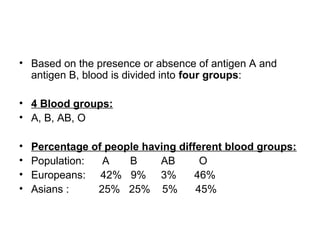
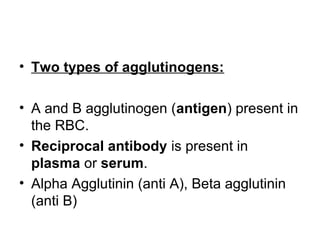
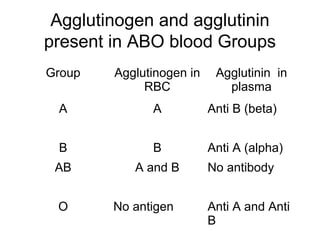
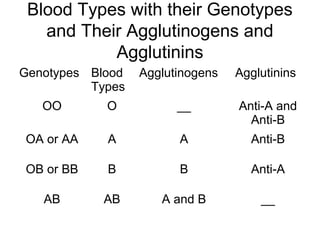
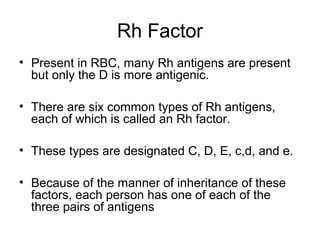
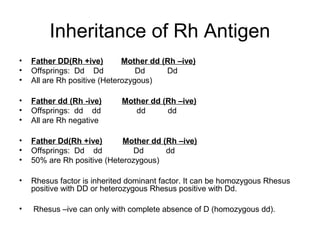
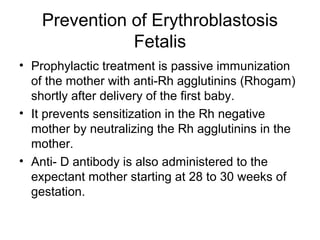
The document outlines the ABO blood grouping system, detailing the presence of agglutinogens A and B in red blood cells and the corresponding agglutinins in plasma that determine blood types A, B, AB, and O. It also discusses the inheritance patterns of blood group antigens and the Rh factor, explaining their clinical significance in blood transfusions and potential complications such as hemolytic reactions and erythroblastosis fetalis. Additionally, it emphasizes the importance of blood typing and cross-matching before transfusions to prevent adverse reactions.