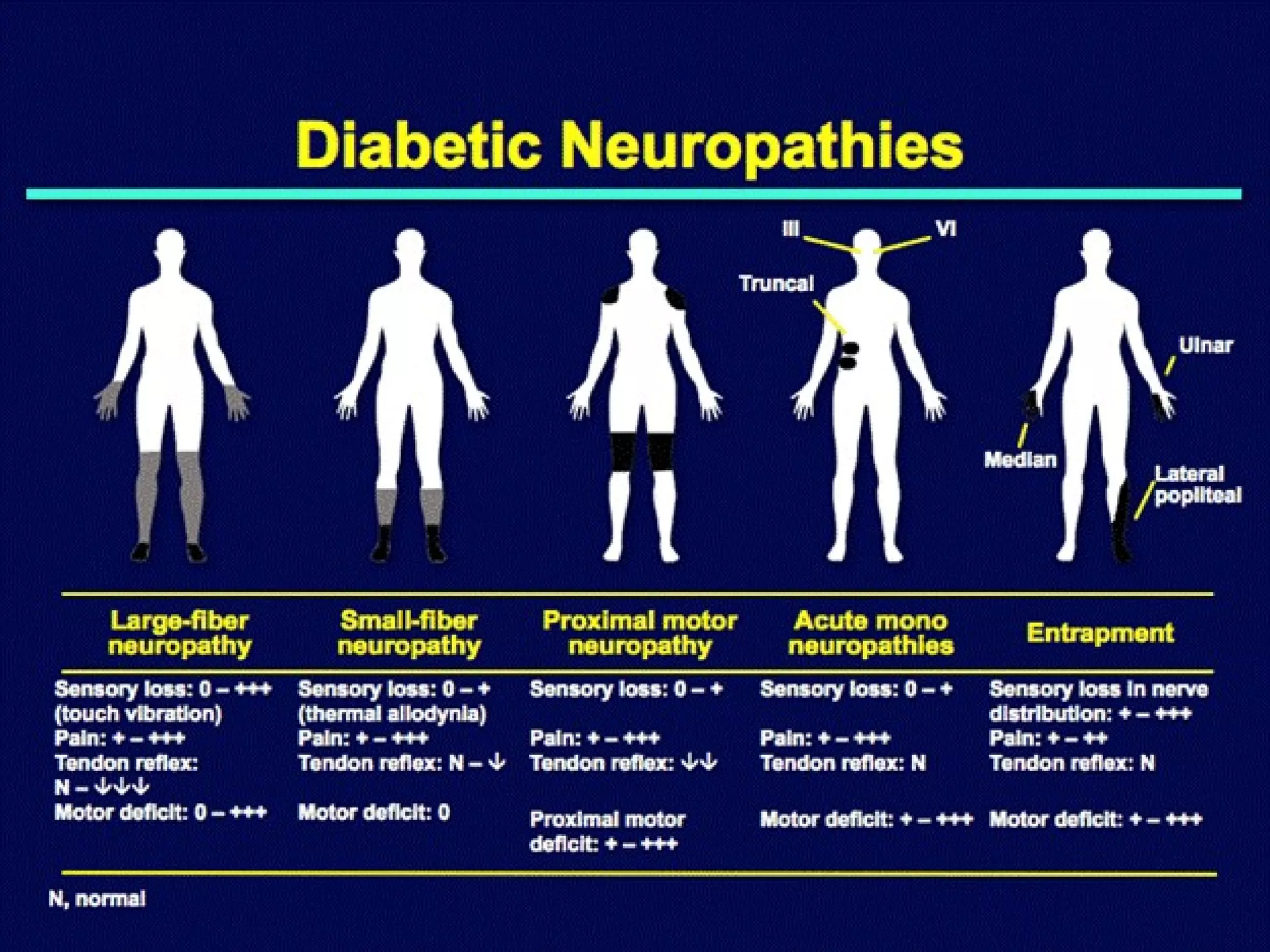
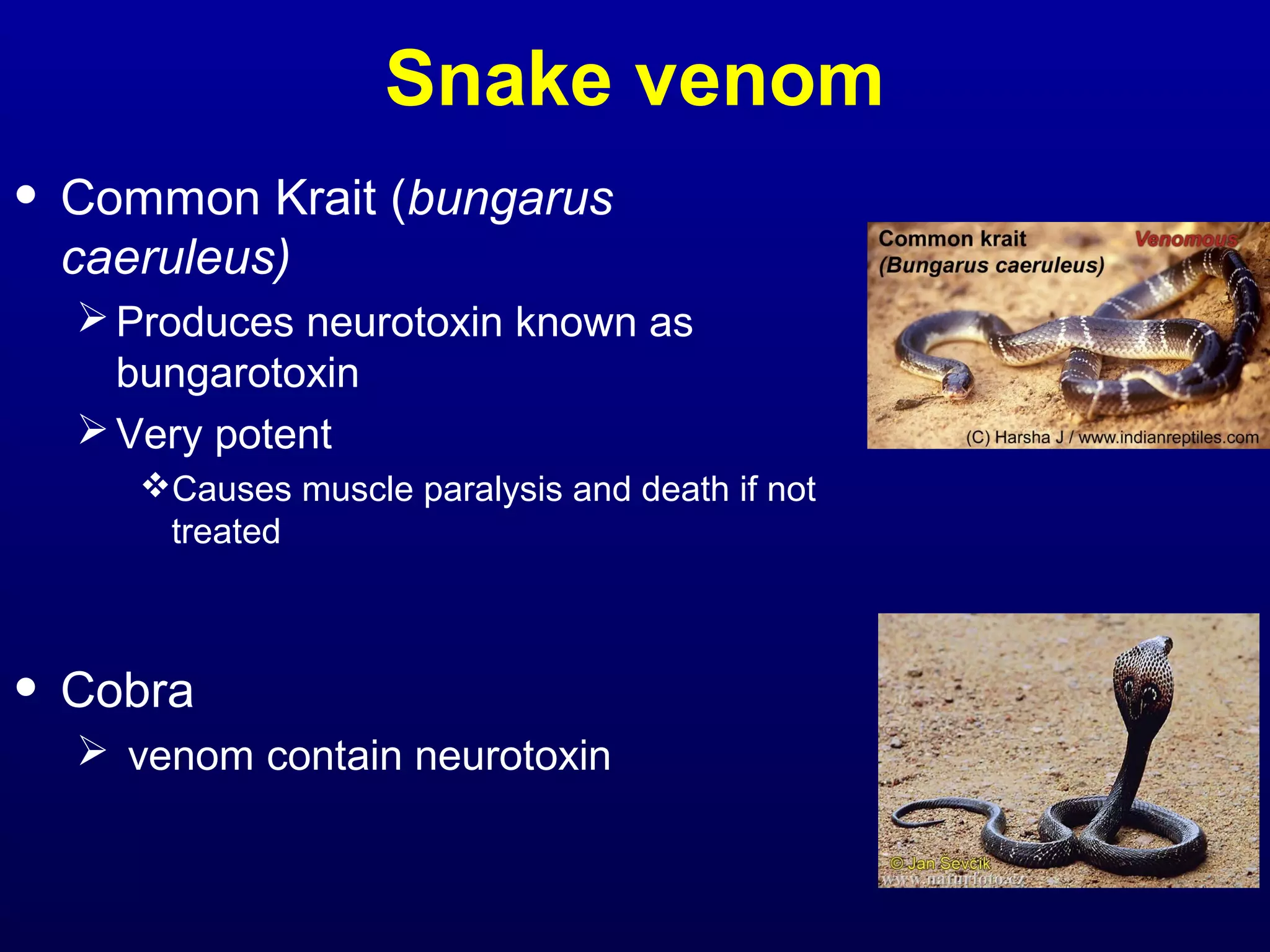
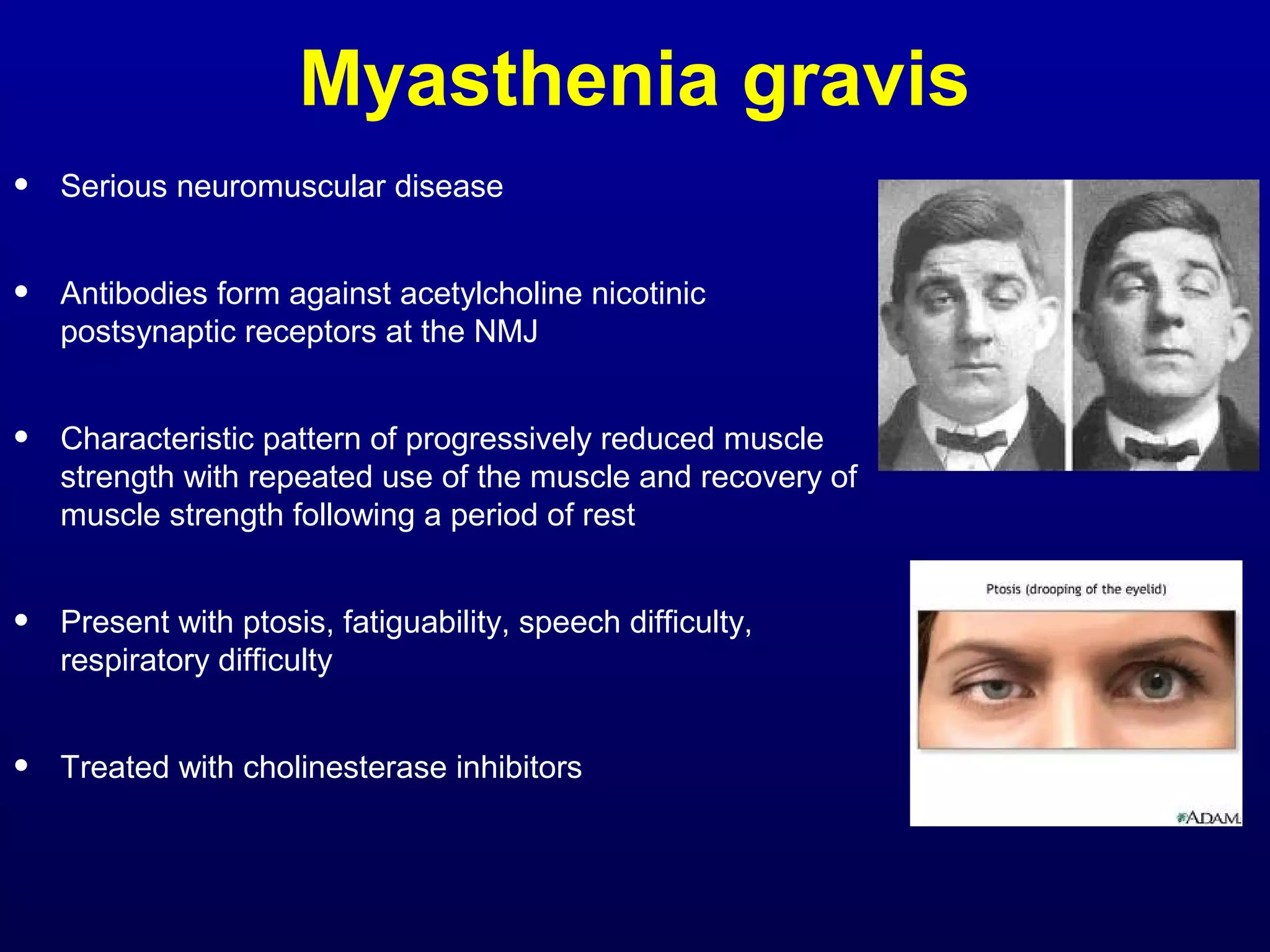
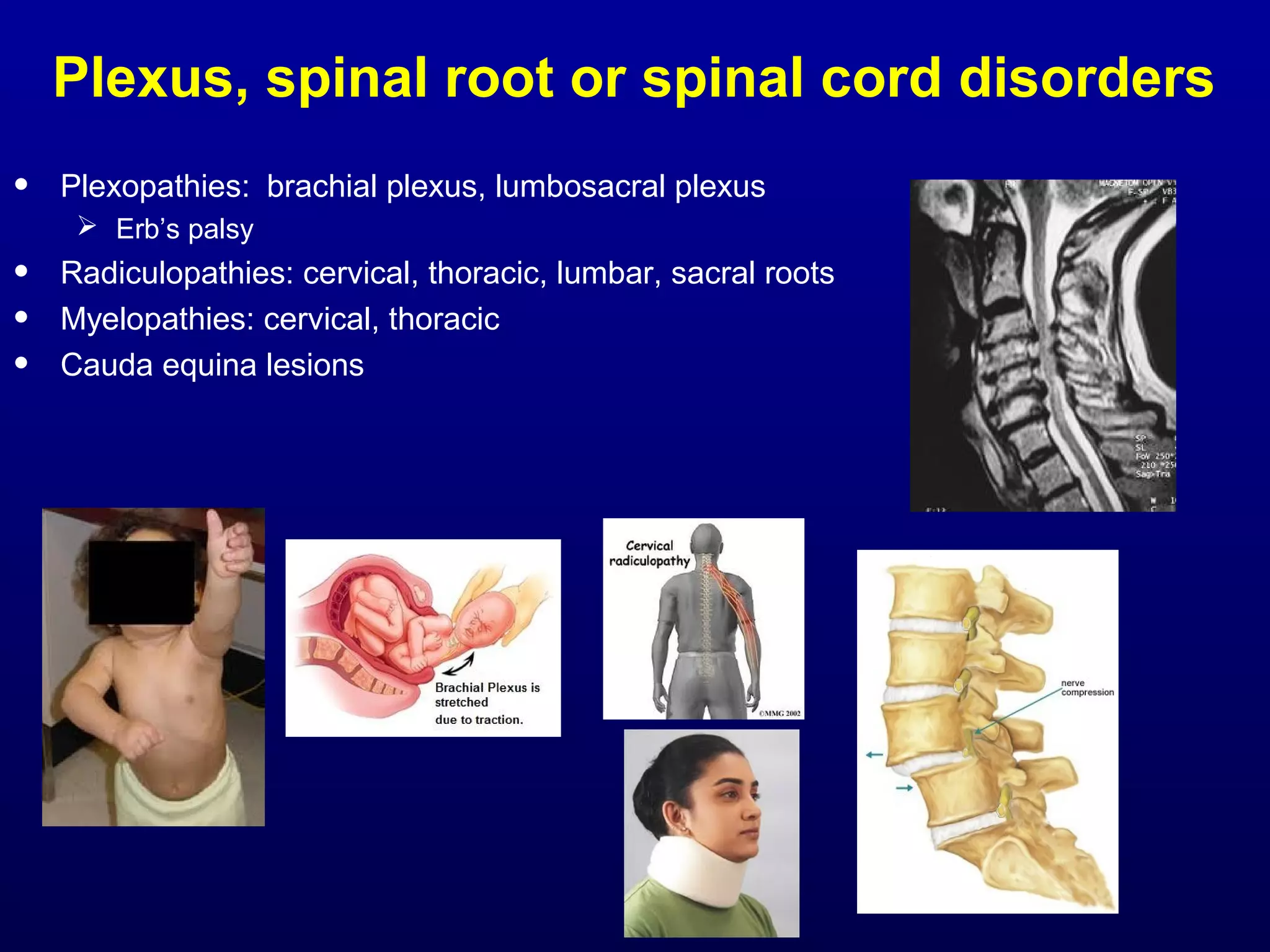
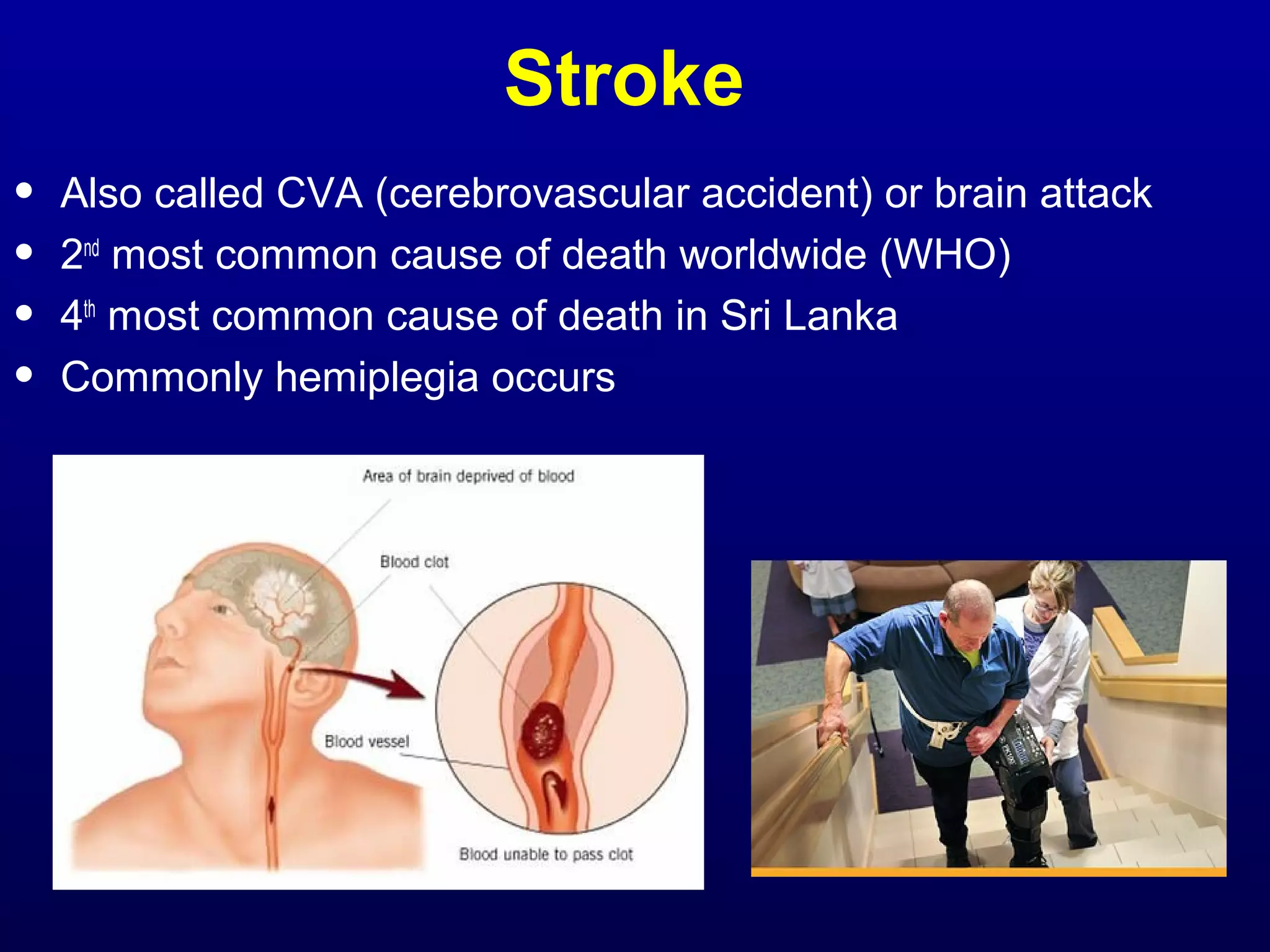
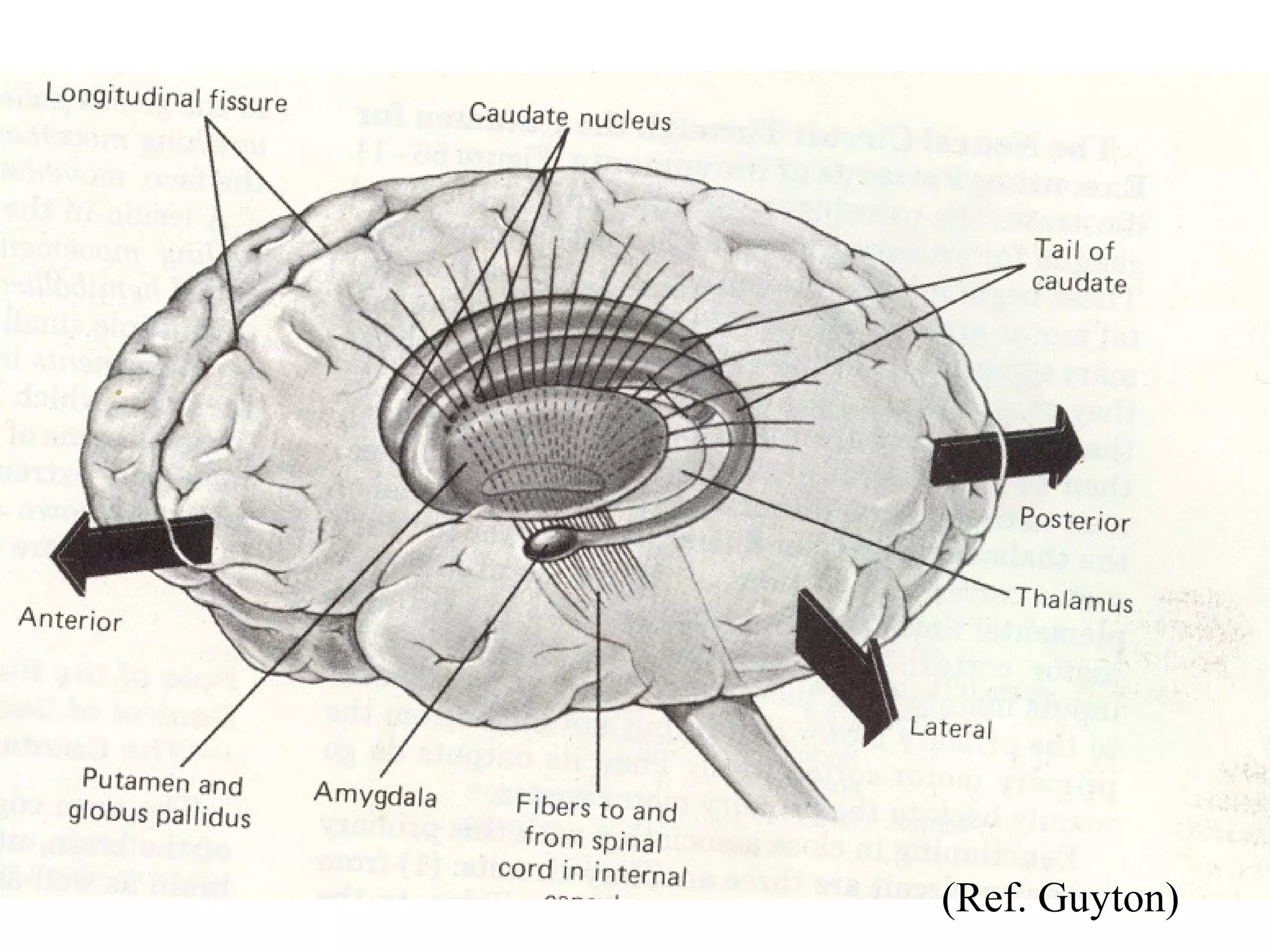
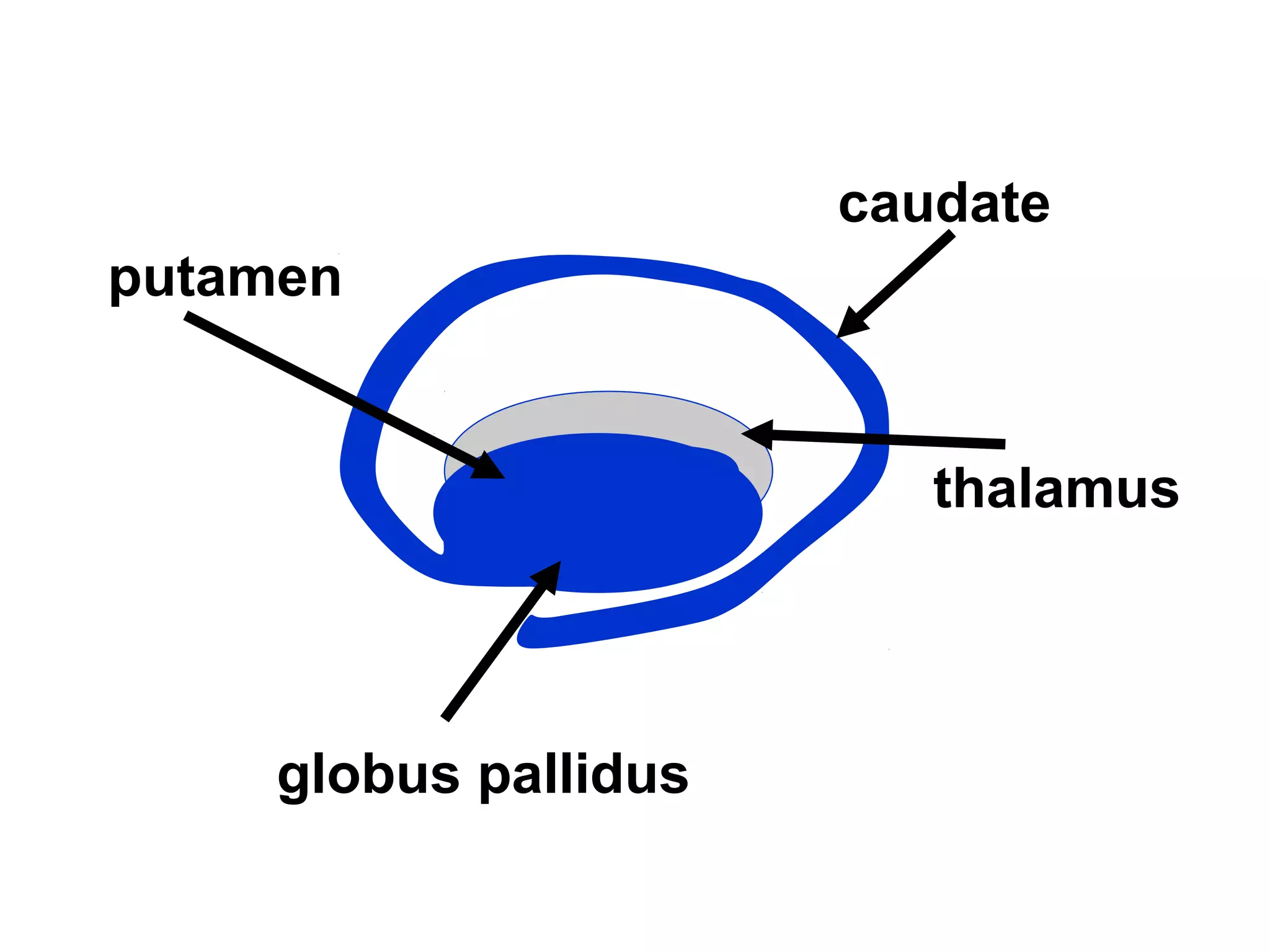
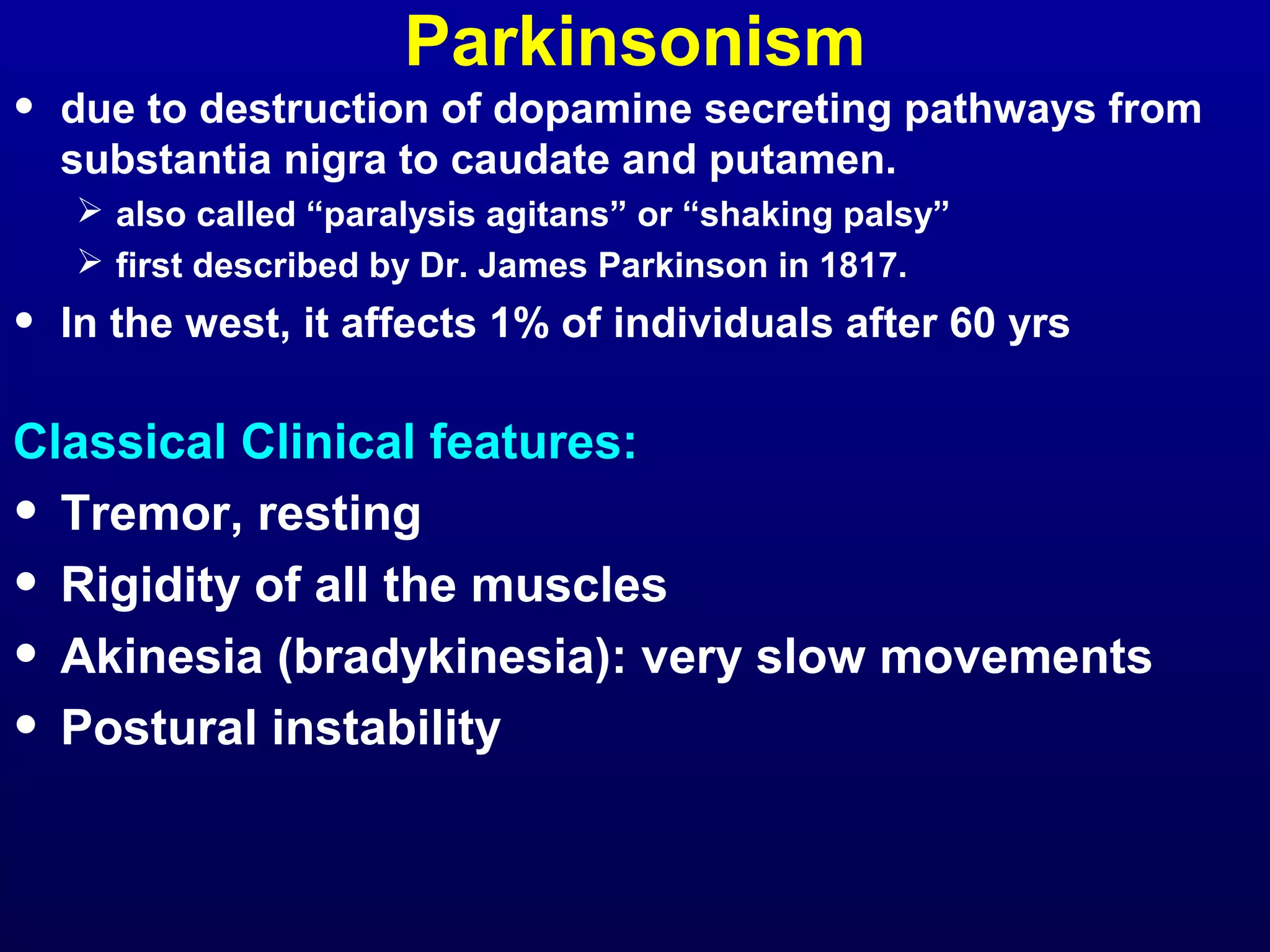
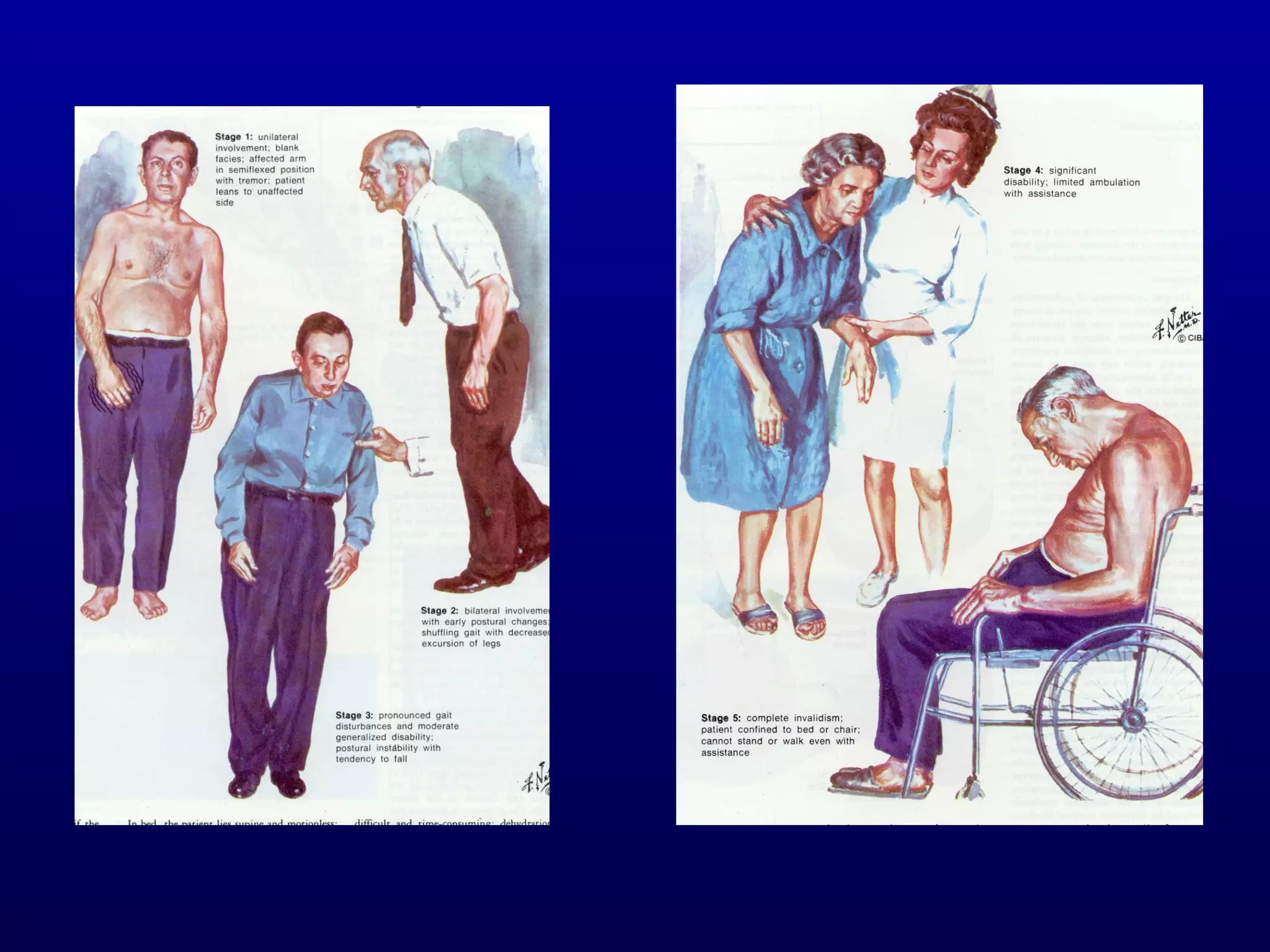
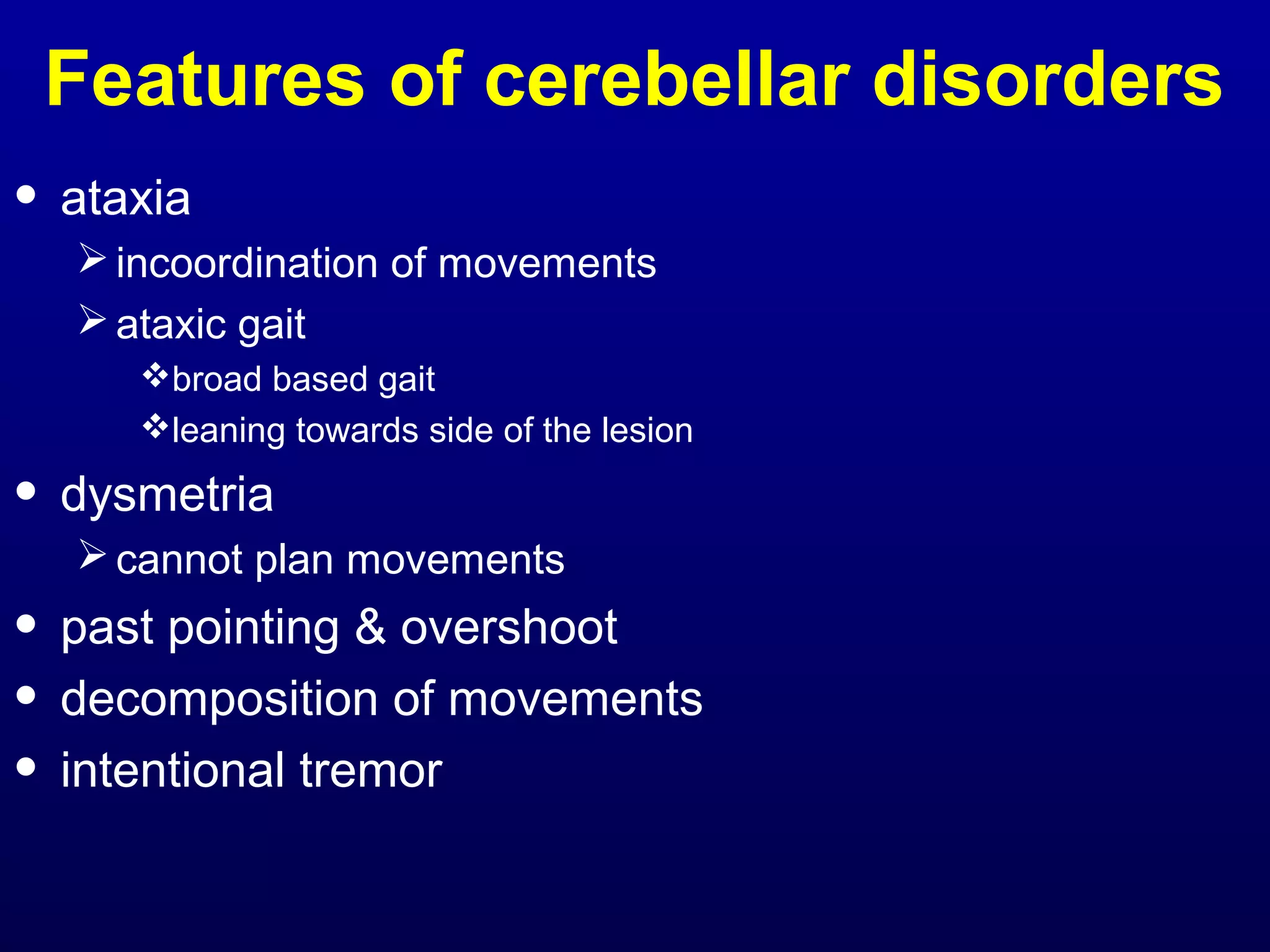
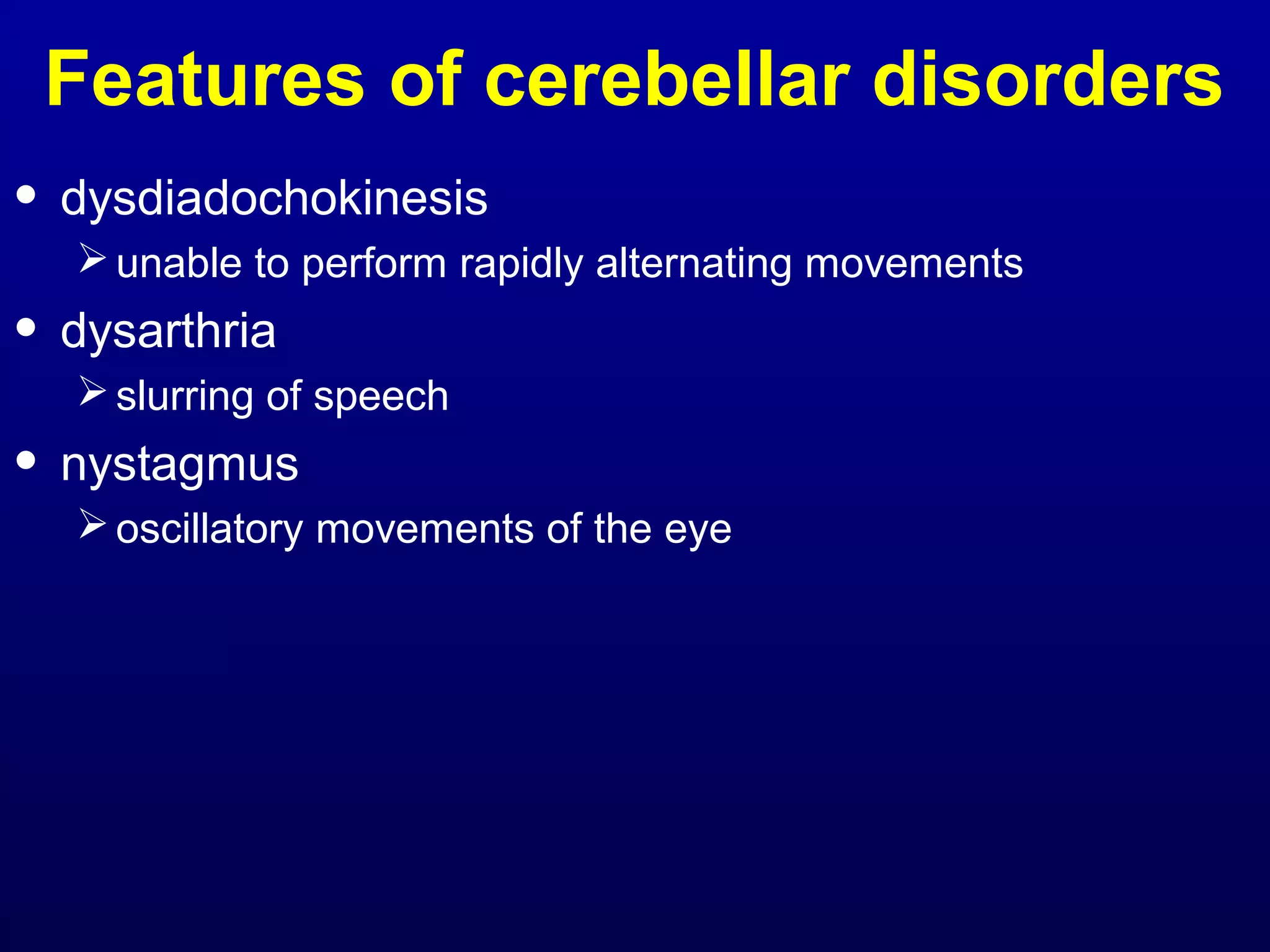
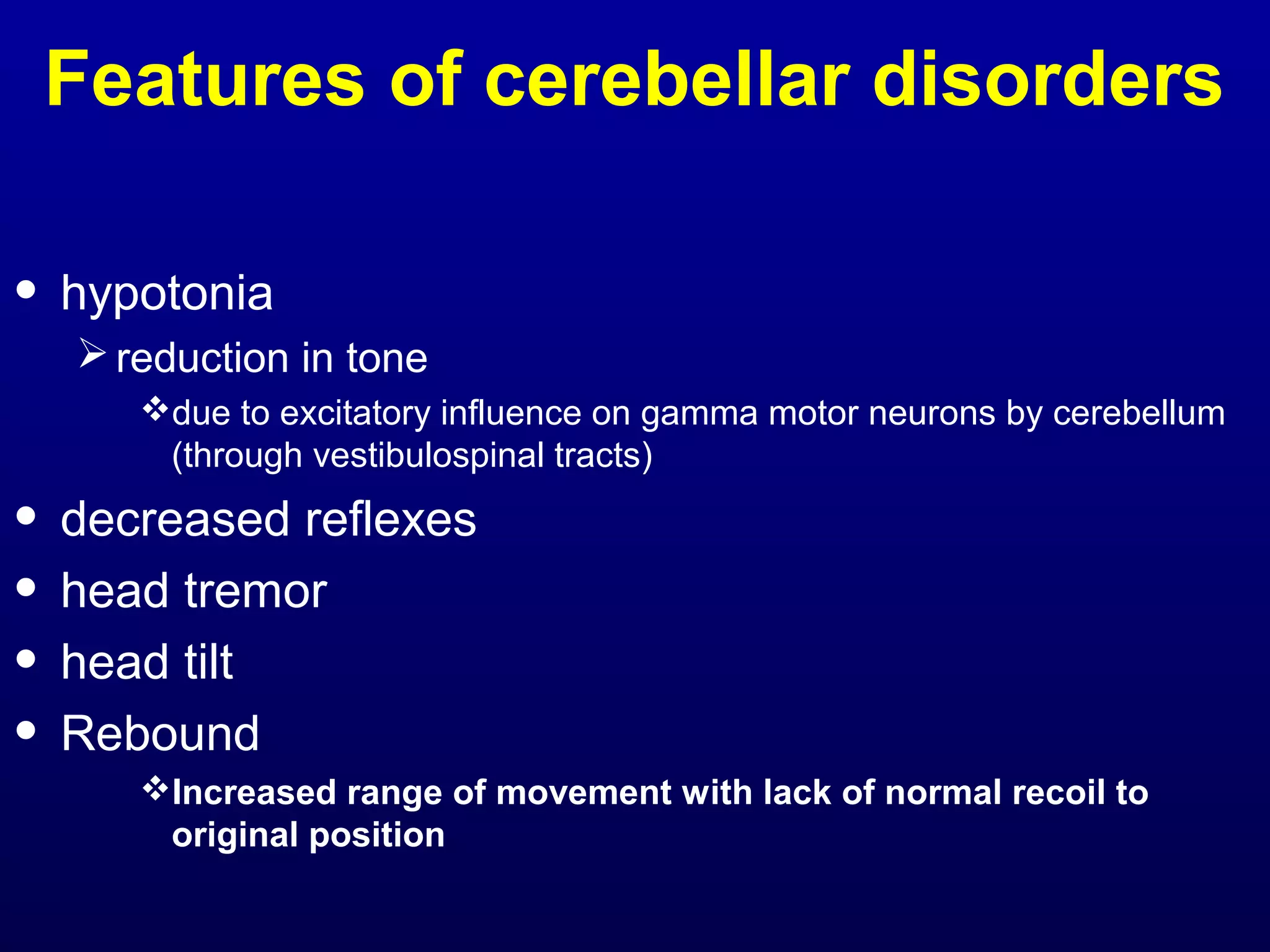
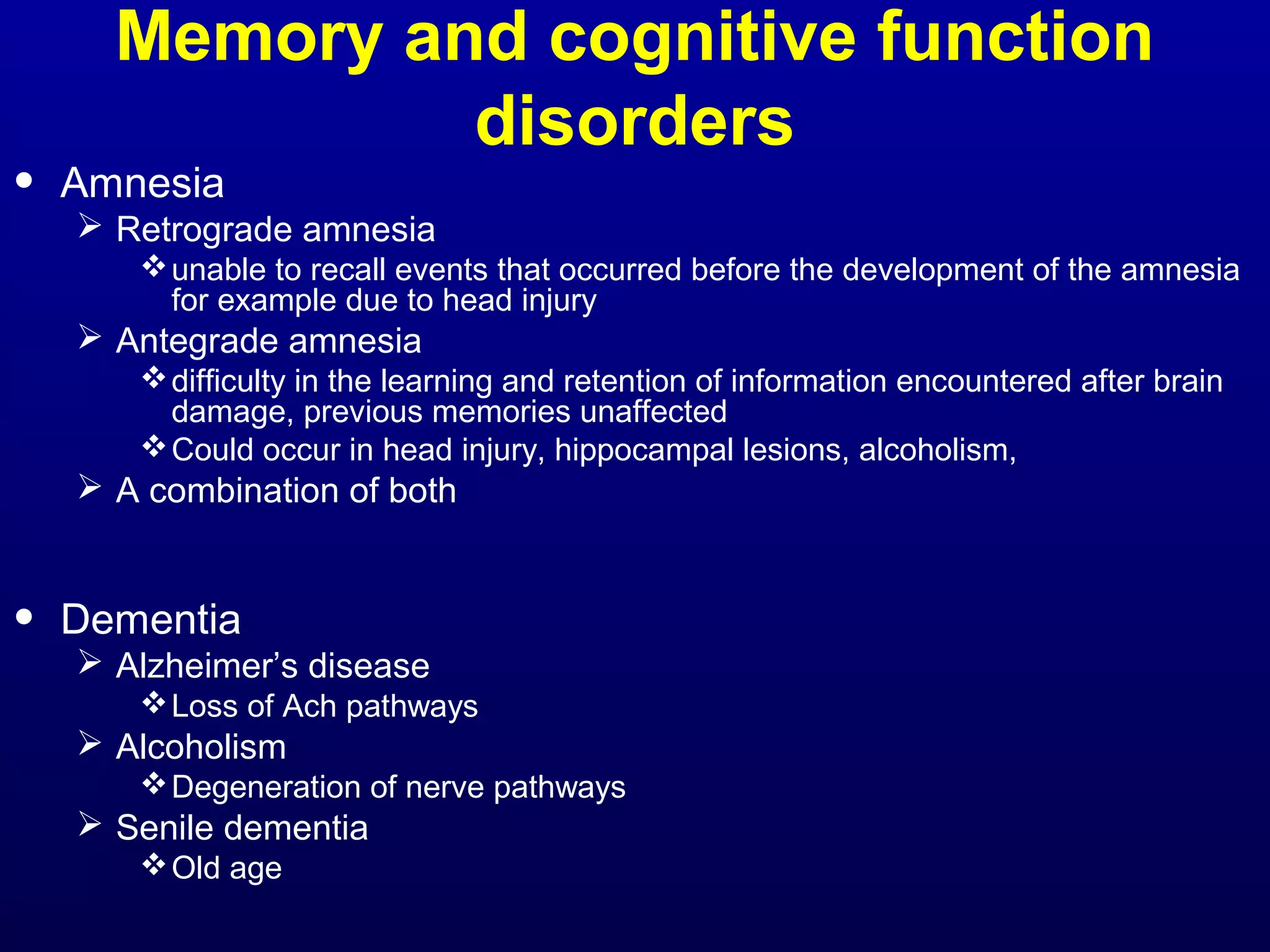
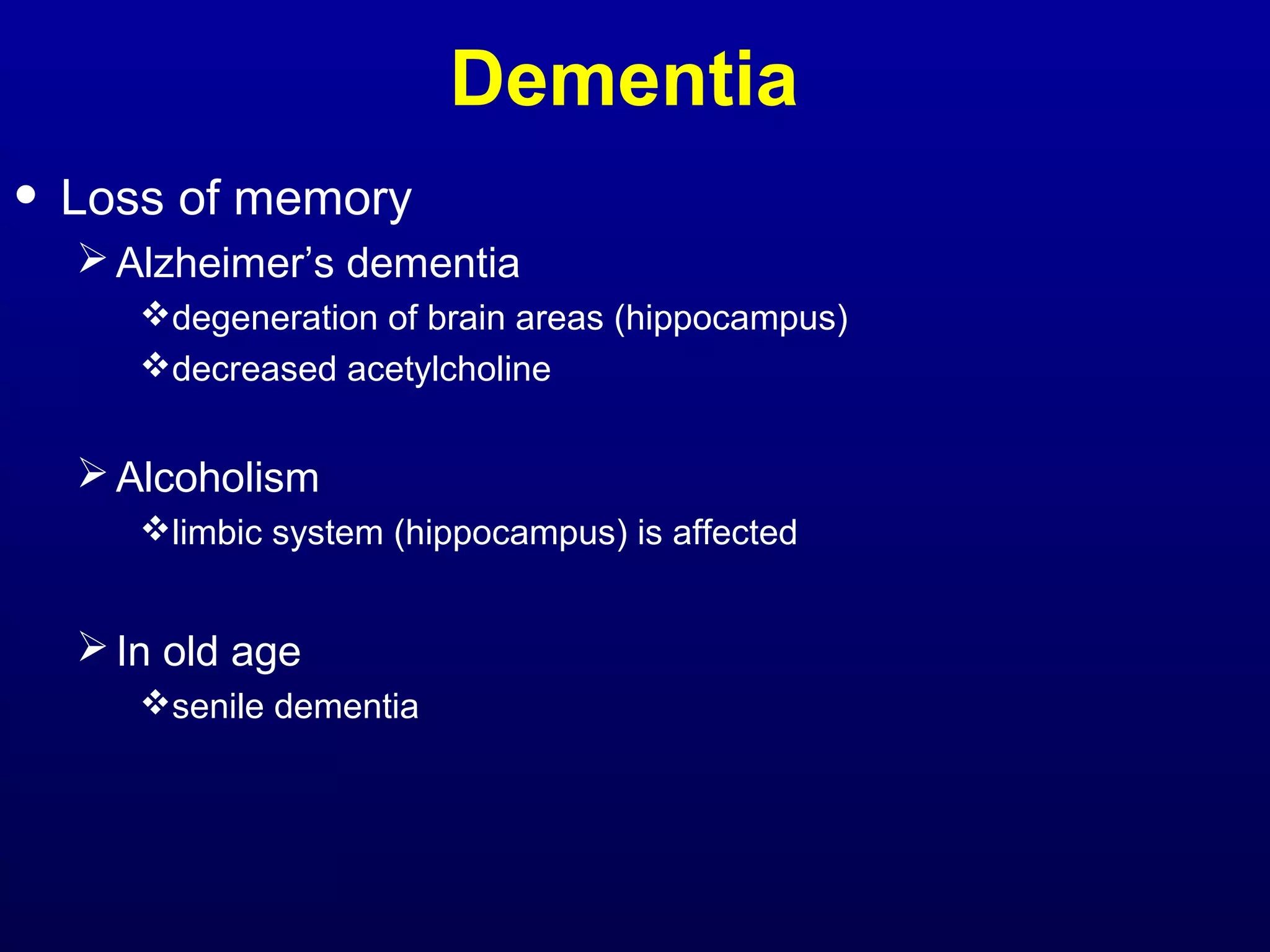
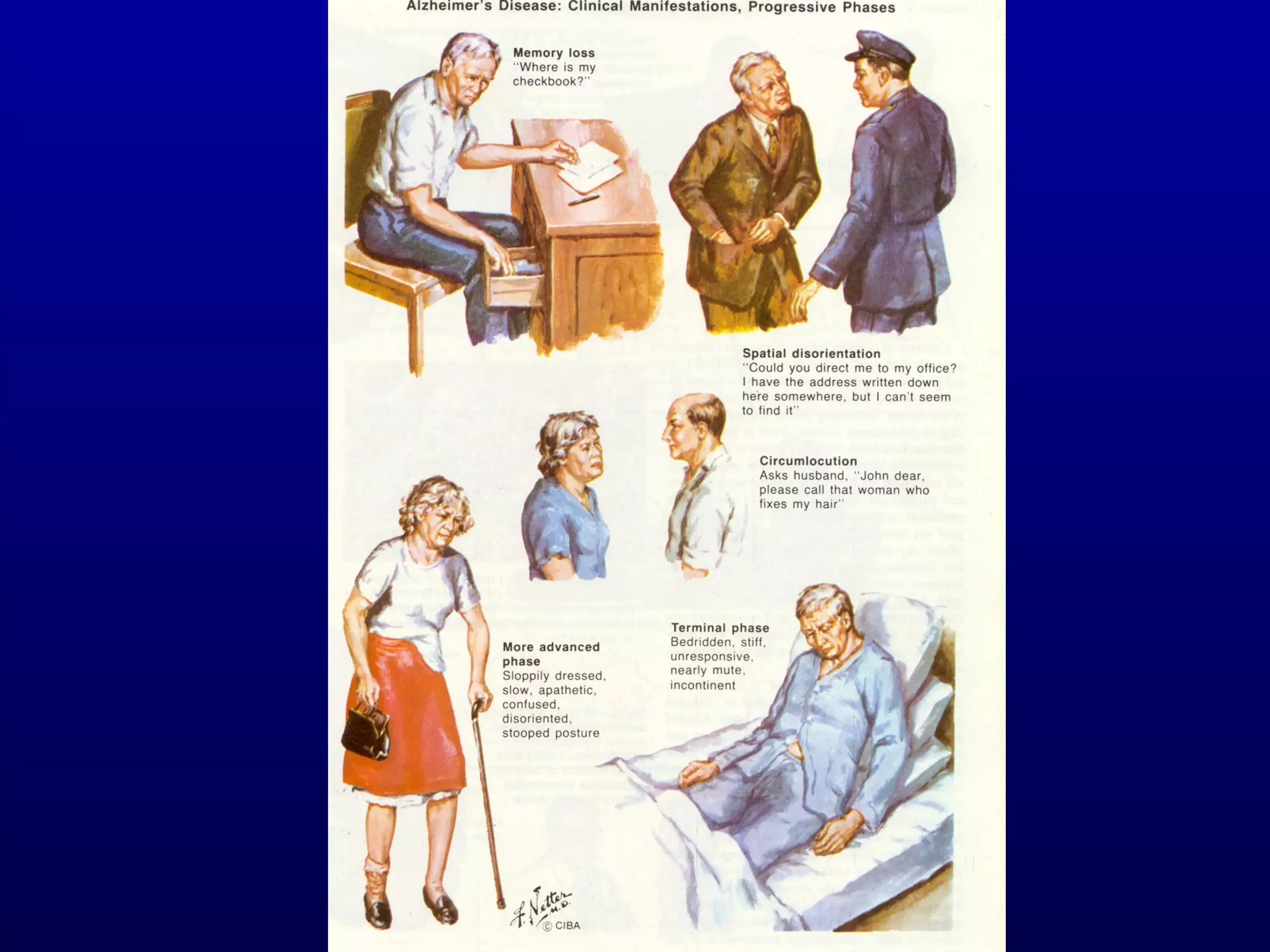
This document provides an overview of clinical neuroanatomy and disorders of the nervous system. It begins by explaining why the study of the nervous system is important for understanding neurological diseases. It then outlines the functional and anatomical subdivisions of the nervous system. The remainder of the document discusses various neurological disorders categorized by the areas of the nervous system they affect, such as the peripheral nerves, neuromuscular junction, brainstem, basal ganglia, cerebellum, and memory/cognition. Examples of specific diseases are provided for each category.