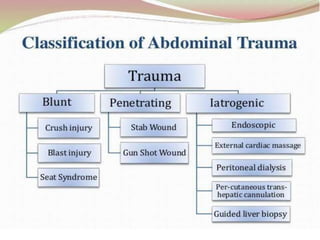
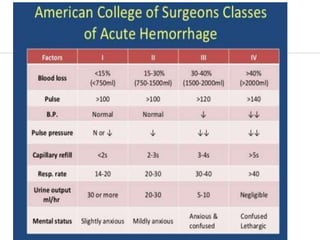
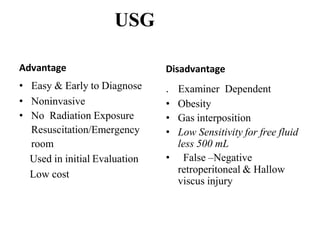
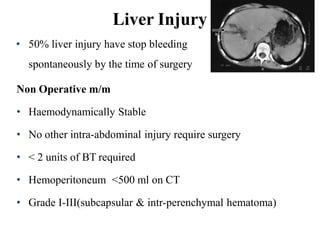
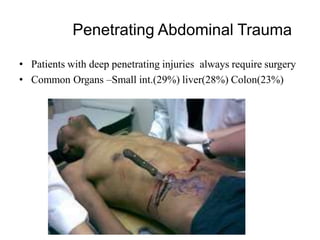
Abdominal trauma can cause serious injuries that are often difficult to diagnose. A thorough secondary survey including physical exam, lab tests, and imaging studies like FAST, CT scan, and diagnostic laparoscopy is needed to identify injuries. Common injuries include spleen laceration, liver laceration, small bowel perforation, and blunt trauma to solid organs. Management depends on injury severity but may involve conservative treatment, organ resection, or repair of damaged structures. Proper identification of intra-abdominal injuries is critical for developing an effective treatment plan.