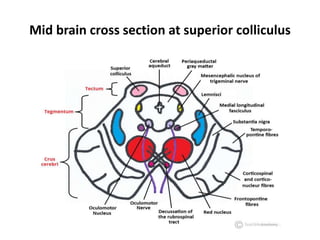
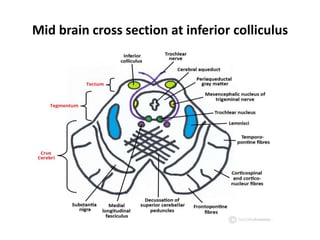
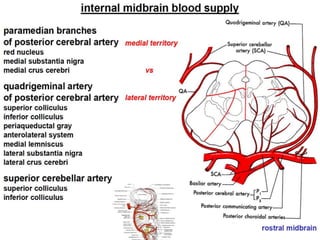
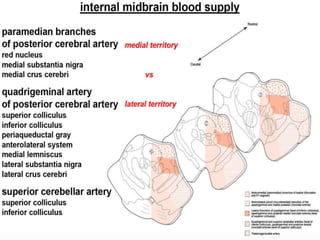
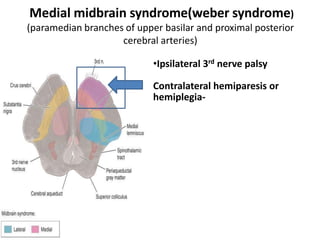
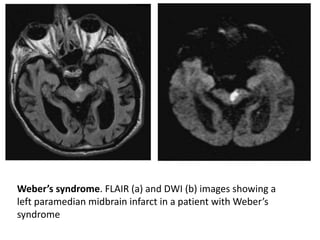
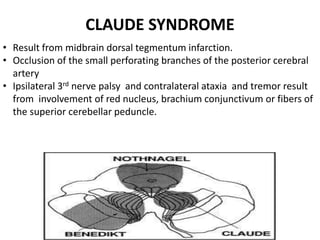
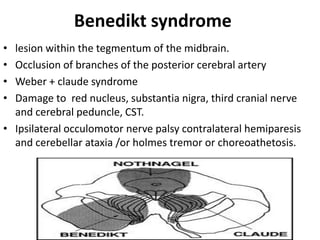
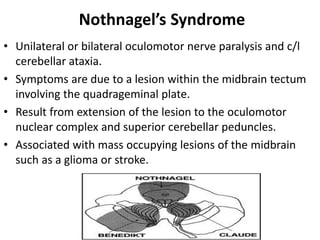
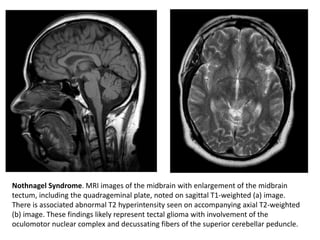
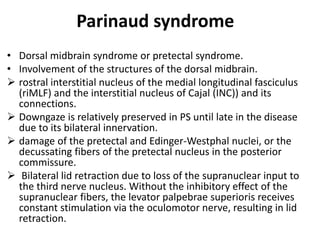
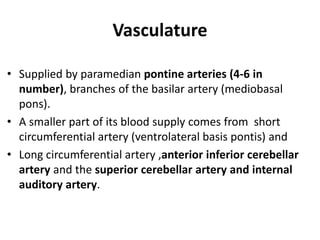
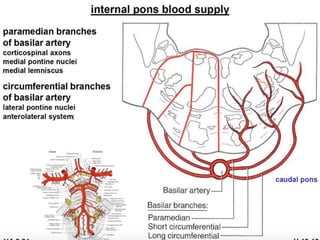
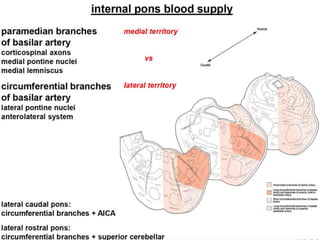
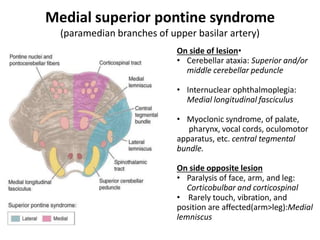
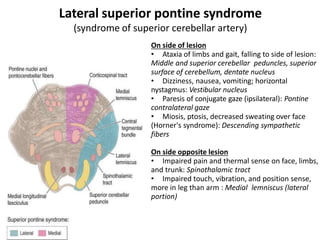
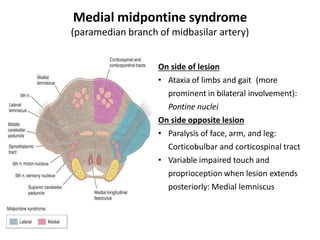
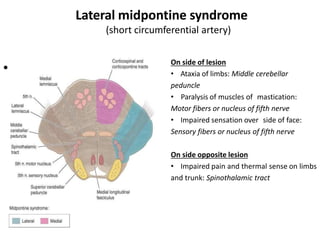
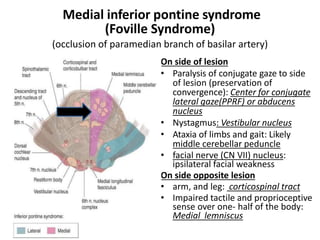
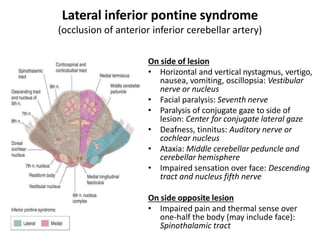
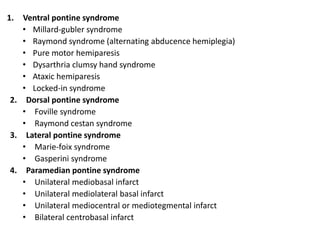
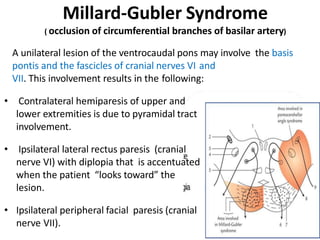
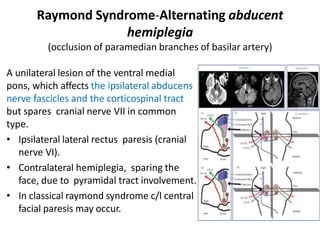
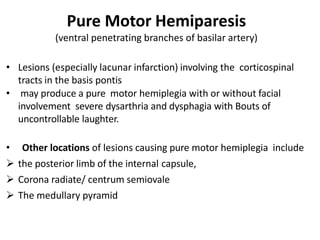
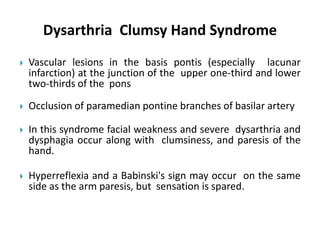
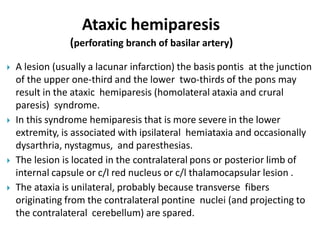
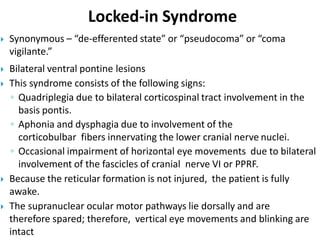
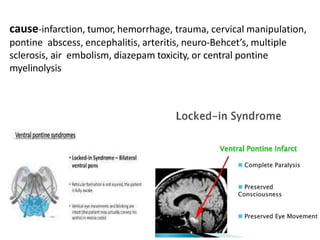
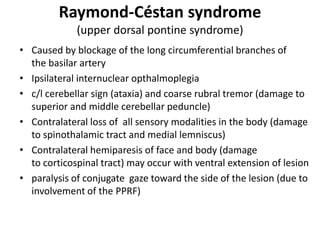
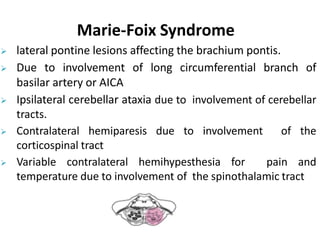
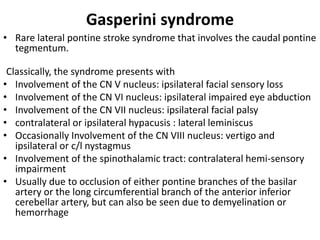
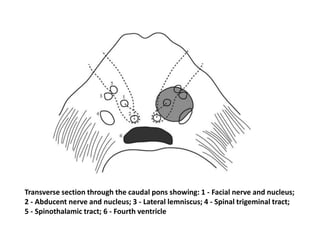
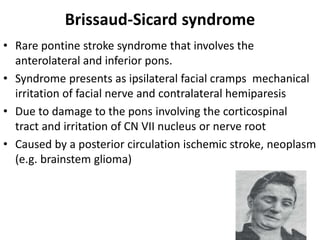
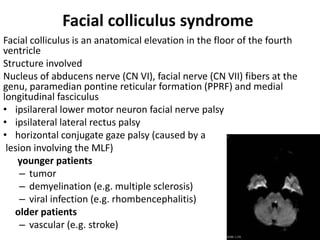
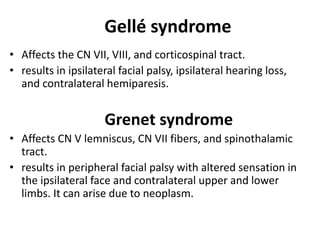
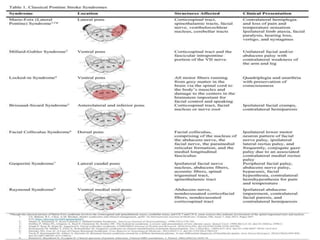
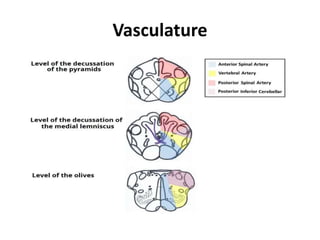
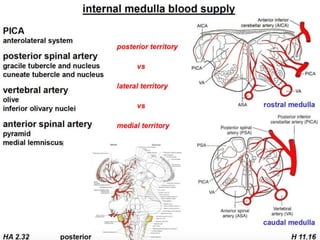
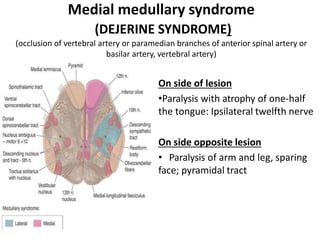
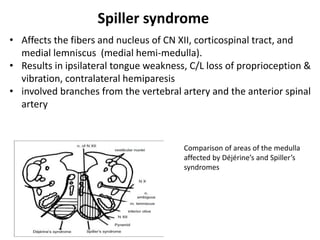
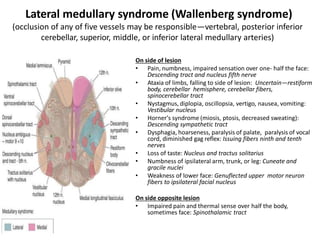
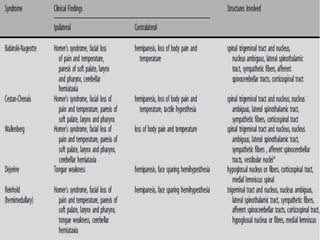
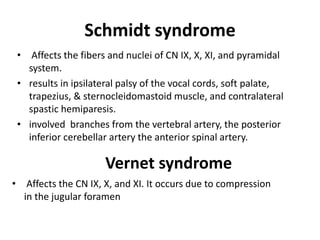
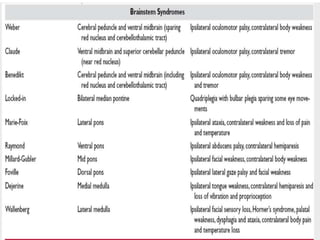
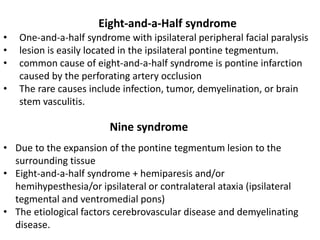
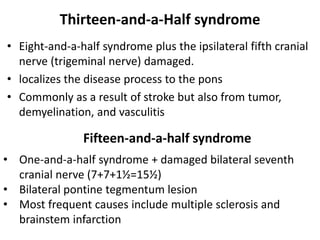
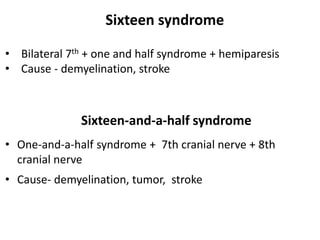
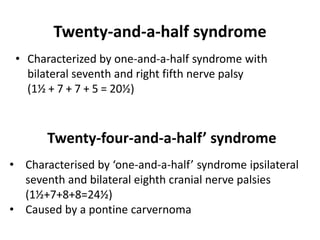
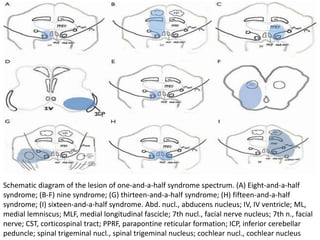
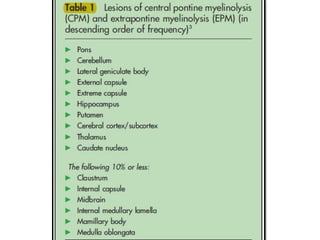
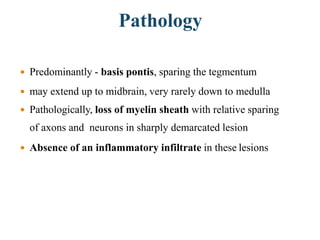
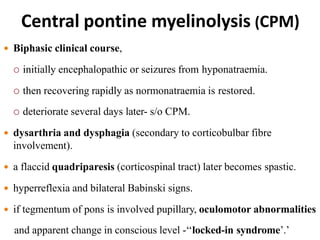
This document discusses various vascular and demyelinating syndromes of the brainstem. It describes several syndromes defined by their anatomical location in the midbrain, pons or specific vascular territories involved. These include Weber's syndrome, Claude syndrome, Benedikt syndrome, and Nothnagel's syndrome in the midbrain as well as Millard-Gubler syndrome, Raymond syndrome, lateral and medial pontine syndromes, and Locked-in syndrome in the pons. Each syndrome is characterized by the neurological deficits caused by lesions to specific brainstem structures. The vascular supply and clinical features of each syndrome are concisely outlined.