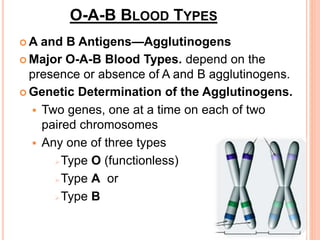
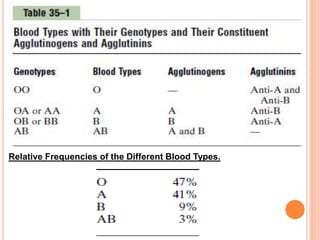
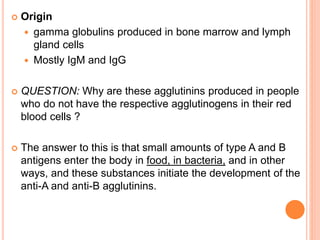
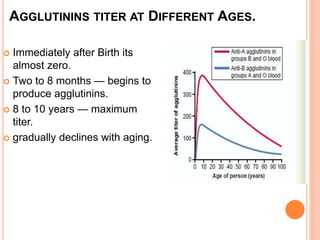
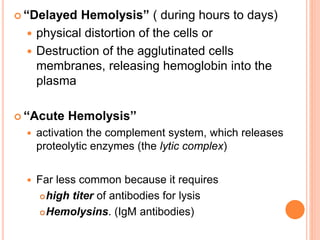
This document discusses blood types and transfusions. It explains that there are multiple blood group antigens, including the A, B, and Rh antigens. A person's blood type depends on which antigens are present on their red blood cells. Improper blood transfusions can cause agglutination and hemolysis reactions as antibodies attack mismatched antigens. The Rh system is also described, including how Rh-negative mothers can produce antibodies against a Rh-positive baby in later pregnancies, potentially causing hemolytic disease of the newborn. Prevention and treatment methods are mentioned.