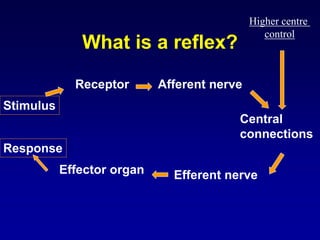
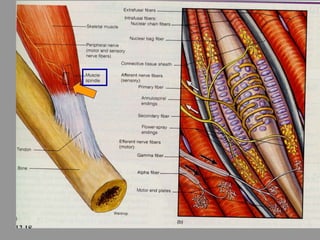
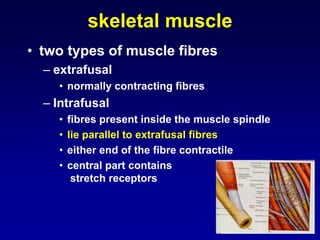
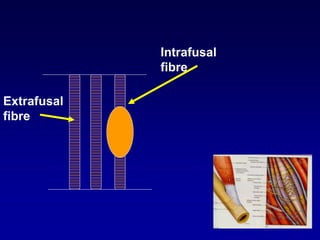
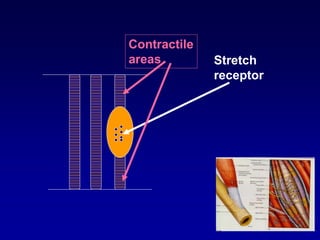
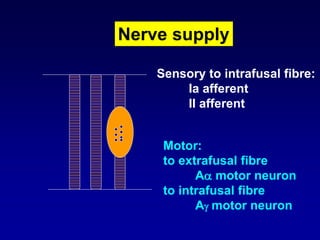
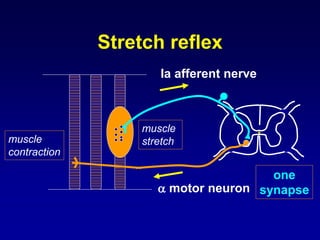
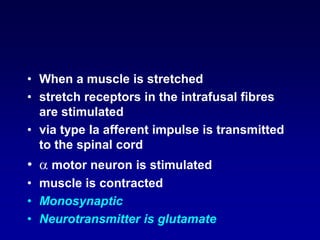
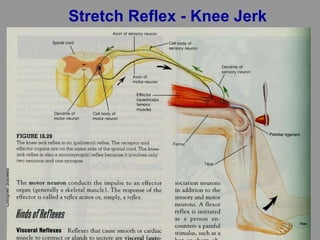
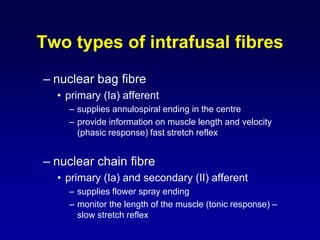
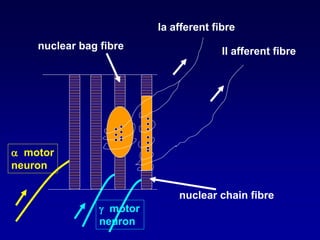
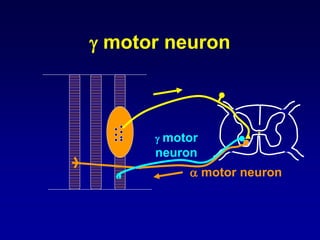
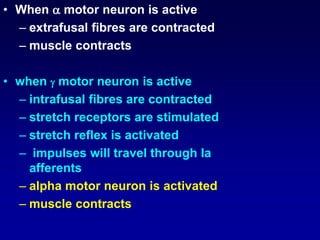
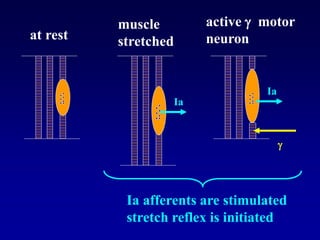
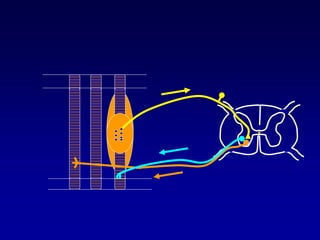
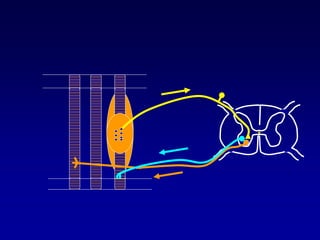
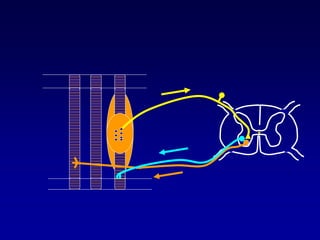
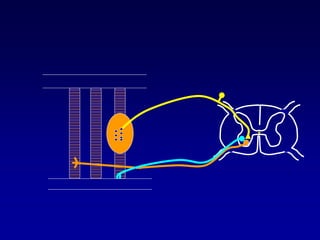
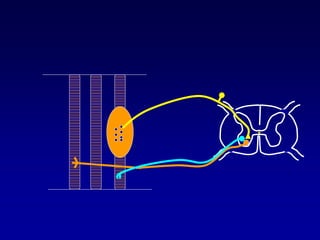
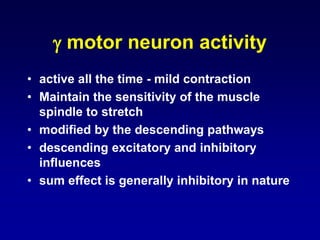
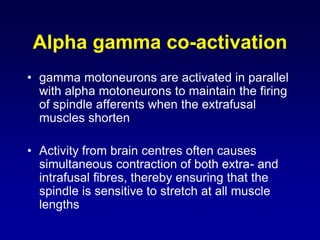
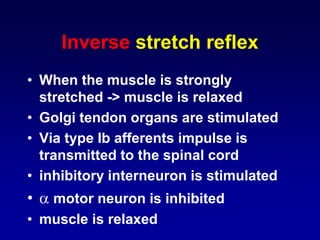
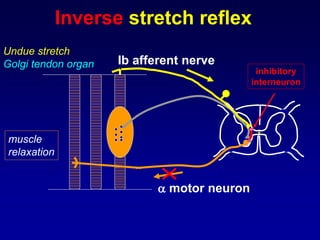
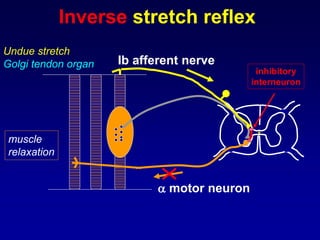
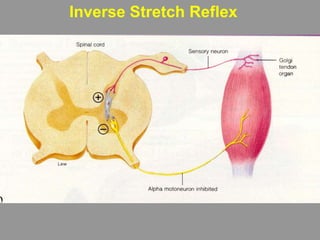
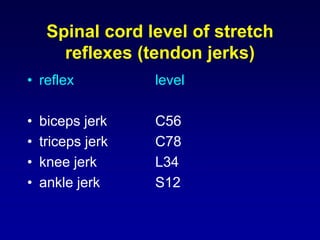
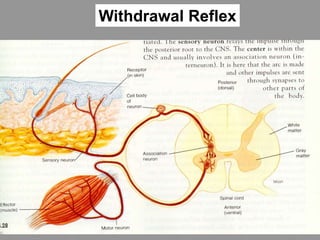
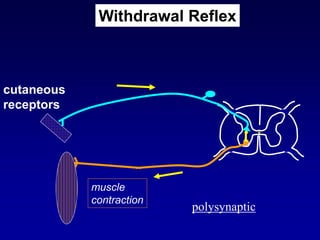
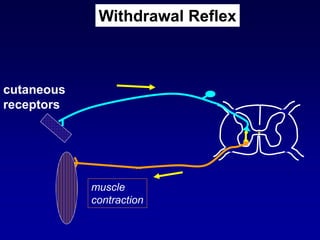
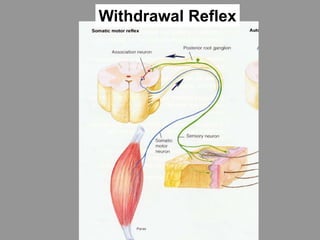
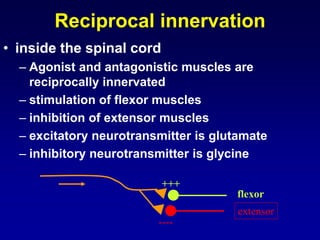
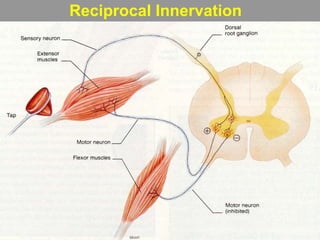
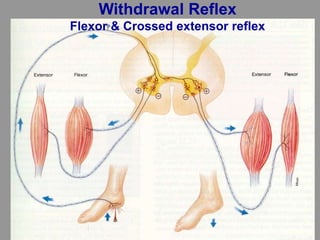
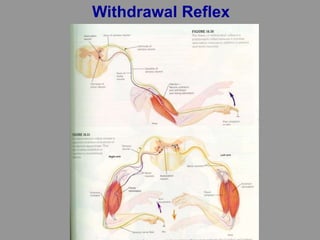
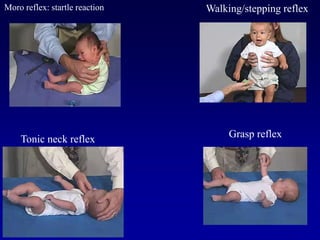
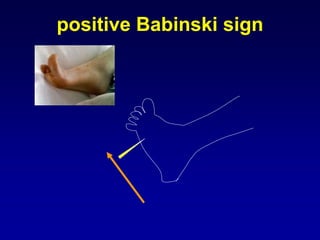
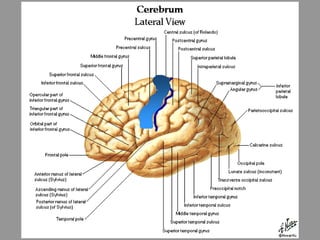
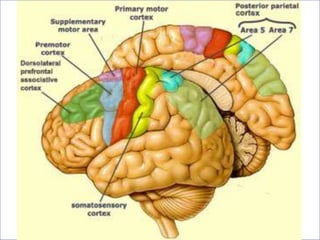
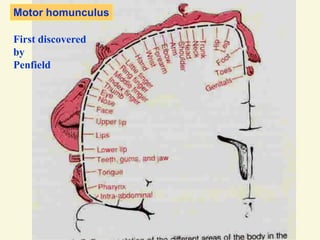
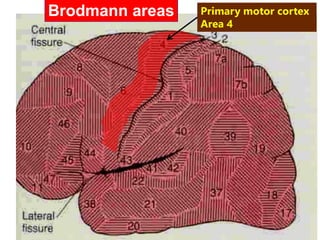
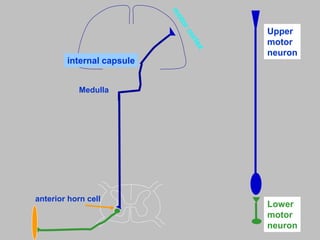
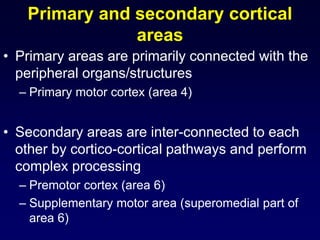
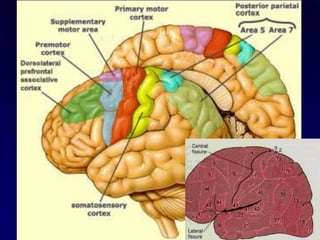
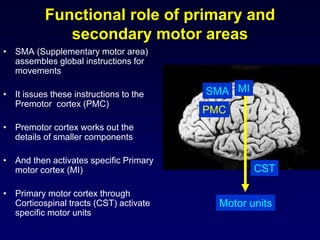
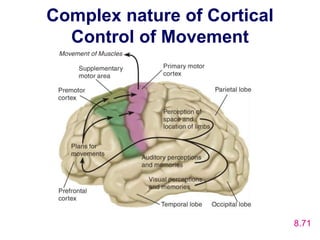
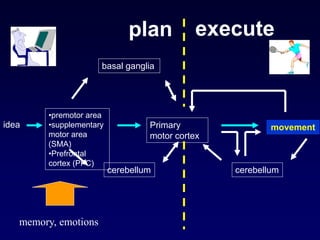
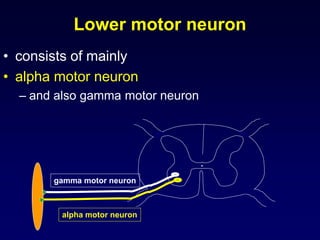
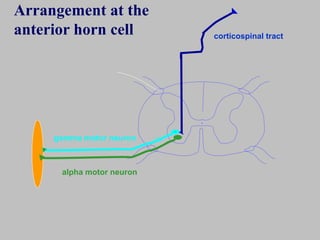
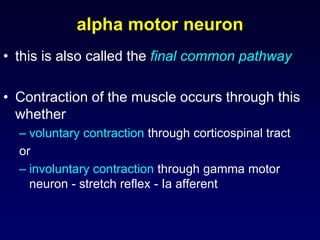
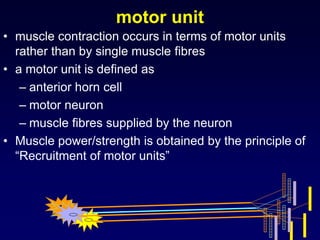
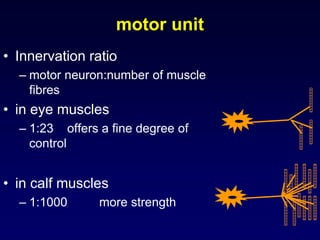
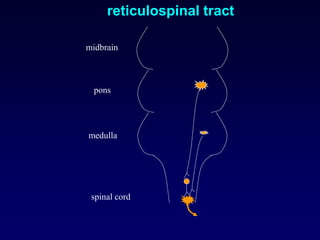
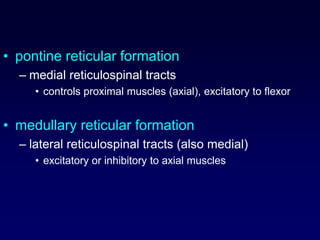
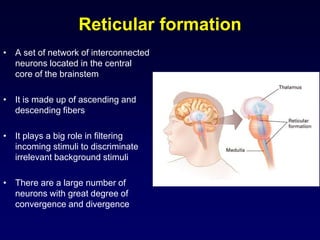
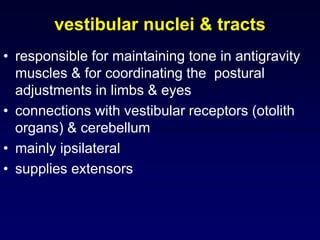
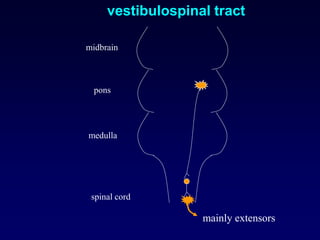
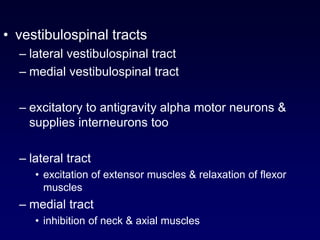
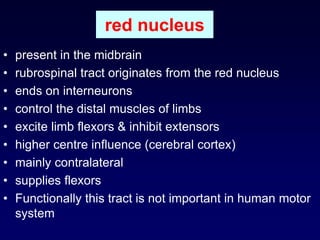
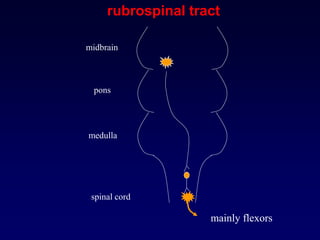
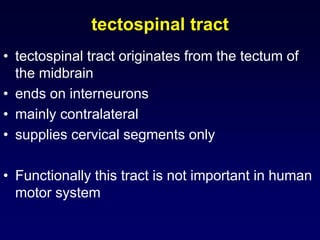
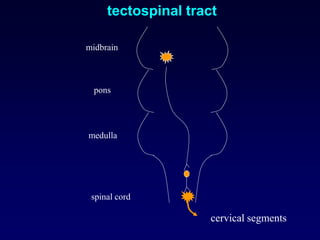
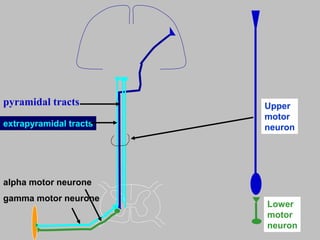
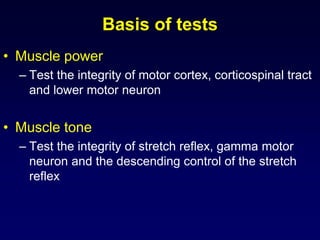
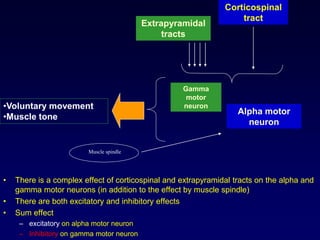
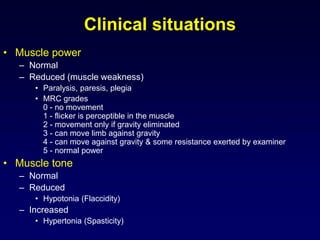
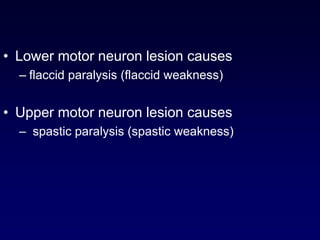
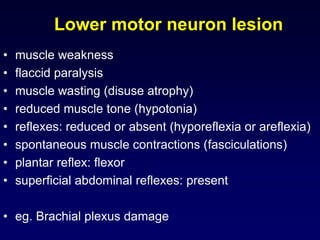
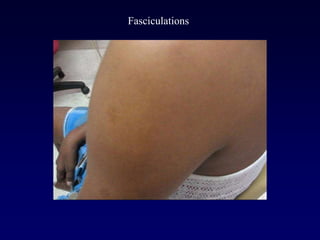
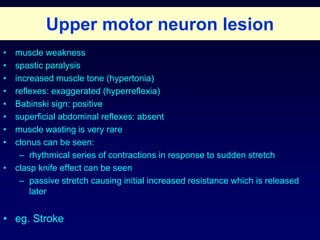
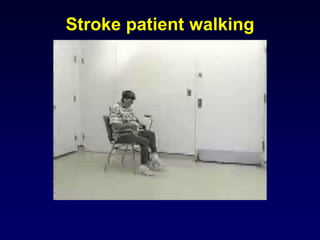
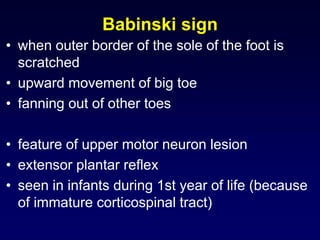
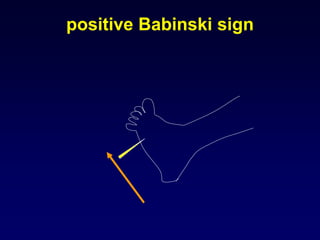
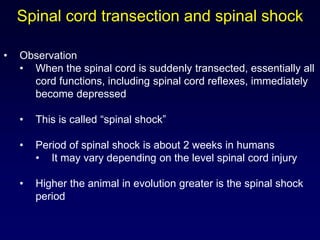
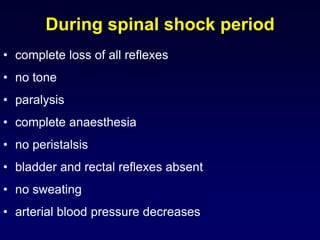
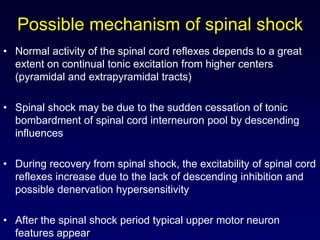
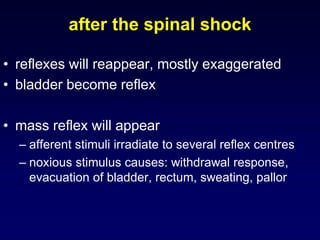
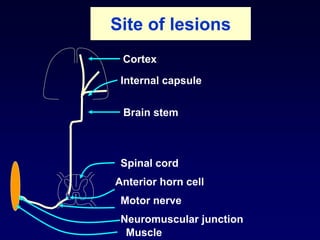
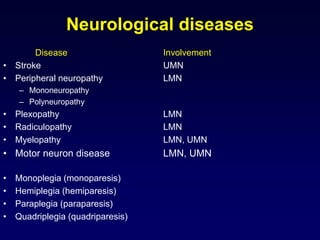
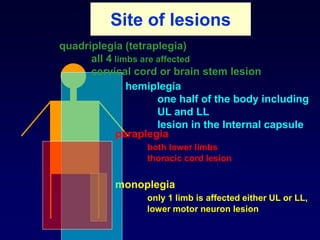
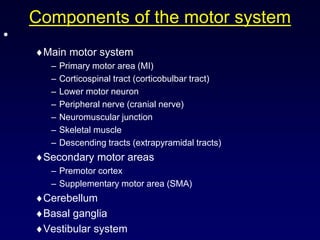
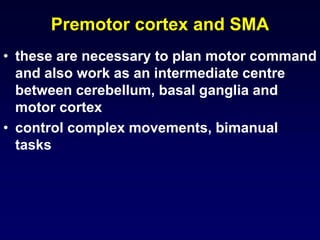
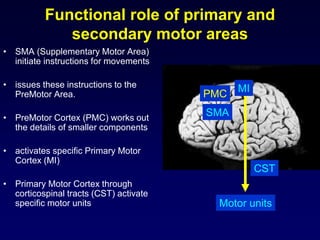
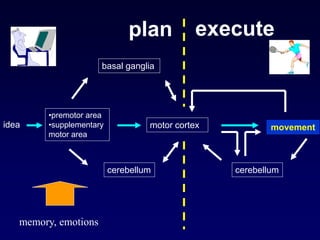
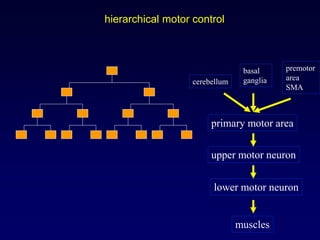
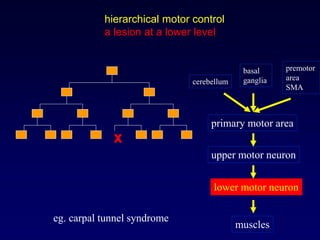
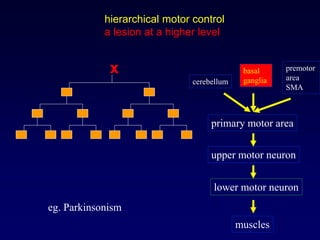
The document summarizes the motor system, including voluntary and involuntary motor functions. It describes various reflexes like the stretch reflex and their components. The motor cortex and corticospinal tract are discussed. The role of upper motor neurons, lower motor neurons, and extrapyramidal tracts in motor control is explained. Various tests to examine the motor system are also mentioned.