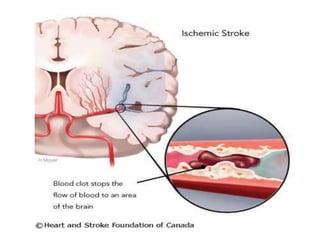
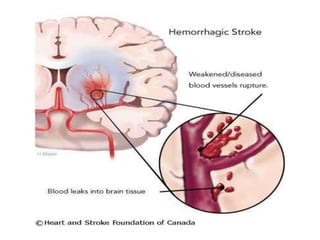
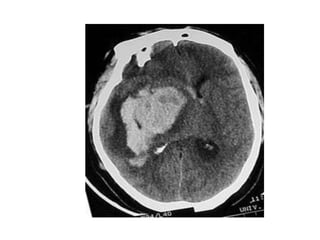
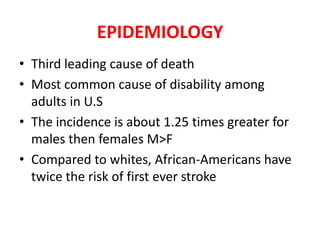
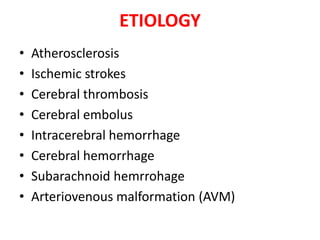
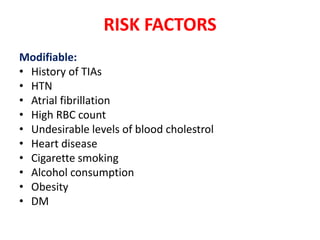
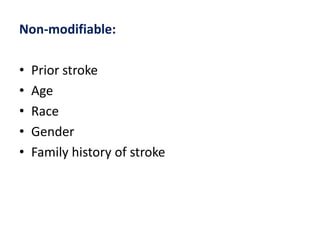
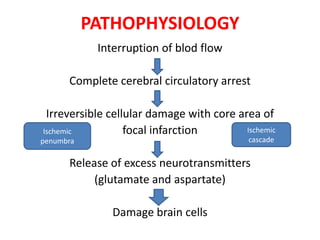
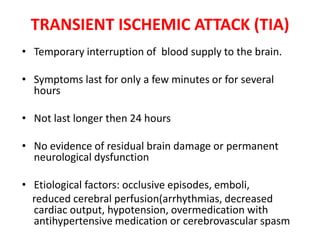
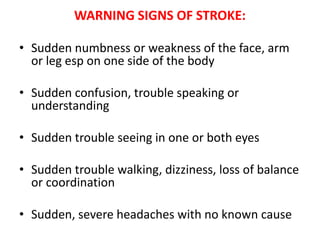
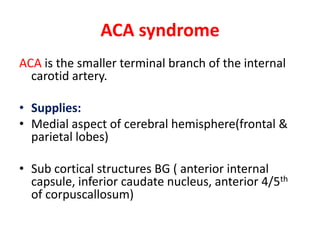
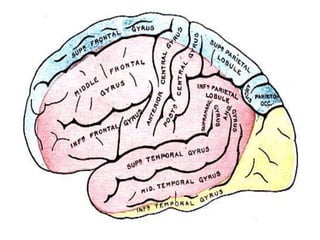
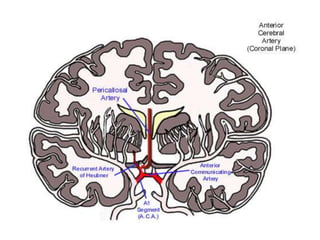
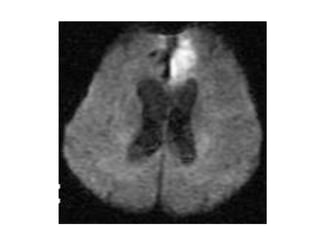
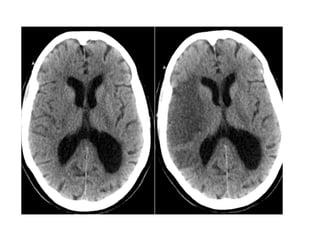
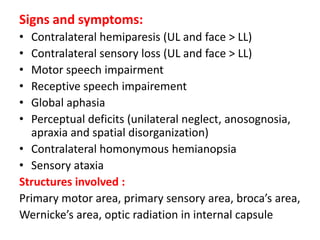
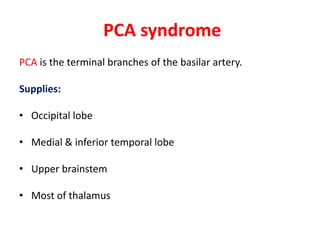
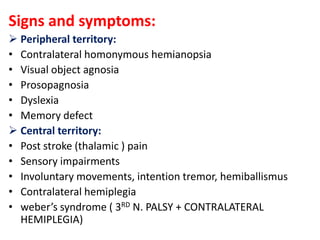
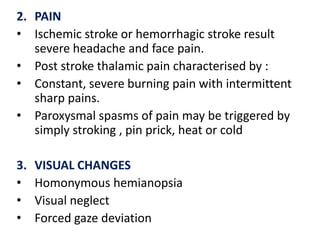
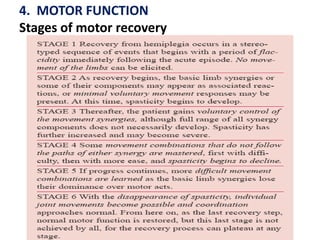
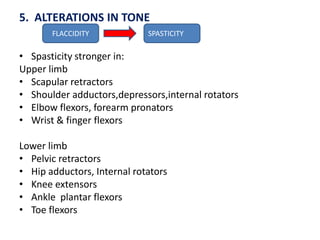
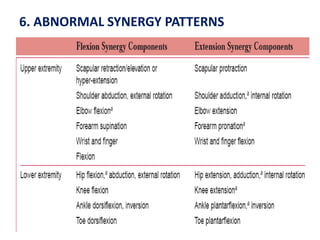
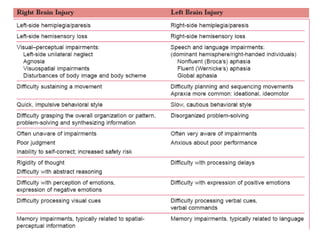
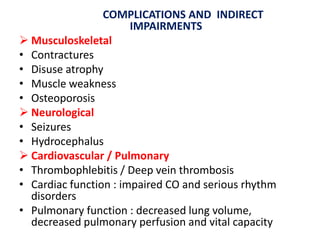
This document defines stroke as the sudden loss of neurological function caused by an interruption of blood flow to the brain. It classifies strokes as either ischemic, caused by a clot blocking blood flow, or hemorrhagic, caused by a ruptured blood vessel. Risk factors include hypertension, atrial fibrillation, and smoking. Symptoms vary depending on the affected brain region but may include weakness, sensory changes, speech problems, and visual issues. Complications can include muscle contractures, seizures, and cardiac or pulmonary issues.