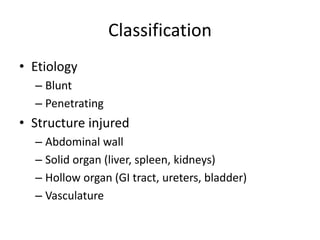
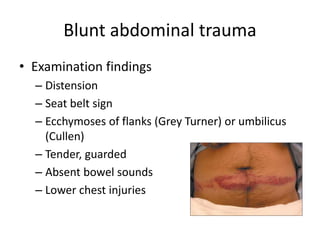
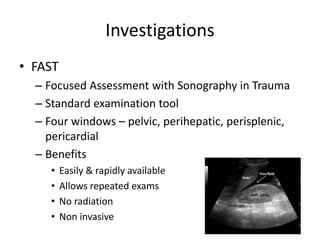
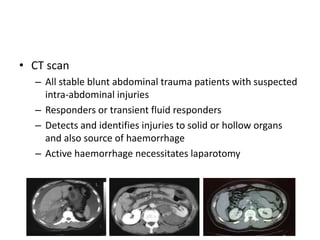
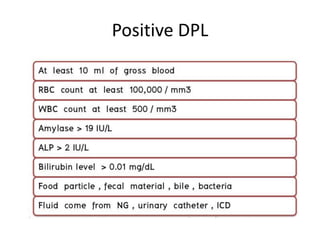
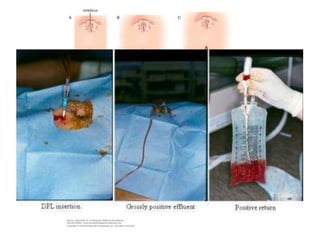
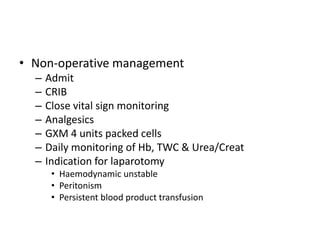
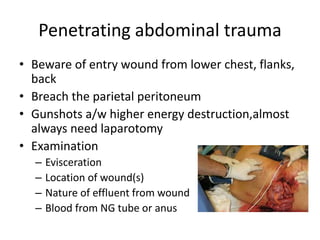
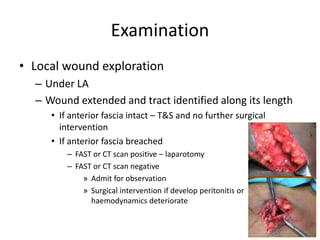
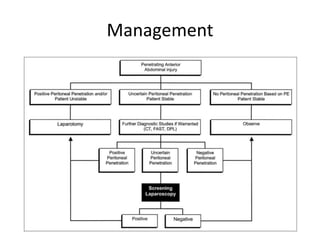
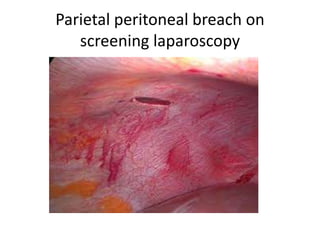
The document discusses the assessment and management of abdominal trauma, including classifications, investigations like FAST and CT scans, and management strategies for various types of injuries. It emphasizes the importance of timely surgical intervention, particularly in unstable patients, and notes that diagnostic peritoneal lavage (DPL) has largely been replaced by FAST. The document also outlines specific management protocols for both blunt and penetrating abdominal trauma, recognizing the complexity of such injuries.