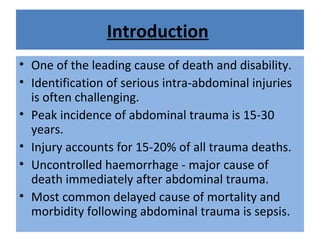
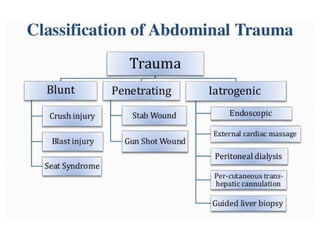
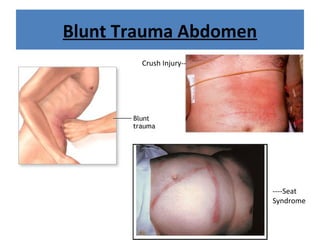
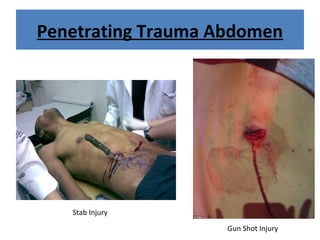
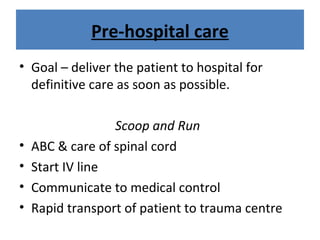
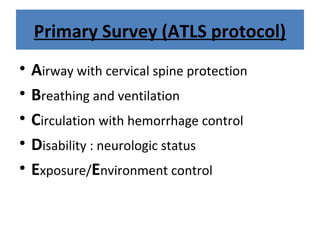
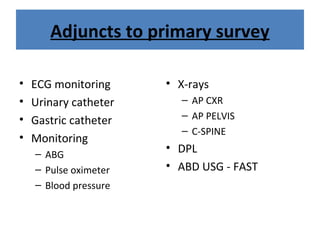
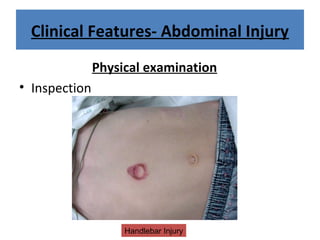
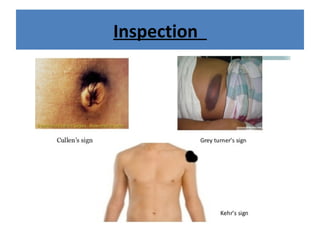
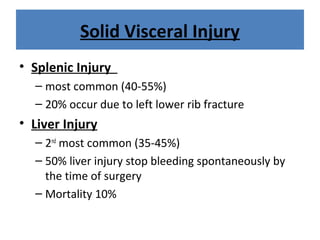
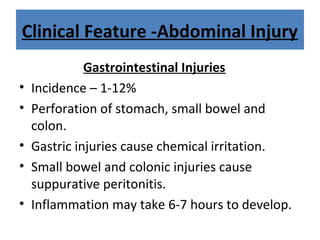
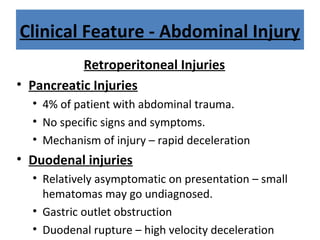
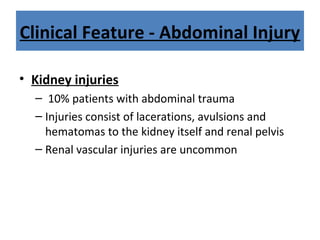
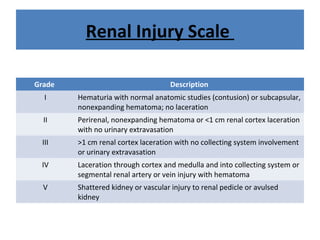
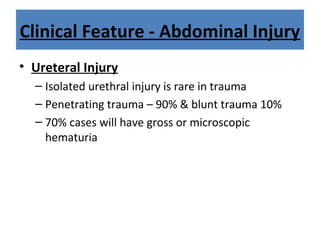
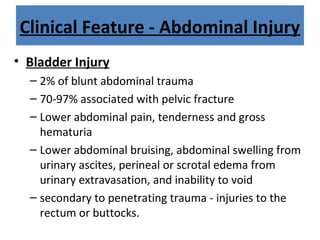
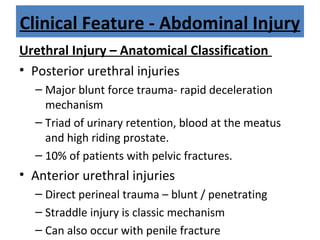
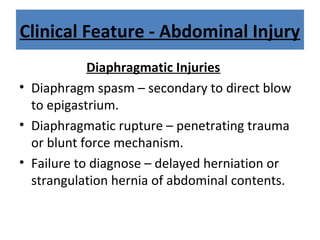
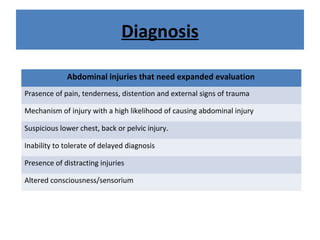
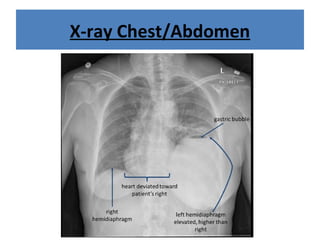
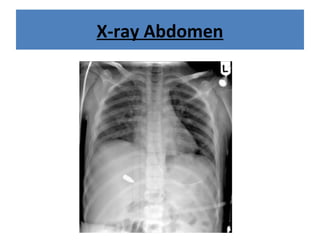
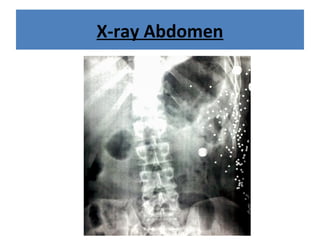
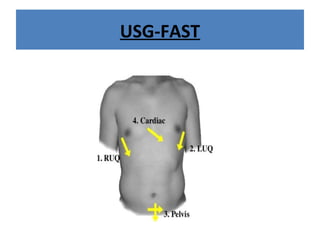
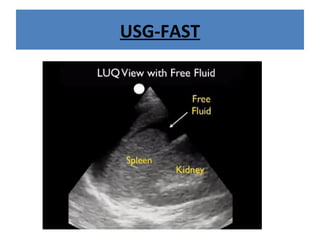
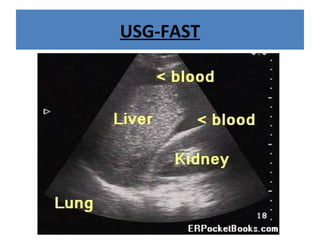
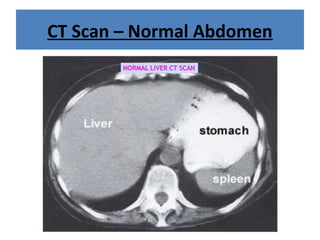
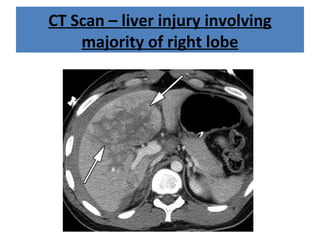
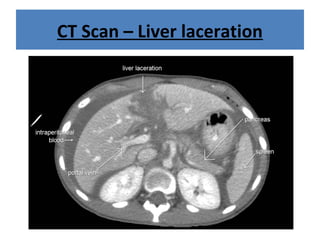
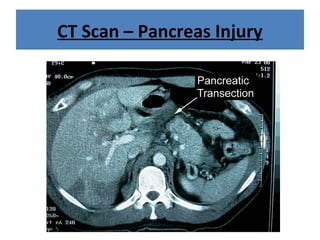
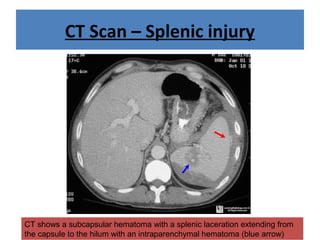
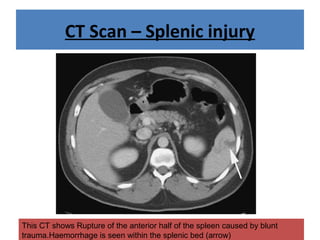
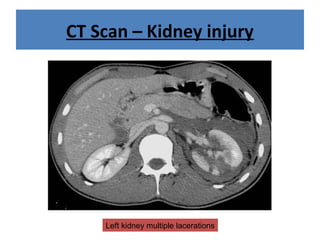
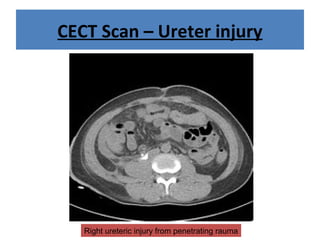
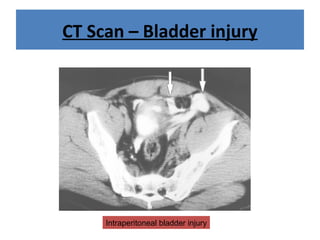
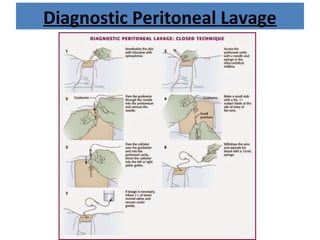
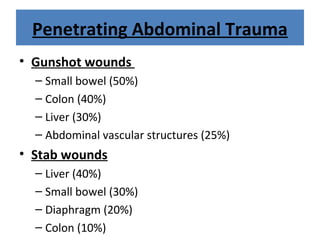
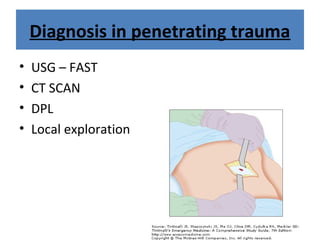
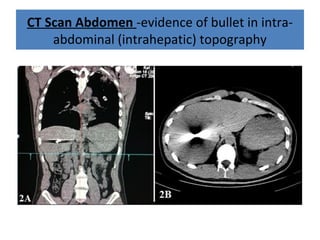
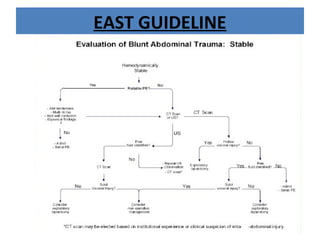
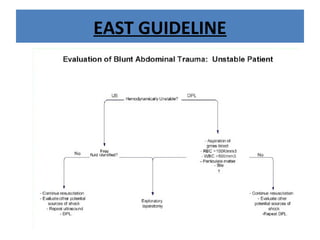
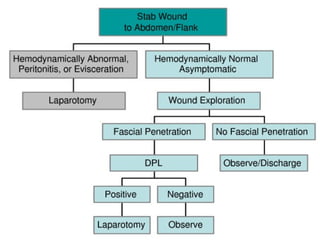
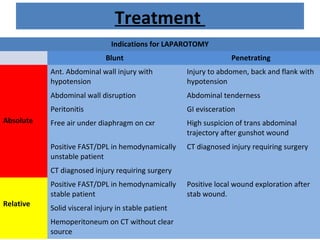
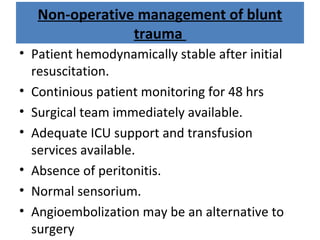
The document discusses abdominal injuries, including their causes, types, and management protocols in emergency medicine, emphasizing the importance of rapid identification and treatment to prevent complications like hemorrhage and sepsis. It outlines the procedure for pre-hospital care, primary and secondary surveys according to ATLS protocols, and detailed clinical features associated with various types of abdominal injuries. The document also covers diagnostic techniques and surgical treatment indications for penetrating and blunt abdominal trauma.