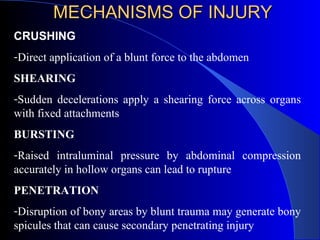
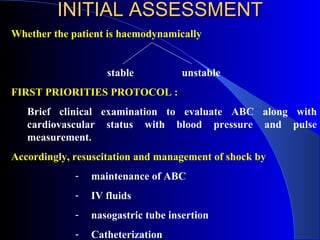
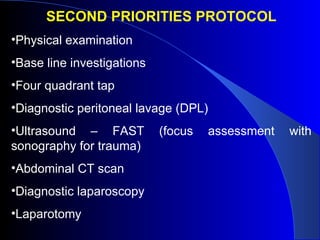
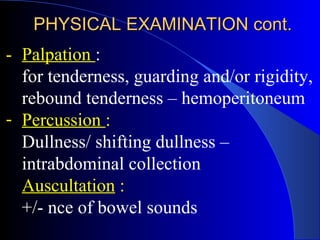
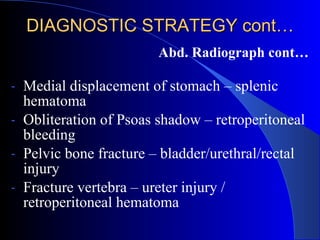
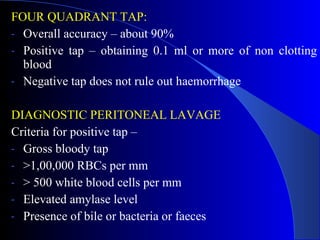
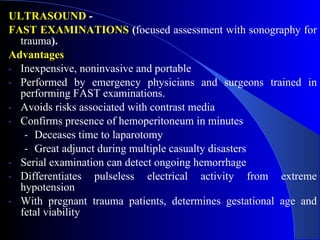
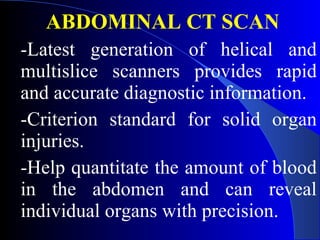
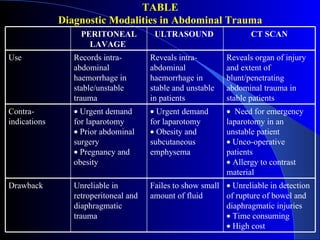
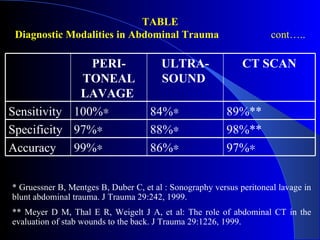
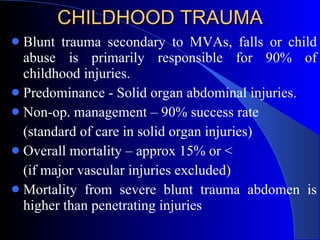
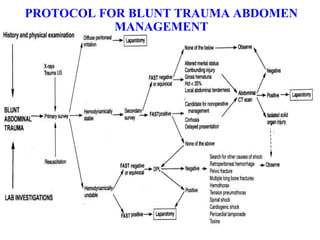
The document discusses the management of blunt abdominal trauma, emphasizing the differences between operative and conservative approaches. Key topics include mechanisms of injury, presentation variability, diagnostic strategies, and the management of solid organ injuries, particularly in children. It highlights the importance of early assessment, the role of imaging techniques, and advancements in trauma care to enhance patient outcomes.