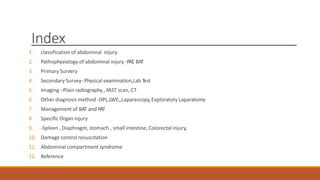
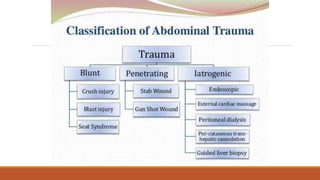
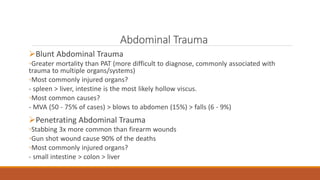
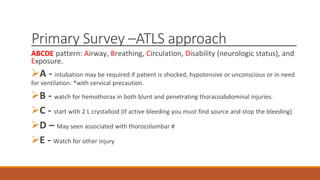
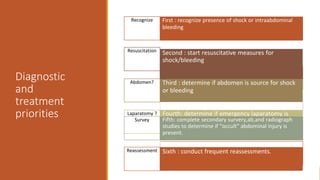
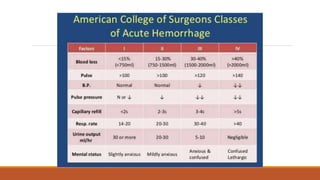
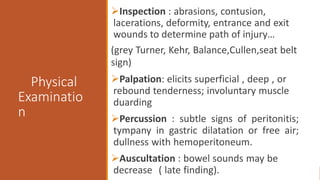
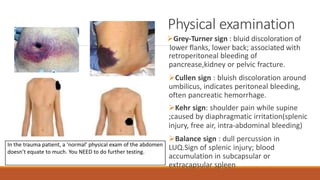
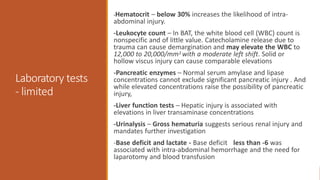
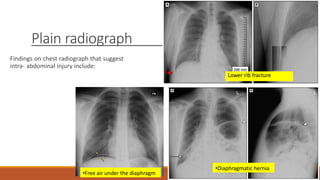
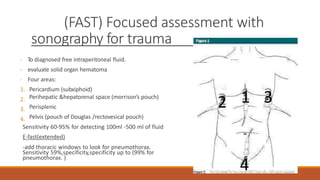
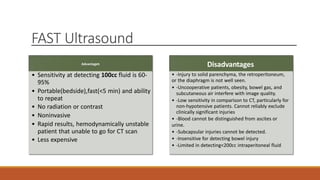
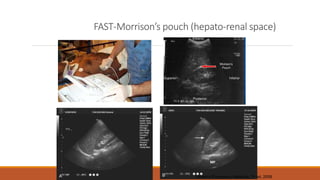
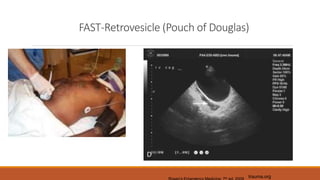
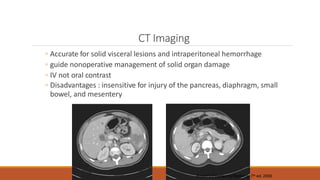
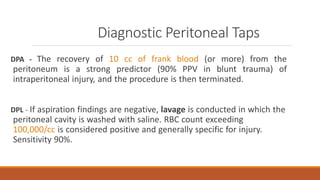
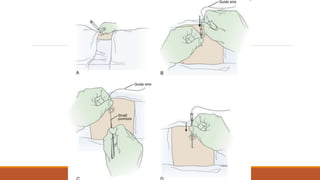
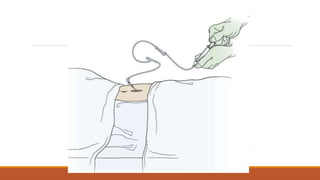
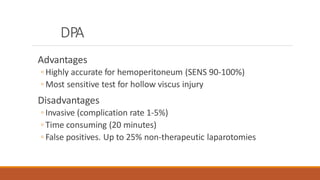
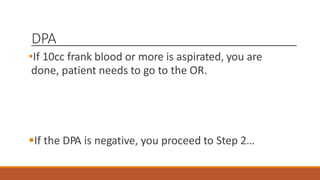
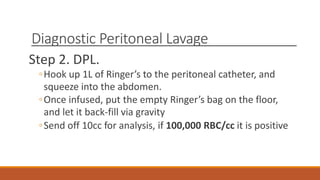
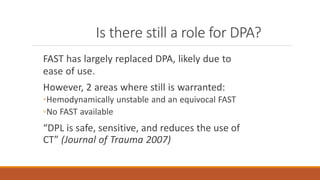
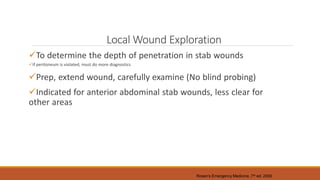
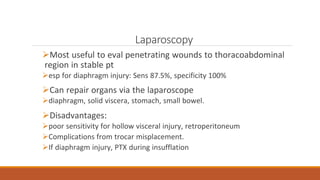
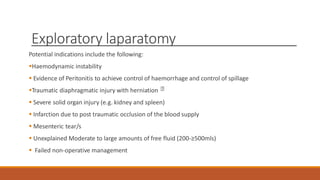
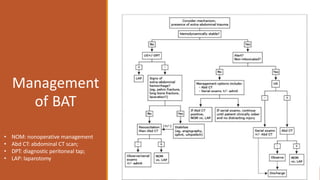
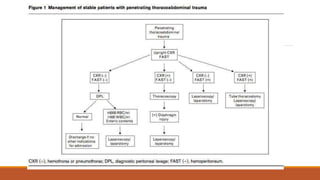
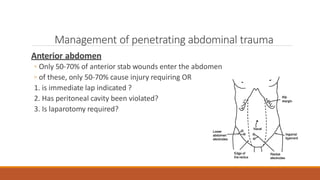
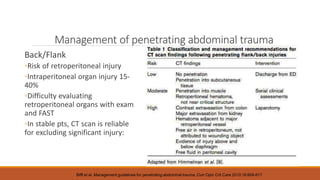
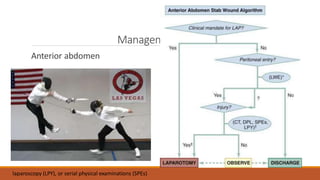
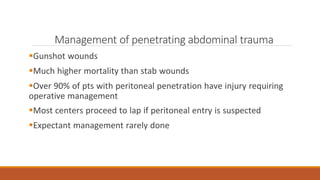
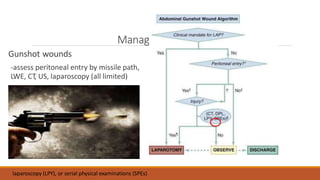
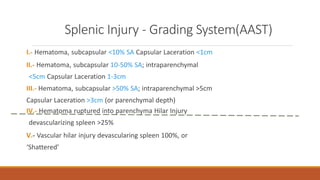
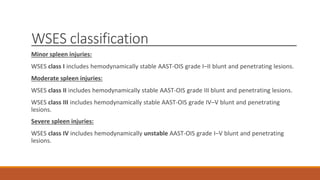
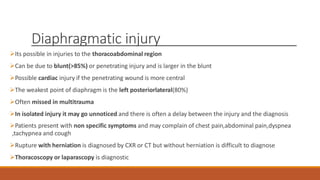
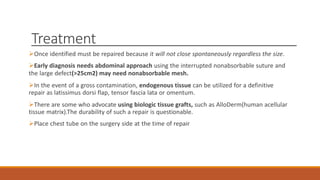
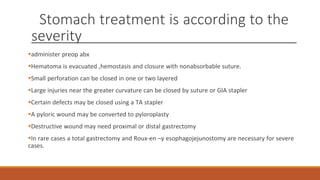
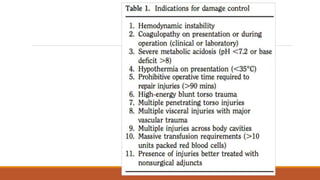
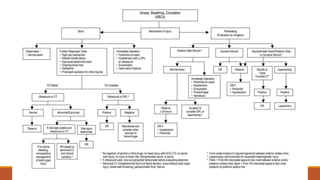
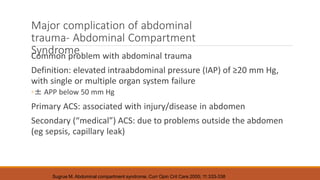
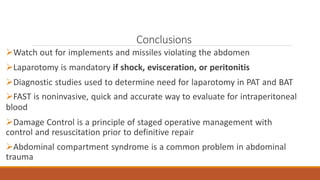
The document provides an overview of the classification, pathophysiology, diagnosis, and management of abdominal trauma. It discusses the primary and secondary surveys, various imaging modalities including FAST ultrasound, CT scan, and DPL, and treatments for different types and severities of injuries. Management may involve nonoperative approaches like observation for mild injuries or surgery for more severe injuries, hemorrhage, or failed nonoperative management. Specific injuries to organs like the spleen are also addressed.